Authors: Eleonora Calabretta, 1 , 12 Jose M. Moraleda, 2 Massimo Iacobelli, 3 Ruben Jara, 4 Israel Vlodavsky, 5 Peter O’Gorman, 6 Antonio Pagliuca, 7 Clifton Mo, 8 Rebecca M. Baron, 9 Alessio Aghemo, 10 , 12 Robert Soiffer, 8 Jawed Fareed, 11 Carmelo Carlo‐Stella, 1 , 12 , * and Paul Richardson 8 , *
Br J Haematol. 2021 Apr; 193(1): 43–51.Published online 2021 Feb 4. doi: 10.1111/bjh.17240 PMCID: PMC8014053PMID: 33538335
Introduction
The coronavirus disease 2019 (COVID‐19) pandemic, a viral illness caused by the severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2), 1 has produced at the time of this writing nearly 33 million cases of infection, with over a million deaths in 235 countries, 2 causing an unprecedented burden on healthcare systems and a severe global socioeconomic crisis. As the pandemic spreads, knowledge on the disease course, as well as potential risk factors and predictors of severity is increasing daily, and initial data from randomised controlled studies have allowed care providers to refine therapeutic strategies. Nonetheless, mortality is markedly elevated among those presenting with severe disease, long‐term sequelae among survivors are unknown, and vaccine‐based therapies currently remain at early stages of development.
Most reported cases are asymptomatic or present with mild symptoms; however, 7–26% of hospitalised patients experience severe disease, often requiring admission to intensive care units (ICUs), with progressive multiple organ dysfunction and high mortality. 3 , 4 , 5 Such differences in clinical outcomes have led physicians to initiate diverse pharmacological therapies at various stages of the disease, generating challenges as to the most appropriate therapeutic choice for COVID‐19. In this context, the use of dexamethasone has significantly reduced mortality rates in critically ill patients requiring supplemental oxygen or mechanical ventilation, 6 and remdesivir has demonstrated clinical benefit in hospitalised patients, but with unknown survival benefit to date 7 ; additional effective treatment options are therefore urgently needed.
In an initial attempt to provide a uniform and widely reproducible methodology to guide systematic treatment strategies, a three‐stage classification of COVID‐19 has been proposed. 8 The Stage I or ‘early infection’ occurs at the initial establishment of disease with high viral replication, and commonly presents with a range of complaints that can include mild and often non‐specific influenza‐like signs and symptoms. Stage II is the ‘pulmonary phase’, with preferential viral‐mediated injury of the lung parenchyma and this is characterised by shortness of breath, hypoxia and pulmonary infiltrates with some degree of lung inflammation. Stage III is characterised by an exaggerated host immune‐inflammatory response to the virus, leading to acute respiratory distress syndrome (ARDS) and multi‐organ failure (MOF).Go to:
Endothelial cells are a preferential target of COVID‐19 resulting in widespread endotheliitis
Emerging evidence suggests that endothelial damage and subsequent morphological and functional changes in the endothelium play important roles in COVID‐19‐induced hyperinflammation. The virus, which binds to the angiotensin‐converting enzyme 2 (ACE2) receptor, 9 displays a profound tropism for human lung and small intestine epithelium, as well as the vascular endothelium. 10 In an important case series from Varga et al., 11 postmortem histology from three patients affected by late‐stage COVID‐19, revealed viral inclusions in endothelial apoptotic cells and microvascular lymphocytic endotheliitis, with infiltration of inflammatory cells around the vessels and endothelial cells (ECs), as well as evidence of endothelial apoptotic cell death in the lung, kidney, small bowel and heart. Additionally, autopsy findings of 27 patients in another series confirmed the detection of the SARS‐CoV‐2 in multiple organs, including the respiratory tract, pharynx, heart, liver, brain, and kidneys. 12 Immunofluorescence of kidney specimens from six of the 27 patients showed the presence of SARS‐CoV‐2 protein in all renal compartments, and in three of the patients preferentially in the endothelium of the glomerulus. Similar microscopic findings were also noted in lung specimens from seven patients with COVID‐19, which displayed small vessel endotheliitis, microvascular thrombosis and angiogenesis, along with the presence of SARS‐CoV‐2 in pulmonary ECs, an observation strongly supporting the vascular tropism of the virus. 13 Lastly, Stahl et al. 14 have identified in the plasma and serum of 19 critically ill patients with COVID‐19 evidence of disruption of the endothelial glycocalyx, reflected by increased levels of the Tie‐2 receptor and syndecan‐1 (SDC‐1), a heparan sulphate (HS) proteoglycan. This particular observation is of interest as the endothelial glycocalyx covers the luminal surface of ECs, and its integrity is vital for the maintenance of vascular homeostasis.
