What is SARS-CoV-2 and COVID-19?
National Institute of Neurological Disorders and Stroke
Coronaviruses are common causes of usually mild to moderate upper respiratory tract illnesses like the common cold, with symptoms that may include runny nose, fever, sore throat, cough, or a general feeling of being ill. However, a new coronavirus called Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) emerged and spread to cause the COVID-19 pandemic.
COVID-19, which means Coronavirus disease 2019, is an infectious disease that can affect people of all ages in many ways. It is most dangerous when the virus spreads from the upper respiratory tract into the lungs to cause viral pneumonia and lung damage leading to Acute Respiratory Distress Syndrome (ARDS). When severe, this impairs the body’s ability to maintain critical levels of oxygen in the blood stream—which can cause multiple body systems to fail and can be fatal.
What do we know about the effects of SARS-CoV-2 and COVID-19 on the nervous system?
Much of the research to date has focused on the acute infection and saving lives. These strategies have included preventing infection with vaccines, treating COVID-19 symptoms with medicines or antibodies, and reducing complications in infected individuals.
Research shows the many neurological symptoms of COVID-19 are likely a result of the body’s widespread immune response to infection rather than the virus directly infecting the brain or nervous system. In some people, the SARS-CoV-2 infection causes an overreactive response of the immune system which can also damage body systems. Changes in the immune system have been seen in studies of the cerebrospinal fluid, which bathes the brain, in people who have been infected by SARS-CoV-2. This includes the presence of antibodies—proteins made by the immune system to fight the virus—that may also react with the nervous system. Although still under intense investigation, there is no evidence of widespread viral infection in the brain. Scientists are still learning how the virus affects the brain and other organs in the long-term. Research is just beginning to focus on the role of autoimmune reactions and other changes that cause the set of symptoms that some people experience after their initial recovery. It is unknown if injury to the nervous system or other body organs cause lingering effects that will resolve over time, or whether COVID-19 infection sets up a more persistent or even chronic disorder.
What are the immediate (acute) effects of SARS-CoV-2 and COVID-19 on the brain?
Most people infected with SARS-CoV-2 virus will have no or mild to moderate symptoms associated with the brain or nervous system. However, most individuals hospitalized due to the virus do have symptoms related to the brain or nervous system, most commonly including muscle aches, headaches, dizziness, and altered taste and smell. Some people with COVID-19 either initially have, or develop in the hospital, a dramatic state of confusion called delirium. Although rare, COVID-19 can cause seizures or major strokes. Muscular weakness, nerve injury, and pain syndromes are common in people who require intensive care during infections. There are also very rare reports of conditions that develop after SARS-CoV-2 infection, as they sometimes do with other types of infections. These disorders of inflammation in the nervous system include Guillain-Barré syndrome (which affects nerves), transverse myelitis (which affects the spinal cord), and acute necrotizing leukoencephalopathy (which affects the brain).
Bleeding in the brain, weakened blood vessels, and blood clots in acute infection
The SARS-CoV-2 virus attaches to a specific molecule (called a receptor) on the surface of cells in the body. This molecule is concentrated in the lung cells but is also present on certain cells that line blood vessels in the body. The infection causes some arteries and veins—including those in the brain—to become thin, weaken, and leak. Breaks in small blood vessels have caused bleeding in the brain (so-called microbleeds) in some people with COVID-19 infection. Studies in people who have died due to COVID-19 infection show leaky blood vessels in different areas of the brain that allow water and a host of other molecules as well as blood cells that are normally excluded from the brain to move from the blood stream into the brain. This leak, as well as the resulting inflammation around blood vessels, can cause multiple small areas of damage. COVID-19 also causes blood cells to clump and form clots in arteries and veins throughout the body. These blockages reduce or block the flow of blood, oxygen, and nutrients that cells need to function and can lead to a stroke or heart attack.
A stroke is a sudden interruption of continuous blood flow to the brain. A stroke occurs either when a blood vessel in the brain becomes blocked or narrowed or when a blood vessel bursts and spills blood into the brain. Strokes can damage brain cells and cause permanent disability. The blood clots and vascular (relating to the veins, capillaries, and arteries in the body) damage from COVID-19 can cause strokes even in young healthy adults who do not have the common risk factors for stroke.
