Authors: Ya-Dong Gao 1, Mei Ding 1 2, Xiang Dong 1, Jin-Jin Zhang 1, Ahmet Kursat Azkur 3, Dilek Azkur 4, Hui Gan 1, Yuan-Li Sun 1, Wei Fu 1, Wei Li 1, Hui-Ling Liang 1, Yi-Yuan Cao 5, Qi Yan 6, Can Cao 1, Hong-Yu Gao 6, Marie-Charlotte Brüggen 7 8 9, Willem van de Veen 2, Milena Sokolowska 2, Mübeccel Akdis 2, Cezmi A Akdis 2
Abstract
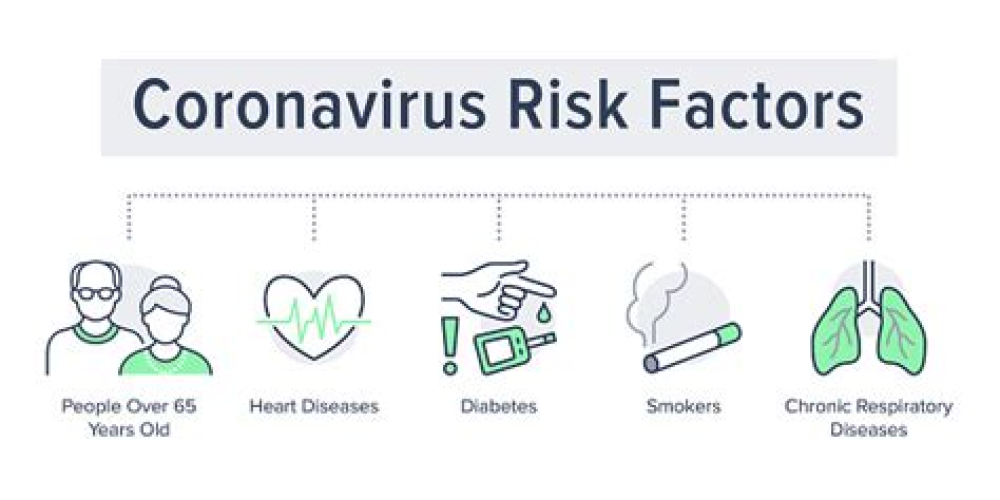
The pandemic of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused an unprecedented global social and economic impact, and high numbers of deaths. Many risk factors have been identified in the progression of COVID-19 into a severe and critical stage, including old age, male gender, underlying comorbidities such as hypertension, diabetes, obesity, chronic lung diseases, heart, liver and kidney diseases, tumors, clinically apparent immunodeficiencies, local immunodeficiencies, such as early type I interferon secretion capacity, and pregnancy. Possible complications include acute kidney injury, coagulation disorders, thromboembolism. The development of lymphopenia and eosinopenia are laboratory indicators of COVID-19. Laboratory parameters to monitor disease progression include lactate dehydrogenase, procalcitonin, high-sensitivity C-reactive protein, proinflammatory cytokines such as interleukin (IL)-6, IL-1β, Krebs von den Lungen-6 (KL-6), and ferritin. The development of a cytokine storm and extensive chest computed tomography imaging patterns are indicators of a severe disease. In addition, socioeconomic status, diet, lifestyle, geographical differences, ethnicity, exposed viral load, day of initiation of treatment, and quality of health care have been reported to influence individual outcomes. In this review, we highlight the scientific evidence on the risk factors of severity of COVID-19.
For More Information: https://pubmed.ncbi.nlm.nih.gov/33185910/