Such findings suggest that virus‐mediated apoptosis may promote endothelial barrier disruption with interstitial oedema and increased recruitment of circulating activated immune cells, thus causing widespread endothelial dysfunction, as well as activation of platelets and the coagulation cascade leading to venous and arterial thrombosis. 15 Altered pro‐inflammatory and pro‐thrombotic status is confirmed by the presence of elevated inflammation‐related indices (e.g. C‐reactive protein and serum ferritin), humoral biomarkers [interleukin (IL)‐2, IL‐6, IL‐7, granulocyte‐colony stimulating factor (G‐CSF), tumour necrosis factor‐alpha (TNF‐α)], and indicators of an increased pro‐coagulant‐fibrinolytic state [e.g. von Willebrand factor (VWF), D‐dimer, fibrinogen]. Further, factor VIII (FVIII), a potent and key factor in the coagulation process, is greatly increased in ICU patients with COVID‐19. 16
In this setting, it has been proposed that the systemic hyperinflammation observed in severe COVID‐19 is comparable to a cytokine release syndrome (CRS), or cytokine storm. IL‐6 has a central role in the generation of the cytokine storm, and is commonly elevated in the serum of severely ill patients with COVID‐19. 17 High levels of IL‐6 activate ECs, thus resulting in vascular leakage, further cytokine secretion and activation of the complement and coagulation cascades. 18 Interestingly, a population of IL‐6 producing monocytes was found to be expanded in the peripheral blood of ICU patients 19 and an aberrant macrophage response exhibiting increased levels of pro‐inflammatory cytokines has been detected in bronchoalveolar fluid, especially in severely ill patients. 20 Although the exact driver of monocyte activation remains unclear, such cells are attracted to the endothelium, where the release of highly noxious molecules, such as reactive oxygen species (ROS), contributes to endothelial dysfunction and promotes hyperinflammation. 21 Further, activated monocytes enhance tissue factor expression and form aggregates with platelets through P‐selectin interaction and hence augmenting the pro‐coagulant response. 22 Indeed, significantly increased levels of VWF and FVIII and thrombomodulin, 16 aberrant coagulation, thrombosis and microangiopathy are very common in critically ill patients with COVID‐19, resulting in a disseminated intravascular coagulation (DIC)‐like syndrome characterised by massive fibrin formation and organ dysfunction. 23 Likewise, adaptive immunity actively participates in the establishment of the inflammatory response; specifically, activated and proliferating CD8+ T cells are prevalent in mild COVID‐19, whereas critically ill patients display higher levels of hyperactive IL‐6‐producing CD4+ T cells, which may contribute to disease severity, even after viral clearance. 17 Interestingly, T cells show phenotypical signs of an exhausted, functionally unresponsive state, thus allowing viral escape from immune surveillance. 22 Once initiated, the endotheliitis and resultant cytokine storm become self‐sustaining, leading to widespread organ damage. Some patients may also display features of haemophagocytic lymphohistiocytosis, such as cytopenias, hyperferritinaemia and rapid onset of MOF.