COVID-19 can cause blood clots in other parts of the body, too. A blood clot in or near the heart can cause a heart attack. A heart attack or Inflammation in the heart, called myocarditis, can cause heart failure, and reduce the flow of blood to other parts of the body. A blood clot in the lungs can impair breathing and cause pain. Blood clots also can damage the kidneys and other organs.
Low levels of oxygen in the body (called hypoxia) can permanently damage the brain and other vital organs in the body. Some hospitalized individuals require artificial ventilation on respirators. To avoid chest movements that oppose use of the ventilator it may be necessary to temporarily “paralyze” the person and use anesthetic drugs to put the individual to sleep. Some individuals with severe hypoxia require artificial means of bringing oxygen into their blood stream, a technique called extra corporeal membrane oxygenation (ECMO). Hypoxia combined with these intensive care unit measure generally cause cognitive disorders that show slow recovery.
Diagnostic imaging of some people who have had COVID-19 show changes in the brain’s white matter that contains the long nerve fibers, or “wires,” over which information flows from one brain region to another. These changes may be due to a lack of oxygen in the brain, the inflammatory immune system response to the virus, injury to blood vessels, or leaky blood vessels. This “diffuse white matter disease” might contribute to cognitive difficulties in people with COVID-19. Diffuse white matter disease is not uncommon in individuals requiring intensive hospital care but it not clear if it also occurs in those with mild to moderate severity of COVID-19 illness.
What is the typical recovery from COVID-19?
Fortunately, people who have mild to moderate symptoms typically recover in a few days or weeks. However, some people who have had only mild or moderate symptoms of COVID-19 continue to experience dysfunction of body systems—particularly in the lungs but also possibly affecting the liver, kidneys, heart, skin, and brain and nervous system—months after their infection. In rare cases, some individuals may develop new symptoms (called sequelae) that stem from but were not present at the time of initial infection. People who require intensive care for Acute Respiratory Distress Syndrome, regardless of the cause, usually have a long period of recovery. Individuals with long-term effects, whether following mild or more severe COVID-19, have in some cases self-identified as having “long COVID” or “long haul COVID.” These long-term symptoms are included in the scientific term, Post Acute Sequelae of SARS-CoV-2 Infection (PASC).
What are possible long-term neurological complications of COVID-19?
Researchers are following some known acute effects of the virus to determine their relationship to the post-acute complications of COVID-19 infection. These post-acute effects usually include fatigue in combination with a series of other symptoms. These may include trouble with concentration and memory, sleep disorders, fluctuating heart rate and alternating sense of feeling hot or cold, cough, shortness of breath, problems with sleep, inability to exercise to previous normal levels, feeling sick for a day or two after exercising (post-exertional malaise), and pain in muscle, joints, and chest. It is not yet known how the infection leads to these persistent symptoms and why in some individuals and not others.
Collapse accordion content
Nerve damage, including peripheral neuropathy
Some symptoms experienced by some people weeks to months after COVID infection suggest the peripheral nervous system, the vast communication network that sends signals between the central nervous system (the brain and spinal cord) and all other parts of the body, is impaired. Peripheral nerves send many types of sensory information to the central nervous system (CNS), such as a message that the feet are cold. They also carry signals from the CNS to the rest of the body, including those that control voluntary movement. Nerve dysfunction is also a known complication in those with critical care illness such as the acute respiratory distress syndrome.
Symptoms of peripheral neuropathy vary depending on the type of nerves—motor, sensory, or autonomic—that are damaged.
- Motor nerves control the movement of all muscles under conscious control, such as those used for walking, grasping things, or talking. Damage to the motor nerves can cause muscle weakness and cramps.
- Sensory nerves carry messages from our sense of touch, sight, hearing, taste, and smell. Sensory nerves transmit information such as the feeling of a light touch, temperature, or pain. The symptoms of sensory nerve damage can include loss of sense of touch, temperature, and pain or a tingling sensation.
- Autonomic nerves control organs to regulate activities that people do not control consciously, such as breathing, digestion, and heart and gland functions. Common symptoms include excess or absence of sweating, heat intolerance, and drop in blood pressure upon standing. Postural orthostatic tachycardia syndrome (also known as POTS) can increase heart rate when standing up and cause such symptoms as lightheadedness (or fainting) or difficulty concentrating.
