Authos: Ming Tong,1Yu Jiang,2Da Xia,3Ying Xiong,3Qing Zheng,4Fang Chen,2Lianhong Zou,2Wen Xiao,2 and Yimin Zhu2
J Infect Dis. 2020 Sep 15; 222(6): 894–898.Published online 2020 Jun 24. doi: 10.1093/infdis/jiaa349 PMCID: PMC7337874PMID: 32582936
Abstract
In a retrospective study of 39 COVID-19 patients and 32 control participants in China, we collected clinical data and examined the expression of endothelial cell adhesion molecules by enzyme-linked immunosorbent assays. Serum levels of fractalkine, vascular cell adhesion molecule-1 (VCAM-1), intercellular adhesion molecule 1 (ICAM-1), and vascular adhesion protein-1 (VAP-1) were elevated in patients with mild disease, dramatically elevated in severe cases, and decreased in the convalescence phase. We conclude the increased expression of endothelial cell adhesion molecules is related to COVID-19 disease severity and may contribute to coagulation dysfunction.Keywords: COVID-19, fractalkine, endothelial cell adhesion molecules, D-dimer, coagulopathy
In December 2019, a severe public health event, manifested mainly with fever and respiratory tract symptoms, broke out in Wuhan, China, and quickly spread throughout the country and the world [1], which was named coronavirus disease 2019 (COVID-19) by the World Health Organization. As of 1 May 2020, more than 3 million cases have been confirmed, while more than 200 000 patients have died, and the number is continuing to increase.
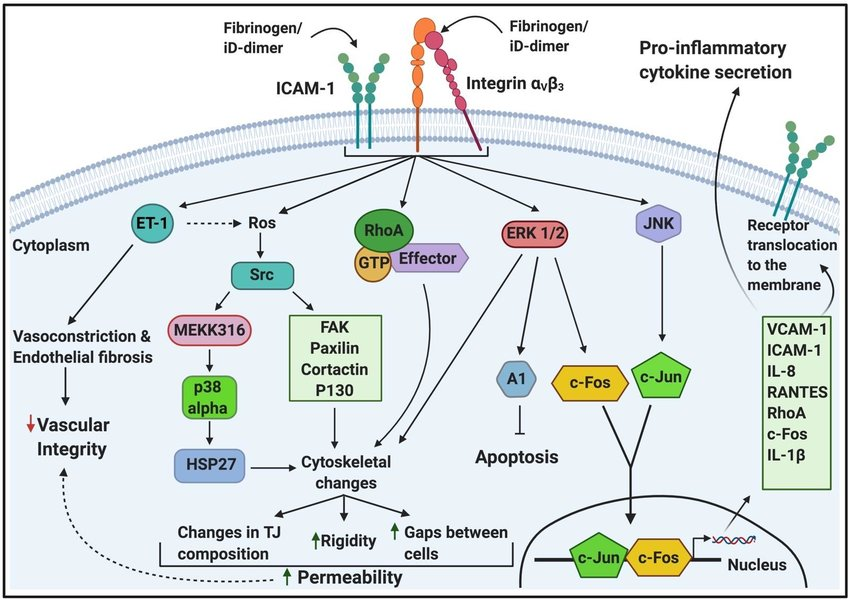
COVID-19 causes a systemic inflammatory response, involving dysregulation and misexpression of many inflammatory cytokines [1]. The recruitment and activation of inflammatory cells depend on the expression of many classes of inflammatory mediators, such as cytokines (interleukin [IL]-1, IL-6, and IL-18), chemokines (fractalkine [FKN]), and adhesion molecules (intercellular adhesion molecule 1 [ICAM-1)] and vascular cell adhesion molecule-1 [VCAM-1]) [2]. Pathological evidence of venous thromboembolism, direct viral infection of the endothelial cells, and diffuse endothelial inflammations have been reported in recent studies [2, 3]. Therefore, it is of significance to investigate the expression of endothelial cell adhesion molecules in COVID-19.