Overall, once hyperinflammation and CRS develop, rates of mortality significantly increase. 24 , 25 , 26 As direct viral activation of the vascular endothelium has an important role in initiating and maintaining the hyperinflammatory response, attempting to blunt such a response with endothelial‐protective agents is a very rational strategy. Controlled clinical trials focussing on the use of anti‐cytokine antibodies, including tocilizumab (IL‐6 inhibitor), have failed to show significant activity in this stage of the disease. 27 However, increasing evidence suggests that the altered homeostasis of the endothelium may be a key initiating event in the pathogenesis of the disease, therefore representing a potentially more promising target. 28Go to:
Endothelial cell‐related disorders in haematology: post‐bone marrow transplantation syndromes and sickle cell disease and the overlap with the pathobiology of COVID‐19
Clinically and histopathologically, COVID‐19‐associated endotheliitis resembles a spectrum of post‐bone marrow and stem cell transplantation (BMT) syndromes characterised by disruption of endothelial homeostasis and consequently dysregulation of coagulation, vascular tone, endothelial permeability and vascular inflammation. 29 These disorders include hepatic veno‐occlusive disease (VOD)/sinusoidal obstruction syndrome (SOS), idiopathic pneumonia syndrome (IPS), transplant‐associated thrombotic microangiopathy and graft‐versus‐host disease (GvHD).
Hepatic VOD/SOS develops as a result of endothelial damage to hepatic sinusoids and subsequent hepatocyte necrosis 30 . Damage to the ECs leads to a hypercoagulable state, production of inflammatory mediators, and the upregulation as well as release of heparanase. 31 Heparanase degrades the heparan sulphate scaffold of the subendothelial basement membrane, consequently allowing the extravasation of blood‐borne cells, including activated T lymphocytes, neutrophils and macrophages. 32 This cascade of events leads to postsinusoidal hypertension, hyperinflammation and ultimately MOF. Severe VOD/SOS associated with MOF without effective therapy is fatal in >80% of cases. 33 Interestingly, the histopathological examination of lung lesions in VOD/SOS shows early alveolar epithelial and lung endothelial injury, resulting in accumulation of protein‐ and fibrin‐rich inflammatory oedematous fluid in the alveolar space and progression to interstitial fibrosis, 34 , 35 as is also seen in fatal COVID‐19 cases.
Similarly, IPS, a widespread alveolar injury in the absence of identifiable infectious or non‐infectious causes, is characterised by histological evidence of EC injury with fibrin accumulation, luminal thrombosis and fibrotic processes. Adhesion molecules, such as intercellular adhesion molecule 1 (ICAM‐1) and/or vascular cell adhesion molecule 1 (VCAM‐1), are commonly upregulated, thus reflecting profound endothelial activation. 36 It has been suggested that TNF‐α directly causes endothelial injury, and increased levels of angiopoietin‐2 (Ang‐2), have been recently reported in cases of acute exacerbations of IPS, 37 similar to that seen in severely ill patients with COVID‐19. 38
Likewise, multifactorial endothelial damage has been also implicated in the development of transplant‐associated thrombotic microangiopathy, where micro‐vessel intimal swelling and necrosis lead to the formation of luminal microthrombi and subsequent microangiopathic haemolytic anaemia. Plasma levels of markers of EC injury and inflammation, such as thrombomodulin, plasminogen activator inhibitor‐1 (PAI‐1), ICAM‐1, VCAM‐1, IL‐1, TNF‐α, interferon gamma and IL‐8 are commonly elevated. 39 , 40 Endothelial dysfunction predominantly affects the kidneys and the brain, but may become widespread and progress to MOF, which in turn is associated with high mortality.
Lastly, acute GvHD (aGvHD) develops as a consequence of the activation of the immune system. Antigen‐presenting cells become activated by endothelial and tissue damage derived from direct toxicity of the conditioning regimen, thus initiating an alloreactive T‐cell response directed against recipient tissues. 41 As a result, SDC‐1 is commonly elevated in the serum of patients with GvHD and correlates with disease severity. 42 In addition to cell‐mediated cytotoxic damage, the cytokine storm generated in response to T‐cell activation and proliferation causes targeted organ damage involving mainly the skin, liver and gut. 43 It has recently been suggested that endothelial vulnerability and pro‐thrombotic shift precedes clinically evident aGvHD and that angiogenesis driven by early endothelial activation is an initiating event. 44 Indeed, increased plasma levels of VWF, 45 Ang‐2 46 and TNF receptor 1 47 have been detected in patients prior to development of aGvHD, correlating with response to therapy.
