ZUBEDA HAMID 15th September 2023 Delhi Print Edition
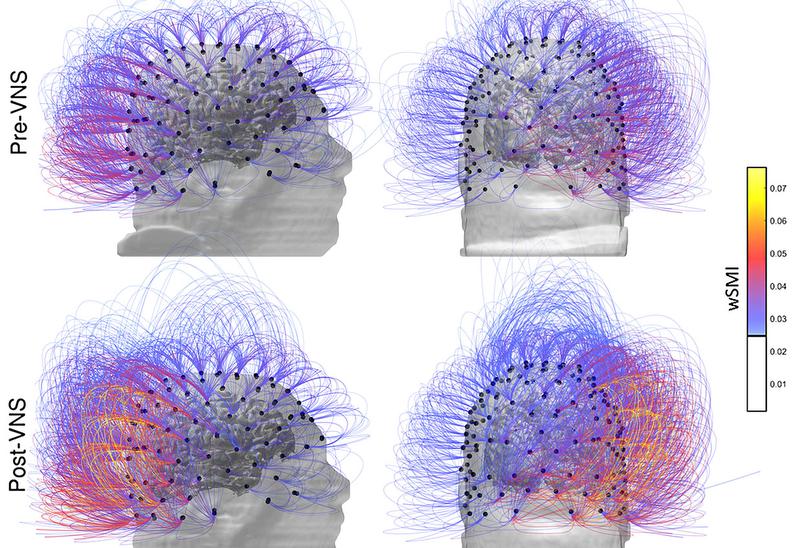
Brain activity in a patient before, top row, and after vagus nerve stimulation. Image for representational purpose only. AP
The story so far: There’s been a lot of chatter online of late, about the vagus nerve: ways to stimulate it and possible benefits of this stimulation to help with health problems from anxiety to obesity. Videos abound on stimulation, including yoga, plunging your face into cold water, alongside sales of little devices that send electrical impulses into your brain. Research has also indicated a link between vagus nerve dysfunction and long COVID.
What is the vagus nerve?
They’re actually a pair of nerves, one on each side, that run from your brainstem, through the neck, to your chest and stomach. They form a key part of the parasympathetic nervous system, the system that is responsible for relaxing and resting your body after a bout of activity and for a number of vital functions including your heart rate, blood pressure and digestion; it also plays a role in the immune system.
Why is the vagus nerve being researched?
There are many things that make the vagus nerve fascinating to researchers. The vagal nerves are the longest cranial nerves, going from your brain to your large intestine, fulfilling their meaning (‘vagus’ in Latin means ‘wandering’) by passing through, or connecting with your neck, heart, lungs, abdomen and digestive tract – all important parts. They are the 10thof your 12 cranial nerves and contain 75% of your parasympathetic nervous system’s nerve fiber. They work bi-directionally, allowing the brain and body to communicate with each other. So researchers are increasingly looking at ways through which stimulation of these nerves, our ‘sensory superhighways’, thereby triggering the parasympathetic nervous system, may potentially help with various health conditions.
What are the conditions vagus nerve stimulation can treat?
Some treatments are already in existence, for instance, an implantable vagus nerve stimulator is used to treat epilepsy and depression (that does not respond to conventional treatment), by stimulating areas of the brain that lead to seizures and affect moods. There are now non-invasive devices that can be held against the skin for stimulation. One finding about the vagus nerve was that it regulates inflammation: the body, in response to an infection, gets temporarily inflamed, but once the infection is dealt with, the vagus nerve helps bring the body back to normal by suppressing inflammation. This, researchers believe, could have implications in helping to treat several conditions.
Vagus nerve stimulation is also being studied for other diseases and disorders such as migraines, polycystic ovary syndrome, alcoholism, rheumatoid arthritis, Alzheimer’s, multiple sclerosis and gut disorders such as inflammatory bowel disease and Crohn’s disease.
What is the vagus nerve’s connection to long COVID?
A study posted on the Preprints with Lancet server in June this year, took a look at patients with Post-Covid-19 Condition (PCC) or long COVID. It attempted to find out whether dysfunction of the vagus nerve could be responsible for symptoms these patients experienced, including persistent dysphonia (hoarseness), dysphagia (swallowing difficulties), dizziness, shortness of breath, fast heart rates and gastrointestinal disturbances.
The study found that those with PCC were more likely to have vagus nerve-related symptoms, compared to those who had recovered from COVID-19 and those not infected, indicating that vagus nerve dysfunction could have a role in the pathophysiology of PCC.
The study, also presented at last year’s European Congress of Clinical Microbiology and Infectious Diseases suggested that many symptoms connected to PCC could be linked to the effect of the coronavirus on the vagus nerve.
Other papers have also looked at impaired vagal activity in long COVID patients, as well as potential therapeutic approaches that include vagal nerve stimulation
Does vagus nerve stimulation benefit all patients?
Implanted vagus nerve stimulation does not work for everybody, and is not intended to replace conventional treatment, states the Mayo Clinic’s website. It is an adjuvant treatment for most conditions, not a primary treatment, says E.S. Krishnamoorthy, neuropsychiatrist and founder, Buddhi Clinic, Chennai. VNS is still being studied and, more research is needed into its potential therapeutic effect.
Dr. Krishnamoorthy also cautions that stimulation of the vagus nerve with a devic must not be done at home. Since the nerve regulates heartbeat and blood pressure, cardiac clearance is needed, Dr. Krishanmoorthy, who uses this method as part of broader treatment regimens, explains. “There are inhibitory and stimulatory protocols to be followed while using these devices, and so it has to be done under a doctor’s supervision.”