Here, we collected clinical data and blood samples from confirmed COVID-19 patients in the Fourth People’s Hospital of Yiyang in Hunan, China, and performed enzyme-linked immunosorbent assays (ELISAs) to study the expression of inflammatory mediators and endothelial cell adhesion molecules in COVID-19 patients.Go to:
METHODS
Study Participants
A retrospective study was conducted. From 1 February to 10 March 2020, 39 COVID-19 patients were recruited at the Infectious Disease Ward in the Fourth People’s Hospital of Yiyang, Hunan, China, and 32 uninfected participants were recruited from the physical examination center of Hunan Provincial People’s Hospital. All patients tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and were hospitalized. Nine patients were diagnosed with severe pneumonia, while 30 had mild disease. Mild pneumonia was defined as positivity in quantitative reverse transcription polymerase chain reaction (qRT-PCR) tests, with typical chest tomography imaging features of viral pneumonia [4], while severe pneumonia was defined as mild pneumonia plus 1 of the following criteria: (1) respiratory distress with a respiratory rate ≥ 30 times per minute;
(2) oxygen saturation ≤ 93% at rest; (3) oxygenation index ≤ 300 mmHg (1 mmHg = 0.133 kPa); (4) respiratory failure requiring ventilation; (5) refractory shock; and
(6) admission to the intensive care unit for other organ failure. All patients were given interferon-α2b (5 million units twice daily, atomization inhalation) and lopinavir plus ritonavir (500 mg twice daily, orally) as antiviral therapy. All patients with severe disease received preventive anticoagulant treatment with low-molecular-weight heparin (LMWH) 5000 IU/day by subcutaneous injection for 7 days. No patients died during the observation period.
The criteria for discharge were: (1) absence of fever for at least 3 days; (2) significant improvement in both lungs on chest computed tomography (CT); (3) clinical remission of respiratory symptoms; and (4) repeated negativity in RT-PCR tests of throat swab samples at least 24 hours apart.
Clinical data were measured at enrolment. The study was approved by the Medical Ethics Review Board of Hunan Provincial People’s Hospital (No. 2020-10). All study participants provided written informed consent.
Sample Collection
Blood samples were collected at admission from each patient in a fasting state and repeated during the convalescence period for severe cases. Serum lipids, glucose, C-reaction protein (CRP), and D-dimer were determined by conventional laboratory methods. Blood samples of control subjects were also collected and tested. The obtained blood samples were placed in tubes containing EDTA and immediately centrifuged at 1500g and stored at −80°C.
Enzyme-Linked Immunosorbent Assay
Quantitative determination of IL-18, tumor necrosis factor-α (TNF-α), interferon-γ (IFN-γ), FKN, VCAM-1, ICAM-1, and vascular adhesion protein-1 (VAP-1) was performed using commercially available ELISA kits (BOSTER).
Statistical Analysis
Categorical variables were reported as number and percentages, and significance was detected by χ2 or Fisher exact test. The continuous variables were compared using independent group t tests and described using mean and standard deviation if normally distributed, or compared using the Mann-Whitney U test and Kruskal-Wallis H test and described using median and interquartile range (IQR) value if not. Paired comparisons of the severe group were analyzed with the Nemenyi test. Statistical analysis was performed by SPSS version 19.0. Two-sided P values < .05 were considered statistically significant.
Patient and Public Involvement
In this retrospective study, no patients were directly involved in the study design, question proposal, or the outcome measurements. No patients were asked for input concerning interpretation or recording of the results.
RESULTS
Patient Characteristics
Demographic information is shown in Table 1. Briefly, 20 patients were male, 19 patients were female, 16 controls were male, and 16 were female, and the median ages in the control, mild, and severe groups were 52, 49, and 54 years, respectively. Nine patients had severe disease, while 30 cases had mild disease. No significant differences were found between patients with mild disease and control participants in age, smoking, cardiovascular disease (CVD), autoimmune disease, low-density lipoprotein cholesterol (LDL-C), triglycerides, total cholesterol (CHO), glucose, and D-dimer. Significant differences in D-dimer were observed between the severe disease and control participants (median, 4.49 vs 0.34, respectively; P < .05), while no significant differences in age, smoking, CVD, autoimmune disease, and the levels of triglycerides, LDL-C, CHO, and glucose were observed. Significant differences in age (median, 54 vs 49; P < .05), triglycerides (median, 0.93 vs 1.29; P < .05), D-dimer (median, 4.49 vs 0.35; P < .05), and length of stay (mean, 16.6 vs 10.6; P < .05) were observed between patients with severe and mild disease, respectively, while no significant differences in smoking, CVD, autoimmune disease, and the levels of LDL-C, CHO, and glucose were observed.