Fatigue and post-exertional malaise
The most common persistent symptom weeks and months after COVID-19 infection is fatigue. The fatigue is similar to what one experiences with many viral infections such as the flu. The sense of fatigue can be brought on by both physical and mental activity. Some people are unable to return to work or school after COVID-19 due to fatigue, while others find it extremely difficult to accomplish their normal level of activity. Tasks such as walking the dog or going shopping can cause extreme tiredness and fatigue; some people can’t carry out everyday activities without feeling pain or tiredness. COVID-related complications such as depressed heart, lung, or kidney function, poor sleep, or muscle deconditioning are known to cause fatigue and affect the ability to exercise. Fatigue is very common in most inflammatory conditions. The cause(s) of fatigue in many of those suffering weeks and months after COVID-19 is not known.
Post-exertional malaise (PEM) is a condition in which otherwise usual activities are followed by a period of very severe fatigue and sense of feeling sick. PEM can occur with a delay after the activity, but can last for days thereafter.
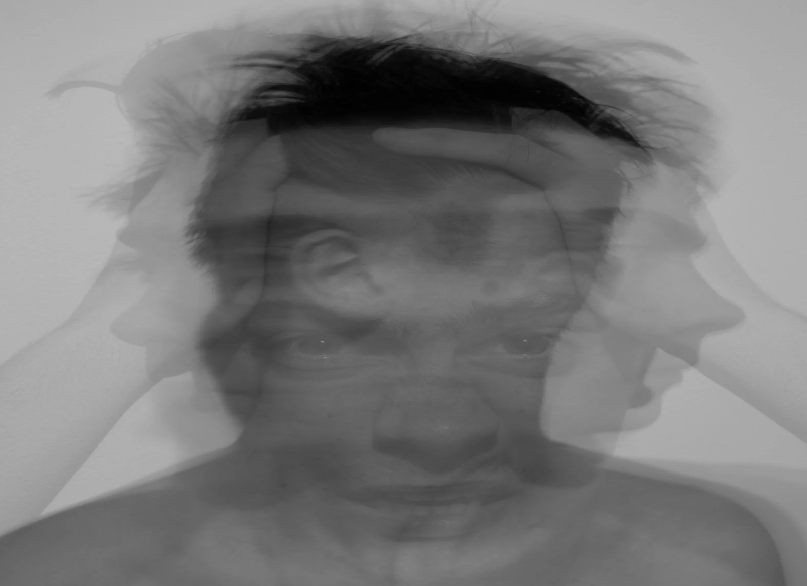
Cognitive impairment/altered mental state
People with severe acute COVID-19 illness may develop confusion, delirium, and a depressed level of consciousness. Those suffering from post-acute sequelae of COVID-19 frequently have difficulty concentrating and memory problems, sometimes called “brain fog.” This impairment is a common symptom in those with severe fatigue of any cause. A variety of immune, metabolic, or blood vessel abnormalities or drug effects can contribute to the dramatic effects on cognitive function in the acute infection. Whether these also underlie the problems experienced weeks or months after mild or moderate illness is not known.
Muscle, joint, and chest pain
Some people continue to report pain in a muscle or group of muscles (myalgia), aching joints, and fatigue after recovering from the initial course of the virus. Persistent muscle pain and chest pain is commonly reported by persons recovering from ARDS, but is now being reported by those who had a mild or moderate infectious illness. Some individuals also have a sense of shortness of breath despite testing normal on pulmonary function tests.
Prolonged/lingering loss of smell (anosmia) or taste
Some people who have had COVID-19 may lose their sense of taste or smell, or the sensation of flavor. The loss of sense of taste or smell is characteristic of COVID-19 because the SARS-CoV-2 virus infects the tissue that forms the lining in the nose. The virus has been found to target certain cells in the nose that support the nerve cells. Those nerve cells detect odors and send that information to the brain. Damage to these supporting cells can cause smell or taste loss that can continue for weeks or months as these cells repair themselves or are replaced by new cells. During the recovery period some odors may smell different—even sometimes unpleasant or foul—than people remember prior to being infected.
Persistent fevers and chills
Some people who recover from their acute (short-term) infection continue to have on-and-off fever, along with chills and body ache. Some people have a high, prolonged fever after the infection is gone, which might contribute to the sense of fatigue. In some instances, people who recover from the initial infection may have temperature dysregulation, in which it’s difficult for the body to keep a normal temperature.