Similarly, markers of endothelial dysfunction and inflammatory activation have been detected also in the serum of patients with sickle cell disease (SCD), especially during vaso‐occlusive episodes. SCD is characterised by a chronic course of relapsing‐remitting episodes of ischaemia and then reperfusion. The polymerisation of defective haemoglobin S upon deoxygenation initiates many pathological processes, such as complement activation, generation of ROS and pro‐thrombotic molecules, secretion of numerous pro‐inflammatory cytokines and chemokines and ultimately leucocyte recruitment. 48 Oxidative stress and endothelial dysregulation plays a key role in vaso‐occlusion; ECs activated by substances released by the haemolytic process and by red blood cell adhesion initiate production and release of soluble mediators such as IL‐1β, IL‐8, IL‐6, IL‐1α and PAI‐1, 49 , 50 and increase the expression of adhesion molecules such as VCAM‐1, ICAM‐1, E‐selectin and P‐selectin, 51 , 52 reflecting a pro‐inflammatory and pro‐thrombotic shift. Vaso‐occlusive phenomena commonly affect the lung vasculature, provoking acute chest syndrome (ACS), a spectrum of diseases ranging from mild pneumonia to ARDS and MOF, which is the leading cause of morbidity and mortality in SCD. 53 Lung specimens from ACS cases showed micro‐thrombotic occlusion, endothelial VWF deposition and arterial vessel re‐modelling with initial fibrotic processes, 54 fascinatingly all comparable to the histopathological findings in COVID‐19. 55 Importantly, heme‐mediated endothelial damage to alveolar cells is regulated by the p38 mitogen‐activated protein kinase (MAPK) pathway, which plays a crucial role in the biosynthesis of pro‐inflammatory cytokines and collagen production. 56 This key pathway is also upregulated in COVID‐19 as a result of decreased ACE2 tissue functionality consequent to viral binding, and may consequently promote endotheliitis, hypercoagulation and end‐stage fibrosis. 57 , 58
In summary, post‐BMT syndromes, vaso‐occlusive organ dysfunction in SCD and COVID‐19‐associated endotheliitis share common pathological mechanisms including: i) dysregulation of the homeostasis of the endothelial milieu toward a pro‐inflammatory and pro‐thrombotic phenotype with thrombotic microangiopathy; ii) hyperproduction of inflammatory cytokines such as IL‐6, IL‐8 and TNF‐α; 59 , 60 , 61 , 62 and iii) small vessel endotheliitis and endothelial barrier dysfunction, leading to oedema of the microvascular bed, protein and fibrin accumulation and subsequent fibrotic shift. 34 , 36 All these conditions if untreated irremediably lead to MOF and display similar microscopic and macroscopic features in target organs upon pathological examination. At the molecular level, the p38 MAPK pathway may also be critical in promoting vasoconstrictive and inflammatory phenomena; its activation is described in SCD, COVID‐19 and also as a result of conditioning regimen‐induced endothelial damage in BMT. 63 Together, these findings support the notion that the pleiotropic character of the endothelium as a key regulator of the internal homeostasis, vascular tone, blood coagulation and the inflammatory process and therefore of so called ‘immune‐thrombosis’ events, make it an intriguing therapeutic target for post‐BMT disorders, SCD, and COVID‐19.Go to:
Agents targeting EC‐related disorders
Heparins
Classically, heparins have been the most widely used drugs for the treatment and prevention of endothelial cell disorders. Several animal studies and clinical trials have suggested that, in addition to its well‐known anticoagulant effects, heparin also possesses anti‐inflammatory properties, mainly mediated by inhibition of IL‐6 release and its activity, 64 a phenomena also demonstrated in patients with COVID‐19 treated with low‐molecular‐weight heparin. 65 Further, heparin is structurally related to HS, 66 a negatively charged glycosaminoglycan as described earlier, which serves as binding sites for growth factors, cytokines, selectins, extracellular‐matrix molecules, and a large number of human viruses, 67 including the SARS‐CoV‐2 virus. 