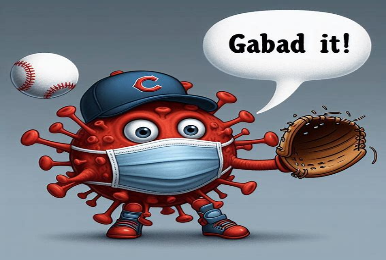
Study shows inexpensive, readily available chemical may limit impact of COVID-19
GABA reduced disease severity, lung viral load, and death in SARS-CoV-2-infected mice, By UCLA Health Preclinical studies in mice that model human COVID-19 suggest that an inexpensive, readily available amino acid…[...]
Read More