Prolonged respiratory effects and lung damage
COVID-19 is primarily a respiratory disease that can seriously affect the lungs during and after the infection. Some people with the disease have breathing difficulties and some require supplemental oxygen support or mechanical ventilation via a respirator. The disease also can damage the muscles that help us breathe. Lung injury can cause low blood oxygen and brain hypoxia, which occurs when the brain isn’t getting enough oxygen. This can lead to cognitive impairment, seizures, stroke, and permanent damage to the brain and other organs. Results from several studies show that, even in people who have had mild-to-moderate infection, the effects of COVID-19 can persist in the lungs for months. Some people develop pneumonia after their acute illness has passed. Several people need pulmonary (lung) rehabilitation to rebuild their lung function. Studies show several people who had the infection, particularly those who had a more severe course of illness, also develop scarring of the lung and permanent lung dysfunction.
Headaches
Headaches are often among the many symptoms that can accompany infection from the coronavirus. Some people continue to have mild to serious headaches sometimes for weeks after recovery. The sensation of pressure is different from a migraine, which may be brought on by stress. The headaches may be infrequent or occur chronically (some people report having daily headache).
Sleep disturbances
Some people with long-term neurological effects from the SARS-CoV-2 infection report having trouble falling asleep or staying asleep (insomnia), excessive daytime sleepiness (hypersomnia), unrefreshing sleep, and changes in sleep patterns. It may be difficult for some people to wake up and fall asleep at their regular times. Depression, anxiety, and post-traumatic stress disorder (PTSD) can negatively affect sleep. Sleep disorders can contribute to fatigue and cognitive troubles. Some people report an increase in pain, headache, and stress because of lack of sleep. Continued loss of sleep also negatively affects attention and mood. For more information about COVID-19’s effect on sleep (as well as on the respiratory system) and tips to improve sleep, see the National Heart, Lung, and Blood Institute.
Anxiety, depression, and stress post-COVID
The outbreak of COVID-19 is stressful for many people. People respond to stress in different ways and it is normal to experience a range of emotions, including fear, anxiety, and grief. Being isolated from others during the infection, the real risk of death, and the stress of hospitalization and critical care can trigger post-traumatic stress disorder. In addition, given the contagious nature of COVID-19, the individual is often not the only affected person in the family or circle of friends, some of whom may even have died. Some people may develop a mood or anxiety disorder. For information on post-COVID stress and coping, see the National Institute of Mental Health’s resources at National Institute of Mental Health’s (NIMH) Director, Dr. Gordon In the News and NIMH Shareable Resources on Coping with COVID-19.
How do the long-term effects of SARS-CoV-2 infection/COVID-19 relate to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)?
Some of the symptom clusters reported by people still suffering months after their COVID-19 infection overlap with symptoms described by individuals with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). People with a diagnosis of ME/CFS have wide-ranging and debilitating effects including fatigue, PEM, unrefreshing sleep, cognitive difficulties, postural orthostatic tachycardia, and joint and muscle pain. Unfortunately, many people with ME/CFS do not return to pre-disease levels of activity. The cause of ME/CFS is unknown but many people report its onset after an infectious-like illness. Rest, conserving energy, and pacing activities are important to feeling better but don’t cure the disease. Although the long-term symptoms of COVID-19 may share features with it, ME/CFS is defined by symptom-based criteria and there are no tests that confirm an ME/CFS diagnosis.
ME/CFS is not diagnosed until the key features, especially severe fatigue, post-exertional malaise, and unrefreshing sleep, are present for greater than six months. It is now becoming more apparent that following infection with SARS-CoV-2/COVID-19, some individuals may continue to exhibit these symptoms beyond six months and qualify for an ME/CFS diagnosis. It is unknown how many people will develop ME/CFS after SARS-CoV-2 infection. It is possible that many individuals with ME/CFS, and other disorders impacting the nervous system, may benefit greatly if research on the long-term effects of COVID-19 uncovers the cause of debilitating symptoms including intense fatigue, problems with memory and concentration, and pain.
Am I at a higher risk if I currently have a neurological disorder?
