Authors: Reiterer M, Rajan M, Gómez-Banoy N, Lau JD, Gomez-Escobar LG, Gilani A, Alvarez-Mulett S, Sholle ET, Chandar V, Bram Y, Hoffman K, Rubio-Navarro A, Uhl S, Shukla AP, Goyal P, tenOever BR, Alonso LC, Schwartz RE, Schenck EJ, Safford MM
Abstract
COVID-19 has proven to be a metabolic disease resulting in adverse outcomes in individuals with diabetes or obesity. Patients infected with SARS-CoV-2 and hyperglycemia suffer from longer hospital stays, higher risk of developing acute respiratory distress syndrome (ARDS), and increased mortality compared to those who do not develop hyperglycemia. Nevertheless, the pathophysiological mechanism(s) of hyperglycemia in COVID-19 remains poorly characterized. Here we show that insulin resistance rather than pancreatic beta cell failure is the prevalent cause of hyperglycemia in COVID-19 patients with ARDS, independent of glucocorticoid treatment. A screen of protein hormones that regulate glucose homeostasis reveals that the insulin sensitizing adipokine adiponectin is reduced in hyperglycemic COVID-19 patients. Hamsters infected with SARS-CoV-2 also have diminished expression of adiponectin. Together these data suggest that adipose tissue dysfunction may be a driver of insulin resistance and adverse outcomes in acute COVID-19.
The deadly COVID-19 pandemic is underscored by the high morbidity and mortality rates seen in certain vulnerable populations, including patients with diabetes mellitus (DM), obesity, cardiovascular disease, and advanced age, with the latter associated with many chronic cardiometabolic diseases 1–4 . Hyperglycemia with or without a history of DM is a strong predictor of in-hospital adverse outcomes, portending a 7-fold higher mortality compared to patients with well-controlled blood glucose levels 5 . Hyperglycemia may be seen as a biomarker that predicts poor prognosis. A retrospective study that compared hyperglycemic patients that were treated with insulin against those who were not showed increased mortality in those receiving insulin 6 . However, it remains unclear whether insulin treatment is a surrogate for increased hyperglycemia and overall morbidity, or whether it is an actual causative factor for death. There is thus uncertainty regarding specific treatments for hyperglycemia in acute COVID-19 7 .
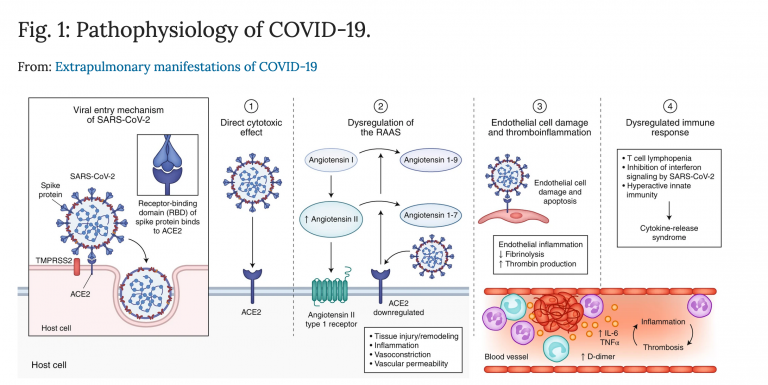
Despite our early recognition of the association between hyperglycemia and perilous outcomes, the pathophysiological mechanisms that underlie hyperglycemia in COVID-19 remain undefined 8,9 . Hypotheses have included a broad range of pathologies from direct infection of islets leading to beta cell failure (BCF) and to inflammation and glucocorticoids leading to insulin resistance (IR). Although COVID-19 is primarily a respiratory tract infection, SARS-CoV-2 is known to infect other cell types and often leads to extrapulmonary consequences 10,11 . ACE2 and other entry receptors for SARS-CoV-2 can be expressed on pancreatic islet cells and endocrine cells differentiated from human pluripotent stem cells are permissive to infection 12 . Early reports of unexpected diabetic ketoacidosis (DKA) in COVID-19 patients fuelled concerns for a novel form of acute onset beta cell failure. For example, one case described a patient with new onset diabetic ketoacidosis (DKA) who was found to be autoantibody negative for type 1 DM (T1DM) but showed evidence of prior SARS-CoV-2 infection based on serology results, suggesting the possibility of pancreatic beta cell dysfunction or destruction as a result of COVID-19 13 . However, given the high rates of COVID-19 during this pandemic coupled with low background rates of new onset T1DM, the connection between these two events in this case could be “true, true, and unrelated.” Recent studies disagree on whether ACE2 is expressed on pancreatic beta cells or whether the SARS-CoV-2 virus is found in pancreatic beta cells of deceased individuals with COVID-19 14–16 . Conversely, the well-known connection between obesity and insulin resistance might lead to impaired immunity and more severe SARS-CoV-2 infection 17 . In fact, population level studies have reported higher risk of complications in obese patients with COVID-19 18–20 . Viral infection may lead to systemic insulin resistance and worsened hyperglycemia. In sum, despite much attention, the pathophysiology of hyperglycemia in COVID-19 remains unknown.
Dexamethasone substantially reduces mortality in patients with severe COVID-19 infection requiring oxygen or invasive mechanical ventilation 21 . Glucocorticoids can also provoke hyperglycemia by inducing insulin resistance and beta cell dysfunction. The widespread usage of dexamethasone in severe SARS-CoV-2 infection is sure to exacerbate both the incidence and severity of hyperglycemia in COVID-19.
For More Information: https://europepmc.org/article/PPR/PPR303316