Table 1.
Characteristics of Study Participants
| Characteristic | Overall | Control | Mild Disease | Severe Disease |
|---|---|---|---|---|
| Sex, male/female, n/n | 36/35 | 16/16 | 16/14 | 4/5 |
| Age, y, median (25, 75 percentile)a | 50 (42, 57) | 52 (44, 60) | 49 (25, 55) | 54 (47, 75)* |
| Current smoker, n (%) | 10 (14) | 6 (19 | 2 (7) | 2 (22) |
| Cardiovascular disease, n (%) | 8 (11) | 5 (16) | 1 (3) | 2 (22) |
| Autoimmune disease, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| LDL-C, mmol/L, median (25, 75 percentile)a | 1.81 (1.53, 2.17) | 1.81 (1.45, 2.03) | 1.81 (1.52, 2.34) | 2.11 (1.58, 2.41) |
| Triglycerides, mmol/L, median (25, 75 percentile)a | 1.17 (0.93, 1.54) | 1.24 (0.93, 1.54) | 1.29 (0.96, 1.64) | 0.93 (0.71, 1.03)* |
| Total cholesterol, mmol/L, mean ± SD | 3.91 ± 1.14 | 3.96 ± 1.48 | 3.83 ± 0.91 | 4.00 ± 0.98 |
| Glucose, mmol/L, median (25, 75 percentile)a | 5.5 (4.3, 6.7) | 5.2 (4.3, 6.7) | 5.5 (4.4, 6.7) | 6.2 (4.7, 7.8) |
| D-dimer, mg/L, median (25, 75 percentile)a | 0.37 (0.25, 0.58) | 0.34 (0.25, 0.46) | 0.35 (0.15, 0.52) | 4.49 (1.29, 7.00)b,,* |
| Length of stay, d, mean ± SD | 12.0 ± 4.3 | … | 10.6 ± 3.5 | 16.6 ± 3.5* |
Abbreviation: LDL-C, low-density lipoprotein cholesterol.
aCompared with control group.
b P value <.05 compared with mild disease group.
*P < .05.
Expression of Inflammatory Mediators and Endothelial Cell Adhesion Molecules in COVID-19 Patients and Uninfected Participants
The serum levels of the following were higher in patients with mild disease than in control participants: FKN (median, 880.1 vs 684.6 pg/mL; P < .01); VCAM-1 (median, 3742.3 vs 891.4 pg/mL; P < .01); ICAM-1 (median, 2866.1 vs 1287.4 pg/mL; P < .01); VAP-1 (median, 16.81 vs 16.68 pg/mL; P = .41) (Figure 1A–D); CRP (median, 10.75 vs 1.59 mg/L; P < .01); IL-18 (median, 415.4 vs 276.5 pg/mL; P = .09); TNF-α (median, 257.1 vs 242.9 pg/mL; P < .01); and IFN-γ (median, 46.00 vs 42.51 pg/mL; P = .50) (Supplementary Figure 1A–D). Of these, CRP, TNF-α, FKN, VCAM-1, and ICAM-1 were significantly elevated.

Expression of endothelial cell adhesion molecules in COVID-19 patients and uninfected participants, the horizontal lines represent median with interquartile range: (A) fractalkine; (B) vascular cell adhesion molecule-1 (VCAM-1); (C) intercellular adhesion molecule 1 (ICAM-1); and (D) vascular adhesion protein-1 (VAP-1). * P < .05; ** P < .01.