Much is still unknown about the coronavirus but people having one of several underlying medical conditions may have an increased risk of illness. However, not everyone with an underlying condition will be at risk of developing severe illness. People who have a neurological disorder may want to discuss their concerns with their doctors.
Because COVID-19 is a new virus, there is little information on the risk of getting the infection in people who have a neurological disorder. People with any of these conditions might be at increased risk of severe illness from COVID-19:
- Cerebrovascular disease
- Stroke
- Obesity
- Dementia
- Diabetes
- High blood pressure
There is evidence that COVID-19 seems to disproportionately affect some racial and ethnic populations, perhaps because of higher rates of pre-existing conditions such as heart disease, diabetes, and lung disease. Social determinants of health (such as access to health care, poverty, education, ability to remain socially distant, and where people live and work) also contribute to increased health risk and outcomes.
Can COVID-19 cause other neurological disorders?
In some people, response to the coronavirus has been shown to increase the risk of stroke, dementia, muscle and nerve damage, encephalitis, and vascular disorders. Some researchers think the unbalanced immune system caused by reacting to the coronavirus may lead to autoimmune diseases, but it’s too early to tell.
Anecdotal reports of other diseases and conditions that may be triggered by the immune system response to COVID-19 include para-infectious conditions that occur within days to a few weeks after infection:
- Multi-system infammatory syndrome – which causes inflammation in the body’s blood vessels
- Transverse myelitis – an inflammation of the spinal cord
- Guillain-Barré sydrome (sometimes known as acute polyradiculoneuritis) – a rare neurological disorder which can range from brief weakness to nearly devastating paralysis, leaving the person unable to breathe independently
- Dysautonomia – dysfunction of the autonomic nerve system, which is involved with functions such a breathing, heart rate, and temperature control
- Acute disseminating encephalomyelitis (ADEM) – an attack on the protective myelin covering of nerve fibers in the brain and spinal cord
- Acute necrotizing hemorrhagic encephalopathy – a rare type of brain disease that causes lesions in certain parts of the brain and bleeding (hemorrhage) that can cause tissue death (necrosis)
- Facial nerve palsies (lack of function of a facial nerve) such as Bell’s Palsy
- Parkinson’s disease-like symptoms have been reported in a few individuals who had no family history or early signs of the disease
Does the COVID-19 vaccine cause neurological problems?
Almost everyone should get the COVID-19 vaccination. It will help protect you from getting COVID-19. The vaccines are safe and effective and cannot give you the disease. Most side effects of the vaccine may feel like flu and are temporary and go away within a day or two. The U.S. Food and Drug Administration (FDA) continues to investigate any report of adverse consequences of the vaccine. Consult your primary care doctor or specialist if you have concerns regarding any pre-existing known allergic or other severe reactions and vaccine safety.
A recent study from the United Kingdom demonstrated an increase in Guillain-Barré Syndrome related to the Astra Zeneca COVID-19 vaccine (virally delivered) but not the Moderna (messenger RNA vaccine). Guillain-Barré syndrome (a rare neurological disorder in which the body’s immune system damages nerve cells, causing muscle weakness and sometimes paralysis) has also occurred in some people who have received the Janssen COVID-19 Vaccine (also virally delivered). In most of these people, symptoms began within weeks following receipt of the vaccine. The chance of having this occur after these vaccines is very low, 5 per million vaccinated persons in the UK study. The chance of developing Guillain-Barré Syndrome was much higher if one develops COVID-19 infection (i.e., has a positive COVID test) than after receiving the Astra Zeneca vaccine. The general sense is that there are COVID-19 vaccines that are safe in individuals whose Guillain-Barré syndrome was not associated with a previous vaccination and that actual infection is the greater risk for developing Guillain-Barré Syndrome.
The U.S. Centers for Disease Control and Prevention (CDC) site offers information on vaccine resources. The National Institutes of Health (NIH) has information on vaccines for the coronavirus. The CDC has make public its report on the association of Guillain-Barré Syndrome with the Janssen COVID-19 Vaccine and no increased incidence occurred after vaccination with the Moderna or Pfizer vaccines.
For more information, visit Guillain-Barré Syndrome.
There have been reports of neurological complications from other SARS-CoV-2 vaccinations. Visit the FDA COVID-19 Vaccines webpage for information about coronavirus vaccines and fact sheets for recipients and caregivers that outline possible neurological and other risks.