Authors: Bethany Milliron, Travis S Henry, Srihari Veeraraghavan, Brent P Little
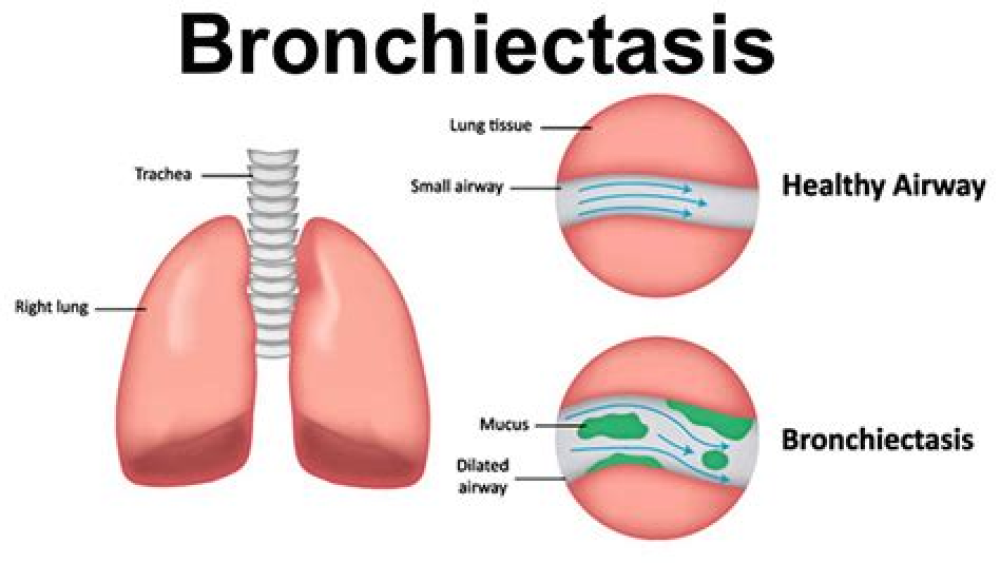
Bronchiectasis is permanent irreversible dilatation of the airways and occurs in a variety of pathologic processes. Recurrent infection and inflammation and the resulting chemical and cellular cascade lead to permanent architectural changes in the airways. Bronchiectasis can confer substantial potential morbidity, usually secondary to recurrent infection. In severe cases of bronchiectasis, massive hemoptysis can lead to death. Thin-section computed tomography is the most sensitive imaging modality for the detection of bronchiectasis; findings include bronchial diameter exceeding that of the adjacent pulmonary artery and lack of normal tapering of terminal bronchioles as they course toward the lung periphery. The authors will review various causes of bronchiectasis, including common causes, such as recurrent infection or aspiration, and uncommon causes, such as congenital immunodeficiencies and disorders of cartilage development. The authors will also present an approach emphasizing the distribution (apical versus basal and central versus peripheral) and concomitant findings, such as nodules, cavities, and/or lymphadenopathy, that can assist in narrowing the differential diagnosis. Although an adequate understanding of these underlying causes in conjunction with their specific imaging appearances will allow radiologists to more confidently determine the process causing this common radiologic finding, clinical history and patient demographic characteristics play an integral role in determining a pertinent and concise differential diagnosis. Online supplemental material is available for this article.
For More Information: https://pubs.rsna.org/doi/10.1148/rg.2015140214