Authors: Steven R Feldman, MD, PhD, Esther E Freeman, MD, PhD Literature review current through: Jul 2021. | This topic last updated: Apr 06, 2021.
INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), raises many critical issues in dermatology and dermatologic care. Addressing these issues is necessary, yet also challenging, because there are few direct data on which to base recommendations [1].
This topic will discuss issues related to dermatologic care during the COVID-19 pandemic. Other relevant aspects of SARS-CoV-2 infection and patient management are discussed in detail separately.
●(See “COVID-19: Epidemiology, virology, and prevention”.)
●(See “COVID-19: Clinical features”.)
●(See “COVID-19: Diagnosis”.)
●(See “COVID-19: Infection control for persons with SARS-CoV-2 infection”.)
●(See “COVID-19: Outpatient evaluation and management of acute illness in adults”.)
●(See “COVID-19: Hypercoagulability”.)
●(See “COVID-19: Management in hospitalized adults”.)
●(See “COVID-19: Questions and answers”.)
●(See “COVID-19: Care of adult patients with systemic rheumatic disease”.)
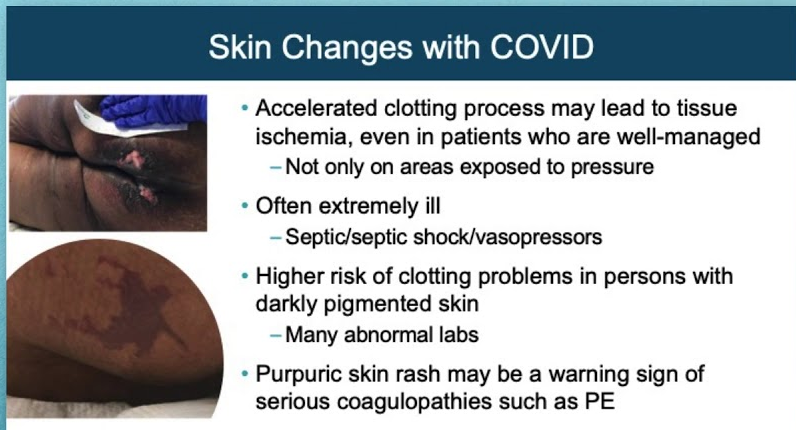
CUTANEOUS MANIFESTATIONS OF COVID-19
Case series from around the world have identified a range of potential dermatologic manifestations of coronavirus disease 2019 (COVID-19) [2-5]. The frequency (ranging from 0.2 to 20.4 percent of cases) and timing of cutaneous manifestations of COVID-19 are difficult to ascertain [6-8]. Also unclear is the association of certain skin manifestations with the illness severity [9]. Moreover, it cannot be excluded that in some patients the observed skin findings may represent cutaneous reactions to the numerous treatments used for COVID-19 [9,10].
The American Academy of Dermatology’s COVID-19 Registry, a collaboration between the American Academy of Dermatology and the International League of Dermatologic Societies, is attempting to collate cases and better define the cutaneous manifestations of COVID-19 [11] (see ‘Registries’ below). Among 171 laboratory-confirmed COVID-19 patients with cutaneous manifestations from the registry, the most commonly reported were morbilliform rash (22 percent), pernio-like acral lesions (18 percent), urticaria (16 percent), macular erythema (13 percent), vesicular eruption (11 percent), papulosquamous eruption (9.9 percent), and retiform purpura (6.4 percent) [12]. Fever and cough were reported in approximately 60 percent of cases:
●Exanthematous (morbilliform) rash – In several case series, a morbilliform rash predominantly involving the trunk has been reported as the most common cutaneous manifestation of COVID-19 [2,3,7,12-14]. The rash has been noted either at the disease onset or, more frequently, after hospital discharge or recovery [7].
●Pernio (chilblain)-like acral lesions – Pernio (chilblain)-like lesions of acral surfaces (“COVID toes”) present as erythematous-violaceous or purpuric macules on fingers, elbows, toes, and the lateral aspect of the feet, with or without accompanying edema and pruritus (picture 1A-B). They have been described across the age spectrum in patients with confirmed or suspected COVID-19, in the absence of cold exposure or underlying conditions associated with pernio [2-4,12,15-22].
Resolution may occur in two to eight weeks. A prolonged course of more than 60 days has been reported in some patients with pernio (“long haulers”) [23].
