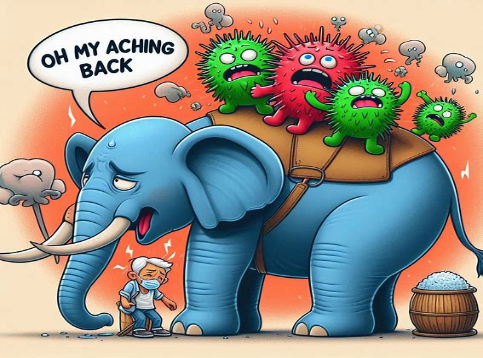
Can COVID-19 cause a rare spinal condition called transverse myelitis? Learn what TM is and see the evidence connecting the two conditions.
The year 2020 has been one for the books: a worldwide pandemic, government shutdowns, quarantining, virtual learning, working from home, wearing masks, capacity restrictions, social distancing, you name it. COVID-19 has directly impacted everyone’s lives in so many ways over the past year; and, because the virus is so new, researchers and scientists continue to study it and find out more about it each day.
One nuance that researchers continue to focus on is the so-called long haulers—people dealing with the lingering effects of COVID such as chronic lung disease, cognitive decline, and psychological effects.
There’s a possible connection between COVID-19 and a rare spinal cord disorder known as transverse myelitis (TM). To date, there have been three known cases of acute transverse myelitis due to COVID-19; and, although these three case reports are not necessarily enough to prove that COVID causes TM, researchers are delving into the possibility of a connection between the virus and this rare spinal condition.
What Is Transverse Myelitis?
Transverse myelitis is an inflammation of the spinal cord and can be caused by infections, immune system disorders, and other disorders that may damage or destroy myelin.
Myelin is an insulating layer that forms around. It is made up of protein and fatty substances and it serves as a defensive sheath that allows electrical impulses to transmit quickly and efficiently along the nerve cells.
The “insulating” role for myelin is essential for normal motor function, sensory function, and cognition. Without it, the electrical impulses sent and received by spinal cord bleed off and nerves don’t get the messages, which can result in muscle spasms, twitching, numbness and more. The most common myelin-destroying (demyelinating) disorder is multiple sclerosis.
Transverse myelitis can affect people of any race, gender, or age; and, although there are treatments, there is no cure. Typical treatments (i.e., corticosteroids and other therapies that suppress the immune system) are only aimed at preventing or minimizing permanent neurological damage.
There is already a well-known link of certain strains of COVID-19 with prolonged neurological consequences, and there have been three case reports that seem to link COVID-19 with acute transverse myelitis because of a possible inflammatory complication affecting the myelin of the spinal cord.
How Can I Recognize Transverse Myelitis?
There are four classic features of transverse myelitis:
- Weakness of the legs and arms
- Pain, typically starting in the lower back and often causing shooting sensations that radiate down the legs, arm, or torso
- Sensory alterations in the legs, torso, and genital regions
- Bowel and bladder dysfunction
You may also experience muscle spasms, a general feeling of discomfort, headache, fever, and loss of appetite. The segment of the spinal cord at which the damage occurs determines which parts of the body are affected.
Your doctors will use various methods to diagnose transverse myelitis. Like most diagnoses, it all starts with a thorough medical evaluation. Then, most physicians will also perform a thorough neurological exam, attempting to first rule out any issues that would require emergency intervention.
When your doctor suspects transverse myelitis is suspected, he or she may order diagnostic tests such as:
- Magnetic resonance imaging (MRI)
- Blood tests
- Lumbar puncture
Treating Transverse Myelitis
There is no cure for transverse myelitis, and treatment is aimed at addressing symptoms and managing complications. Treatments may include:
- Intravenous corticosteroid drugs
- Pain medicines
- Antiviral medications
- Plasma exchange therapy
- Immunomodulating drugs
- Intravenous immunoglobin (IVIG) treatment
Following initial therapy, it is important to stay active, work your treatment and don’t do anything to impede your nervous system’s recovery, like smoke.
So, let’s cut to the chase. What’s the prognosis here?
The hard facts are that while most people with transverse myelitis have at least a partial recovery, for some people, recovery may continue for up to two years (and, in some cases, longer) after the initial “attack” and may be incomplete. A combo of drug and physical therapy may improve the physical manifestation of TM.
Research has suggested that a rapid onset of symptoms generally results in a slower, poorer recovery. It is also not unheard of to have a complete recovery and then suffer a relapse. In all cases of transverse myelitis, your doctors need to find and treat the underlying cause.
The National Institute of Neurological Disorders and Stroke is working to better understand the process by which the immune system destroys or attacks myelin, which hopefully will lead to more answers and improved treatment and prevention of TM. While it’s well-documented that MS, bacterial infections and other viruses can cause transverse myelitis, researchers must continue to be vigilant about the possible connection between COVID-19 and TM as well.
The worldwide COVID-19 pandemic has flipped all of our lives upside down for the last year. Researchers continue to learn more about this virus and its long-term repercussions.
New data will continue to emerge about a possible connection between COVID-19 and neurological illnesses such as transverse myelitis., keep doing what infectious disease experts have been saying for months: Wear a mask in all public places, stay at least 6 feet away from other people, wash and sanitize your hands frequently, and avoid crowds or poorly ventilated spaces.