The serum levels of the following were significantly higher in patients with severe disease than in control participants: FKN (median, 1457.5 vs 684.6 pg/mL; P < .01); VCAM-1 (median, 4991.3 vs 891.4 pg/mL; P < .01); ICAM-1 (median, 4498.2 vs 1287.4 pg/mL; P < .01); VAP-1 (median, 28.80 vs 16.68 pg/mL; P < .01) (Figure 1A–D); CRP (median, 43.64 vs 1.59 mg/L; P < .01); IL-18 (median, 670.7 vs 276.5 pg/mL; P < .01); TNF-α (median, 274.2 vs 242.9 pg/mL; P < .01); and IFN-γ (median, 76.50 vs 42.51 pg/mL; P < .01) (Supplementary Figure 1A–D).
The serum levels of the following were significantly higher in patients with severe disease than in patients with mild disease: FKN (median, 1457.5 vs 880.1 pg/mL; P < .01); VCAM-1 (median, 4991.3 vs 3742.3 pg/mL; P < .05); ICAM-1 (median, 4498.2 vs 2866.1 pg/mL; P < .05); VAP-1 (median, 28.80 vs 16.81 pg/mL; P < .01) (Figure 1A–D); CRP (median, 43.64 vs 10.75 mg/L; P < .01); IL-18 (median, 670.7 vs 415.4 pg/mL; P < .01); TNF-α (median, 274.2 vs 257.1 pg/mL; P < .05); and IFN-γ (median, 76.50 vs 46.00 pg/mL; P < .01) (Supplementary Figure 1A–D).
For severe cases, the serum levels of the following were lower in the convalescence phase than during the acute phase: FKN (median, 1028.2 vs 1457.5 pg/mL; P < .05); VCAM-1 (median, 3420.9 vs 4991.3 pg/mL; P < .01); ICAM-1 (median, 3046.9 vs 4498.2 pg/mL; P < .01); VAP-1 (median, 23.90 vs 28.80 pg/mL; P = .17) (Figure 1A–D); CRP (median, 10.20 vs 43.64 mg/L; P < .01); IL-18 (median, 514.6 vs 670.7 pg/mL; P < .01); TNF-α (median, 265.1 vs 274.2 pg/mL; P < .01); IFN-γ (median, 66.30 vs 76.50 pg/mL; P = .05) (Supplementary Figure 1A–D); and D-dimer (median, 0.45 vs 4.49; P < .01) (Supplementary Figure 2). Of these, IL-18, TNF-α, FKN, VCAM-1, ICAM-1, and D-dimer were significantly lower.Go to:
DISCUSSION
Three novel findings were identified in our study. First, the endothelial cell adhesion markers FKN, VCAM-1, and ICAM-1 were elevated in COVID-19 patients. Second, the severity of COVID-19 was associated with the serum levels of CRP, IL-18, TNF-α, IFN-γ, FKN, VCAM-1, ICAM-1, and VAP-1. Third, recovery from severe COVID-19 was associated with reductions in serum CRP, IL-18, TNF-α, FKN, VCAM-1, ICAM-1, and D-dimer levels.
Endothelial activation is related to severe COVID-19, and antiphospholipid antibodies, von Willebrand factor, and factor VIII may play a role in coagulopathy [5]. Endothelial cells express angiotensin-converting enzyme 2 (ACE2), the receptor for SARS-CoV-2 [6], and the interaction of SARS-CoV-2 and ACE2 possibly mediates endothelial activation. Endothelial cells are an essential component of the coagulation system and their integrity and functionality are critical to maintaining hemostasis, whereas endothelial cell activation or injury may result in platelet activation, thrombosis, and inflammation [7]. Dysfunctional endothelial cells activated by proinflammatory cytokines may contribute to the pathogenesis of thrombosis by altering the expression of pro- and antithrombotic factors [8, 9].
In this cohort of COVID-19 patients, although apparent thrombosis formation was excluded by Doppler ultrasound in deep veins in the lower extremities and repeated chest CT scans, we found an interesting phenomenon in patients with severe disease, that is serum D-dimer levels were elevated during the acute phase and decreased significantly during the convalescence phase. As an indirect marker of coagulation activation, elevated D-dimer has been reported in several studies and confirmed to correlate with an increased likelihood of death in COVID-19 patients [10]. We consider that the relationship between prethrombosis levels of D-dimer and thrombotic disease is likely partly attributable to subclinical clot formation.