The development of pernio-like lesions in COVID-19 may be associated with a relatively mild COVID-19 disease course [2,4,24]. In the American Academy of Dermatology/International League of Dermatologic Societies registry study, 55 percent of patients overall were otherwise asymptomatic. Ninety-eight percent of patients in the study were treated in the outpatient setting alone; this finding held true when restricted to laboratory-confirmed cases only, with 78 percent remaining in the outpatient setting [4].
Our understanding of the pathogenesis of these lesions is still under evolution, though it appears to be a primarily inflammatory process with histopathologic and direct immunofluorescence findings similar to those seen in idiopathic and autoimmune-related pernio [3,18,20,25-28]. (See “Pernio (chilblains)”.)
A French study demonstrated increased in vitro production of interferon-alpha from stimulated peripheral blood T cells in patients with pernio compared with patients with polymerase chain reaction (PCR)-positive, moderate to severe COVID-19 [29]. The histologic and biologic patterns of these patients with pernio were similar to a type I interferonopathy, suggesting that a robust, innate immune response may lead to rapid control of the virus in these patients and could, at least in part, explain the relatively mild disease course and low level of antibody production.
Pernio-like lesions may represent a postviral or delayed-onset process, with 80 out of 318 cases in the American Academy of Dermatology/International League of Dermatologic Societies registry developing lesions after the onset of other COVID-19 symptoms [4]. This finding is similar to data from Spain, where 42 out of 71 patients developed lesions after other symptoms [2].
There are several case reports and case series of patients with pernio-like lesions testing positive for immunoglobulin M (IgM), immunoglobulin G (IgG), or immunoglobulin A (IgA) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and negative for PCR, possibly indicating a later stage in the disease process [4,24,30]. However, pernio-like lesions can, in some cases, appear while patients are still PCR positive for the virus, which has potential implications for infectivity and viral spread [4,22]:
•In a French, prospective study, 40 consecutive patients with chilblain-like lesions (median age 22 years, range 12 to 67) were tested for SARS-CoV-2 RNA with reverse transcription (RT)-PCR and SARS-CoV-2-specific IgA, IgM, and IgG antibodies with enzyme-linked immunosorbent assays (ELISAs) [24]. None of these patients were PCR positive at the time of dermatologic consultation; 12 (30 percent) had positive serology for antibodies, of whom seven had only IgA. Twenty-five patients (63 percent) were asymptomatic, and the remaining had only mild symptoms.
•In another French series of 311 patients (median age 26 years) with acral manifestations seen between March and May 2020, 150 (49 with symptoms suspicious for COVID-19) underwent nasopharyngeal swab RT-PCR and/or serology for SARS-CoV-2 [31]. Five of 75 patients were positive for SARS-CoV-2 serology, and 7 of 121 patients were positive for SARS-CoV-2 RT-PCR. Overall, 10 of 170 patients (7 percent) had confirmed COVID-19.
•In the American Academy of Dermatology/International League of Dermatologic Societies registry study, of 318 cases from eight countries, 14 of these cases were PCR positive.
•In an Italian study that screened 22 patients presenting with pernio-like lesions, 6 (26 percent) were PCR positive for SARS-CoV-2 [22].
Although the finding of PCR positivity is not universal and not all observed cases of pernio during the COVID-19 epidemic are necessarily related to COVID-19, it may be prudent that patients presenting with new-onset, pernio-like lesions that have no other clear cause be tested for SARS-CoV-2 PCR within seven days of the onset of pernio lesions [32-35]. For patients who have had these lesions for >4 weeks, IgM and IgG antibody testing may be appropriate, following local guidelines and depending on the quality of available tests, acknowledging that many of these patients may only make transient antibody responses or IgA responses that are not currently being tested in commercial laboratories. Work-up of other causes of pernio is discussed in greater detail separately [2,4,24]. (See “Pernio (chilblains)”.)
There are no treatment guidelines for COVID-19-associated, pernio-like lesions of the feet or hands. However, high-potency topical corticosteroids may be helpful if the lesions are causing discomfort.
Some patients have been noted to have “long COVID”/long-hauler COVID toes [23]. Additionally, some patients have been found to have recurrent pernio after initial SARS-CoV-2 infection, which may be triggered by cold [36].
For More Information: https://www.uptodate.com/contents/covid-19-cutaneous-manifestations-and-issues-related-to-dermatologic-care#!