68 , 69 Indeed, Clausen et al. 70 have recently demonstrated that the SARS‐CoV‐2 spike protein must bind both the ACE2 receptor and HS to enter human cells. The structural analogies between heparin and HS may result in competitive inhibition, where heparin and related compounds compete with the cell surface HS for viral binding to target cells, 68 , 69 thus potentially blocking or at least attenuating viral entry. The beneficial effects of heparin‐based therapies are also linked to their inhibition of circulating heparanase enzymatic activity. 32 Heparanase, an endo‐β‐glucuronidase, physiologically cleaves HS chains located in extracellular matrices and on cell surfaces. 32 It is often overexpressed during viral infections and act as a regulator of virus release after replication has occurred, promoting its dissemination. 71 , 72 , 73 , 74 Additionally, it may be upregulated by pro‐inflammatory molecules such as IL‐1 and TNF‐α. Once activated, heparanase stimulates the expression and release of pro‐inflammatory cytokines, including TNF‐α, IL‐1 and IL‐6. 75 The enzyme has been implicated in cancer progression, inflammation, 76 VOD/SOS development 77 and other vascular pathologies. 71
Currently, numerous clinical trials are underway to investigate the therapeutic potential of intravenous and subcutaneous heparin, as well as the appropriate dose regimen in COVID‐19. Further, nebulised heparin delivered directly to the airways may be effective in preventing infection and mitigating lung disease (clinicaltrials.gov; NCT04545541, NCT04511923). Notwithstanding their anticoagulant, anti‐inflammatory and anti‐viral properties, the use of heparins is associated with a substantially increased risk of systemic bleeding, and other challenging ‘off‐target’ effects, making its use potentially part of the standard of care, but not without qualification, as well as highlighting the need for combination approaches.
Defibrotide
The use of defibrotide (DF), which has both comparable but distinct properties from heparins and negligible haemorrhagic risk 78 may therefore be warranted, especially given the established propensity for the development of DIC later in the COVID‐19 clinical course. DF is a naturally derived, complex mixture of poly‐deoxyribonuleotides extracted originally from bovine lung and now exclusively from porcine gut mucosa. 79 , 80 Since its original isolation >30 years ago, DF has demonstrated locally acting pro‐fibrinolytic, 81 , 82 , 83 , 84 anti‐thrombotic, 85 , 86 anti‐ischaemic and anti‐inflammatory activities, which exert protective effects on small vessel endothelia. It is currently approved for the treatment of paediatric and adult hepatic VOD/SOS with MOF. 87 , 88 , 89 In this setting, DF has demonstrated efficacy and safety in critically ill patients with MOF, as well as a significant reduction in PAI‐1 and other markers of endothelial stress in patients with VOD/SOS and MOF successfully treated with DF. 89 , 90 , 91 Furthermore, in a pivotal Phase III trial, DF prophylaxis reduced the incidence and severity of VOD/SOS in high‐risk children undergoing BMT. 92 In a more recent study, Palomo et al. 93 demonstrated that DF directly interacts with the cell membrane and becomes internalised by ECs, thus providing physical evidence of its endothelial‐protective properties. In particular, DF appears to decrease levels of pro‐inflammatory proteins, such as TNF‐α, 94 IL‐6, vascular endothelial growth factor (VEGF) 95 and to downregulate major histocompatibility complex (MHC) Class I and Class II molecules, 96 , 97 therefore attenuating both the inflammatory and immune responses. Furthermore, it appears to decrease interaction between leucocytes and ECs by downregulating P‐selectin, 98 ICAM‐1 95 and VCAM‐1. 99 Lastly, DF displays potent adenosine agonism. 100 Such activity may be clinically relevant, not least based on substantial improvement observed in an animal model of acute lung injury upon treatment with adenosine receptor agonists. 101
