- What is SARS-CoV-2 and COVID-19?
- What do we know about the effects of SARS-CoV-2 and COVID-19 on the nervous system?
- What are the immediate (acute) effects of SARS-CoV-2/COVID-19 on the brain?
- What is the typical recovery from COVID-19?
- What are possible long-term neurological complications of COVID-19?
- How do the long-term effects of SARS-CoV-2 infection/COVID-19 relate to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)?
- Am I at higher risk if I currently have a neurological disorder?
- Can COVID-19 cause other neurological disorders?
- Does the COVID-19 vaccine cause neurological problems?
What is SARS-CoV-2 and COVID-19?
Coronaviruses are common causes of usually mild to moderate upper respiratory tract illnesses like the common cold, with symptoms that may include runny nose, fever, sore throat, cough, or a general feeling of being ill. However, a new coronavirus called Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) emerged and spread to cause the COVID-19 pandemic.
COVID-19, which means Coronavirus disease 2019, is an infectious disease that can affect people of all ages in many ways. It is most dangerous when the virus spreads from the upper respiratory tract into the lungs to cause viral pneumonia and lung damage leading to Acute Respiratory Distress Syndrome (ARDS). When severe, this impairs the body’s ability to maintain critical levels of oxygen in the blood stream—which can cause multiple body systems to fail and can be fatal.
What do we know about the effects of SARS-CoV-2 and COVID-19 on the nervous system?
Much of the research to date has focused on the acute infection and saving lives. These strategies have included preventing infection with vaccines, treating COVID-19 symptoms with medicines or antibodies, and reducing complications in infected individuals.
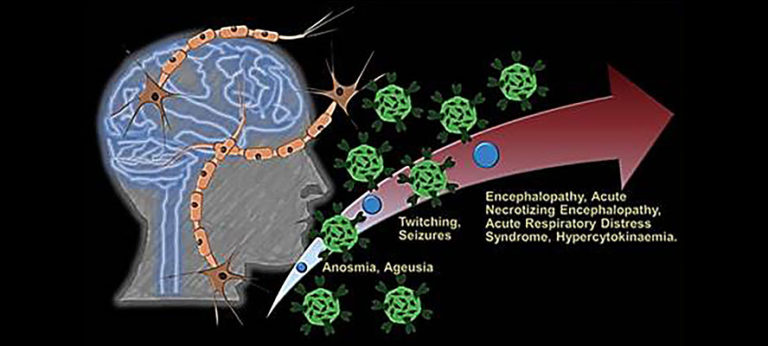
Research shows the many neurological symptoms of COVID-19 are likely a result of the body’s widespread immune response to infection rather than the virus directly infecting the brain or nervous system. In some people, the SARS-CoV-2 infection causes an overreactive response of the immune system which can also damage body systems. Changes in the immune system have been seen in studies of the cerebrospinal fluid, which bathes the brain, in people who have been infected by SARS-CoV-2. This includes the presence of antibodies—proteins made by the immune system to fight the virus—that may also react with the nervous system. Although still under intense investigation, there is no evidence of widespread viral infection in the brain. Scientists are still learning how the virus affects the brain and other organs in the long-term. Research is just beginning to focus on the role of autoimmune reactions and other changes that cause the set of symptoms that some people experience after their initial recovery. It is unknown if injury to the nervous system or other body organs cause lingering effects that will resolve over time, or whether COVID-19 infection sets up a more persistent or even chronic disorder.
What are the immediate (acute) effects of SARS-CoV-2 and COVID-19 on the brain?
Most people infected with SARS-CoV-2 virus will have no or mild to moderate symptoms associated with the brain or nervous system. However, most individuals hospitalized due to the virus do have symptoms related to the brain or nervous system, most commonly including muscle aches, headaches, dizziness, and altered taste and smell. Some people with COVID-19 either initially have, or develop in the hospital, a dramatic state of confusion called delirium. Although rare, COVID-19 can cause seizures or major strokes. Muscular weakness, nerve injury, and pain syndromes are common in people who require intensive care during infections. There are also very rare reports of conditions that develop after SARS-CoV-2 infection, as they sometimes do with other types of infections. These disorders of inflammation in the nervous system include Guillain-Barré syndrome (which affects nerves), transverse myelitis (which affects the spinal cord), and acute necrotizing leukoencephalopathy (which affects the brain).
Bleeding in the brain, weakened blood vessels, and blood clots in acute infection
The SARS-CoV-2 virus attaches to a specific molecule (called a receptor) on the surface of cells in the body. This molecule is concentrated in the lung cells but is also present on certain cells that line blood vessels in the body. The infection causes some arteries and veins—including those in the brain—to become thin, weaken, and leak. Breaks in small blood vessels have caused bleeding in the brain (so-called microbleeds) in some people with COVID-19 infection. Studies in people who have died due to COVID-19 infection show leaky blood vessels in different areas of the brain that allow water and a host of other molecules as well as blood cells that are normally excluded from the brain to move from the blood stream into the brain. This leak, as well as the resulting inflammation around blood vessels, can cause multiple small areas of damage. COVID-19 also causes blood cells to clump and form clots in arteries and veins throughout the body. These blockages reduce or block the flow of blood, oxygen, and nutrients that cells need to function and can lead to a stroke or heart attack.
A stroke is a sudden interruption of continuous blood flow to the brain. A stroke occurs either when a blood vessel in the brain becomes blocked or narrowed or when a blood vessel bursts and spills blood into the brain. Strokes can damage brain cells and cause permanent disability. The blood clots and vascular (relating to the veins, capillaries, and arteries in the body) damage from COVID-19 can cause strokes even in young healthy adults who do not have the common risk factors for stroke.
COVID-19 can cause blood clots in other parts of the body, too. A blood clot in or near the heart can cause a heart attack. A heart attack orInflammation in the heart, called myocarditis, can causeheart failure, and reduce the flow of blood to other parts of the body. A blood clot in the lungs can impair breathing and cause pain. Blood clots also can damage the kidneys and other organs.
Low levels of oxygen in the body (called hypoxia) can permanently damage the brain and other vital organs in the body. Some hospitalized individuals require artificial ventilation on respirators. To avoid chest movements that oppose use of the ventilator it may be necessary to temporarily “paralyze” the person and use anesthetic drugs to put the individual to sleep. Some individuals with severe hypoxia require artificial means of bringing oxygen into their blood stream, a technique called extra corporeal membrane oxygenation (ECMO). Hypoxia combined with these intensive care unit measure generally cause cognitive disorders that show slow recovery.
Diagnostic imaging of some people who have had COVID-19 show changes in the brain’s white matter that contains the long nerve fibers, or “wires,” over which information flows from one brain region to another. These changes may be due to a lack of oxygen in the brain, the inflammatory immune system response to the virus, injury to blood vessels, or leaky blood vessels. This “diffuse white matter disease” might contribute to cognitive difficulties in people with COVID-19. Diffuse white matter disease is not uncommon in individuals requiring intensive hospital care but it not clear if it also occurs in those with mild to moderate severity of COVID-19 illness.
For More Information: https://www.ninds.nih.gov/Current-Research/Coronavirus-and-NINDS/nervous-system