Authors: Timothy L. Wong* and Danielle J. Weitzer
Abstract
Background and Objectives: Long COVID defines a series of chronic symptoms that patients may experience after resolution of acute COVID-19. Early reports from studies with patients with long COVID suggests a constellation of symptoms with similarities to another chronic medical illness—myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). A review study comparing and contrasting ME/CFS with reported symptoms of long COVID may yield mutualistic insight into the characterization and management of both conditions. Materials and Methods: A systemic literature search was conducted in MEDLINE and PsycInfo through to 31 January 2021 for studies related to long COVID symptomatology. The literature search was conducted in accordance with PRISMA methodology. Results: Twenty-one studies were included in the qualitative analysis. Long COVID symptoms reported by the included studies were compared to a list of ME/CFS symptoms compiled from multiple case definitions. Twenty-five out of 29 known ME/CFS symptoms were reported by at least one selected long COVID study. Conclusions: Early studies into long COVID symptomatology suggest many overlaps with clinical presentation of ME/CFS. The need for monitoring and treatment for patients post-COVID is evident. Advancements and standardization of long COVID research methodologies would improve the quality of future research, and may allow further investigations into the similarities and differences between long COVID and ME/CFS.
1. Introduction
Coronavirus disease 2019 (COVID-19), a highly contagious respiratory disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2), was declared a pandemic by the World Health Organization in March 2020 [1]. As of 7 March 2021, there are over 100 million cumulative cases, with over 2.5 million deaths worldwide [2]. Within the United States alone, there have been almost 30 million cumulative cases, with over half a million deaths as of mid-March [3].
In terms of clinical profile and disease symptomatology, individuals afflicted with COVID-19 vary greatly in terms of clinical presentation [4,5]. While some individuals remain asymptomatic, others experience symptoms generally associated with other viral respiratory diseases, such as fever, cough, dyspnea, headache, and sore throat [6,7,8]. During the acute phase of COVID-19, various other systemic impacts including gastrointestinal, renal, hepatological, rheumatological, and neurological symptoms and complications have been reported [9,10]. While there continues to be significant public concern and research centered around the acute course and presentation of COVID-19, there is increasing public and academic interest in the chronic sequelae of the disease [11,12,13].
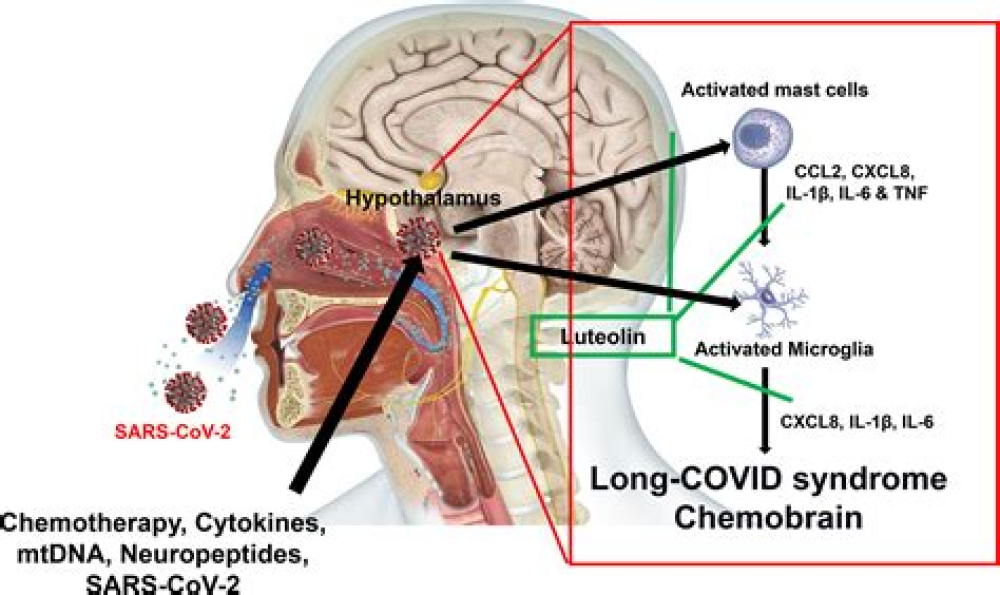
There is currently no uniform terminology for this so-called long COVID [14], or, as it has also been termed, long-haul COVID-19 [15,16], post-COVID syndrome [17], chronic COVID syndrome [18], and more recently, post-acute sequelae of SARS-COV-2 infection (PASC) [19]. There is no established case definition or diagnostic criteria, but some have suggested long COVID as being defined by persistent signs and symptoms more than four weeks after initial infection with SARS-COV-2 [20,21]. Research into the prevalence of long COVID is ongoing, but one study has estimated that over 87% of COVID patients continue to experience at least one symptom, two months after COVID symptom onset [22]. The risk for developing long COVID does not appear to be correlated with the severity of acute illness [23]. The etiologies of long COVID are uncertain, with some linking it to autoimmune condition or hyperinflammatory states after resolution of acute COVID [24,25,26].
The characteristics and mysterious nature of long COVID led some to suggest a connection to a debilitating but lesser-known chronic medical condition: myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) [27,28,29]. ME/CFS is a long-term complicated illness characterized by at least six months of fatigue and exhaustion. This illness is estimated to account for USD 18–51 billion dollars in economic costs. In total, 2.5 million Americans suffer from chronic fatigue syndrome, with one quarter of those diagnosed being house or bed bound [30]. Within the general population, the prevalence of chronic fatigue ranges between ten and forty percent. Despite this, due to a lack in diagnostic testing without consistent and established treatments, there has been disputes regarding the actual existence of chronic fatigue syndrome. As the diagnosis is mostly based upon patient’s subjective feedback, this has sparked stigma that has led to dismissive behaviors in the medical community. The misconception regarding chronic fatigue syndrome may have been started because of how it was initially characterized. For example, early reports of chronic fatigue were described as a derogatory term known as the Yuppie Flu, which initially characterized the illness among young workers, with the implication of individuals trying to get out of their job responsibilities. However, since this time, the illness has come to be understood to rather affect a broader array of populations, but with a predominance of women being more affected than men [31]. To better understand this illness, improved knowledge of the research and definitions surrounding the illness is needed.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8145228/