Based on such properties, the use of DF can be reasonably extended to other post‐BMT syndromes and other microangiopathies involving CRS complicating a variety of disease states and treatment modalities, such as chimeric antigen receptor (CAR) T‐cell therapy. 102 Indeed, paediatric and adult patients receiving DF as VOD/SOS prophylaxis also exhibited a reduced incidence of aGvHD, 92 , 103 a finding that is strongly supported by a preclinical model of aGvHD. 99 Additionally, a retrospective survey from paediatric patients treated with DF for transplant‐associated thrombotic microangiopathy showed resolution of clinical disease in 77% of patients. 104 Currently, Phase II studies investigating the use of DF for prevention of transplant‐associated thrombotic microangiopathy and VOD, and in the same context the treatment of ACS are ongoing (clinicaltrials.gov; NCT03384693, NCT03805581, NCT02675959). Notably, DF suppresses the expression of heparanase transcripts, cell surface expression and enzymatic activity, 95 suggesting that DF may have anti‐viral properties, although this remains to be confirmed. 71 , 72 , 73 Heparanase is putatively upregulated by the cytokine storm of advanced COVID‐19 and may contribute to further inflammation, oedema of the microvascular bed and coagulopathy. 28 , 75 , 105 , 106 DF is a potent inhibitor of heparanase in terms of both cell surface and gene expression, and therefore is especially attractive. Furthermore, the therapeutic use of DF in a murine model of IPS significantly improved survival compared to untreated controls by reducing, among other biomarkers, the levels of Ang‐2, 107 which is known to correlate with ARDS and is markedly elevated in critically ill patients with COVID‐19. 38
In addition, ICU‐admitted patients with COVID‐19 may display increased platelet activation and subsequent formation of platelet‐monocyte aggregates upon interaction with P‐selectin, thus stimulating monocyte‐induced inflammation and thrombosis. 22 By reducing P‐selectin and other adhesion molecules expression, DF may inhibit monocyte‐derived inflammatory and pro‐coagulant signals. Lastly and most importantly, DF has also been shown to decrease the activity of p38 MAPK and its pathway, 93 the importance of which is increasingly recognised in the pathogenesis of the COVID‐19 hyperinflammation syndrome and this may be a key therapeutic target in this process. 58 , 108
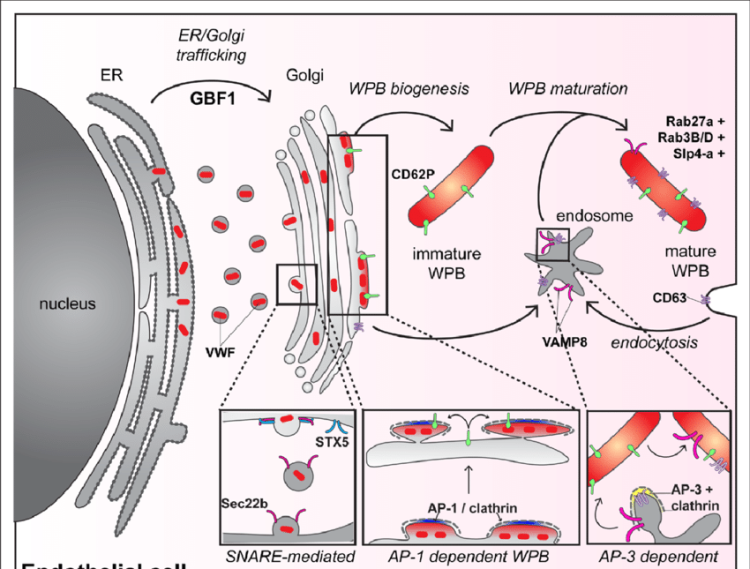
In summary, the multitargeted endothelial‐based therapeutic properties of DF and its relative safety, as well as its regulatory approval, make it an ideal potential therapeutic candidate for the treatment of COVID‐19 vascular complications. 28 In contrast to heparin, DF also exhibits broader anti‐cytokine, anti‐inflammatory and endothelial‐stabilising properties. Importantly, by acting on the heparanase‐HS axis, 74 , 102 DF may limit viral infectivity given its capacity to i) compete with HS and thereby possibly inhibit virus–cell adhesion and entry, ii) inhibit heparanase enzymatic activity and thereby attenuate virus detachment/release and spread 74 and iii) inhibit heparanase‐mediated activation of immune cells and thereby upregulation of pro‐inflammatory cytokines and the associated self‐sustaining systemic inflammatory host response (Fig 1). Actively accruing, international Phase II clinical trials are now underway and should shed critical light on DF’s therapeutic potential in patients with COVID‐19 (examples include clinicaltrials.gov; NCT04348383, NCT04335201). Strikingly, two critically ill paediatric patients treated with DF for a SARS‐CoV‐2‐associated multisystem inflammatory syndrome experienced complete resolution and no attributable toxicity, with correlative studies supporting the mechanistic effects described above, as well as favourable effects seen on complement activation. 109 Similarly, preliminary results from the current studies as part of the international DEFACOVID (Defibrotide as Prevention and Treatment of Respiratory Distress and Cytokine Release Syndrome of COVID‐19) study group support both safety and promising potential efficacy to date.Fig 1