Severe COVID-19 is commonly complicated by coagulopathy, while disseminated intravascular coagulation may contribute to most deaths [11]. Anticoagulant treatment may decrease mortality due to coagulopathy [12]. In patients with severe disease, serum FKN, ICAM-1, VCAM-1, and D-dimer levels declined significantly after antiviral and anticoagulant treatment. In addition to stimulating the immune system to suppress viral replication and clear pathogens, interferon-α also inhibits the inflammatory immune response that leads to histological damage [13]. Hence, we speculate that the dynamic changes in these molecules resulted from the alleviation of endothelial cell injuries, the anti-inflammatory effect of medications, or recovery from COVID-19.
Limitations should be noted when interpreting the results of this study. First, the number of patients with severe disease was low, which may lead to statistical deviation. Second, due to tissue sample inaccessibility, the expression of endothelial activation molecules was not measured in tissues. Third, because we did not measure the direct biomarkers in the coagulation system, the specific disturbed pathways and mechanisms are still unknown. Fourth, due to the anti-inflammatory effect of interferon-α, the relationship between the anticoagulant effect of LMWH and the decreased expression of endothelial cell adhesion molecules in COVID-19 is still uncertain, and requires further study.
In conclusion, based on the results of this study, increased expression of endothelial cell adhesion molecules is related to COVID-19 and disease severity, and may contribute to coagulation dysfunction.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
jiaa349_suppl_Supplementary_Figure_1
Click here for additional data file.(328K, png)
jiaa349_suppl_Supplementary_Figure_2
Click here for additional data file.(70K, png)
Notes
Acknowledgments. We sincerely thank clinicians at the Forth People’s Hospital of Yiyang, Hunan, China.
Financial support. This work was supported by the Key Research and Development Program of Hunan Province (grant number 2020SK3011).
Potential conflicts of interest. All authors: No reported conflicts of interests. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.Go to:
References
1. Huang C, Wang Y, Li X, et al. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [PMC free article] [PubMed] [Google Scholar]2. Varga Z, Flammer AJ, Steiger P, et al. . Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020; 395:1417–8. [PMC free article] [PubMed] [Google Scholar]3. Wichmann D, Sperhake JP, Lütgehetmann M, et al. . Autopsy findings and venous thromboembolism in patients with COVID-19 [published online ahead of print 6 May 2020]. Ann Intern Med doi: 10.7326/M20-2003. [PMC free article] [PubMed] [CrossRef] [Google Scholar]4. Shi H, Han X, Jiang N, et al. . Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20:425–34. [PMC free article] [PubMed] [Google Scholar]5. Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res 2020; 190:62. [PMC free article] [PubMed] [Google Scholar]6. Turner AJ, Hiscox JA, Hooper NM. ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci 2004; 25:291–4. [PMC free article] [PubMed] [Google Scholar]7. Krüger-Genge A, Blocki A, Franke RP, Jung F. Vascular endothelial cell biology: an update. Int J Mol Sci 2019; 20:4411. [PMC free article] [PubMed] [Google Scholar]8. Wong R, Lénárt N, Hill L, et al. . Interleukin-1 mediates ischaemic brain injury via distinct actions on endothelial cells and cholinergic neurons. Brain Behav Immun 2019; 76:126–38. [PMC free article] [PubMed] [Google Scholar]9. Fong LY, Ng CT, Zakaria ZA, et al. . Asiaticoside inhibits TNF-α-induced endothelial hyperpermeability of human aortic endothelial cells. Phytother Res 2015; 29:1501–8. [PubMed] [Google Scholar]10. Zhou F, Yu T, Du R, et al. . Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–62. [PMC free article] [PubMed] [Google Scholar]11. Chen N, Zhou M, Dong X, et al. . Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507–13. [PMC free article] [PubMed] [Google Scholar]12. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020; 18:1094–9. [PubMed] [Google Scholar]13. Lee AJ, Ashkar AA. The dual nature of type I and type II interferons. Front Immunol 2018; 9:2061. [PMC free article] [PubMed] [Google Scholar]