Potential mechanisms of action of defibrotide in the treatment of COVID‐19. Left, defibrotide limits viral attachment by interfering with Syndecan‐1, the primary cell surface heparan sulfate on ECs, and reduces viral dissemination, by inhibiting HPSE‐mediated viral release. Right, effects of defibrotide on endothelial‐mediated pathological processes. Viral infection of ECs promotes apoptosis with breakdown of endothelial barrier and exposure of the subendothelium, with subsequent platelet activation and thrombotic phenomena. Defibrotide inhibits platelet activation and leukocyte recruitment and blocks the generation of the cytokine storm; specifically, HPSE‐mediated activation of immune cells is suppressed, thus limiting the development of cytokine release syndrome. Sars‐Cov‐2, severe acute respiratory syndrome coronavirus‐2; ACE2, angiotensin‐converting enzyme 2; Ang‐2, angiopoietin‐2; GI, gastrointestinal; IL, interleukin; NFKB, nuclear factor kappa‐light chain‐enhancer of activated B cells; TNF‐α, tumor necrosis factor‐alpha; VWF, von Willebrand Factor.
Other heparanase inhibitors
Given the heparanase‐inhibiting activity of heparin, effort has been directed towards modifications of its structure to endow candidate molecules with potentiated anti‐heparanase activity while limiting anticoagulant effects. Specifically, N‐acetylated and glycol‐split heparins are promising agents presenting such characteristics. Indeed, administration of N‐acetylheparin (NAH) in murine models of sepsis ameliorated lung and intestinal injury and subsequent oedema by reducing tissue neutrophilic infiltration and suppressing IL‐6, IL‐1β and TNF‐α production. 110 , 111 Furthermore, roneparstat, the most developed glycol‐split NAH, restored pathological renal cellular damage caused by ischaemia‐reperfusion by reducing release of pro‐inflammatory cytokines and reverted established fibrotic processes, thus restoring normal tissue histology in preclinical models. 112 This aspect is especially relevant, considering the extensive formation of fibrosis and irreversible end‐organ damage in post‐BMT syndromes, SCD and advanced COVID‐19.
Additionally, much interest has been directed towards the novel heparanase‐inhibiting agent pixatimod, a modified oligosaccharide glycoside with heparan sulphate‐mimetic properties. Pixatimod is a potent inhibitor of Type 1 T‐helper cells (Th1)/Th17 effector functions, 113 IL‐6 expression, 114 M2 macrophage activation, 115 angiogenesis and tumour progression in vivo. Furthermore, it exhibits mild anticoagulant activity and despite transient infusion reactions is otherwise generally well tolerated. Guimond et al. 116 have recently demonstrated that pixatimod interacts with the SARS‐CoV‐2 spike protein binding site, and this is coherent with its heparan sulphate‐mimetic activity. Moreover, pixatimod was found to markedly inhibit SARS‐CoV‐2 infectivity, 116 supporting its clinical application as a novel therapeutic intervention for prophylaxis and treatment of COVID‐19. Taken together, heparanase emerges as a host‐encoded virulence factor that once activated enhances viral spread and triggers downstream inflammatory cascades. These preliminary data indicate that heparanase inhibitors currently under development are possible candidates for multisystem inflammatory conditions, such as COVID‐19, sepsis, thrombotic microangiopathies and cancer, but as of now studies remain preclinical with clinical application pending.
Conclusions
In conclusion, increasing evidence suggests that the SARS‐CoV‐2 directly targets ECs, promoting the release of pro‐inflammatory and pro‐thrombotic molecules. Endothelial dysfunction appears to be a crucial initiating step in the pathogenesis of the disease and its ensuing morbidity and mortality. Endotheliitis with the hyperproduction of cytokines leading to CRS, hypercoagulability and thrombotic microangiopathy are hallmarks shared by COVID‐19, VOD/SOS and other endothelial injury syndromes, underpinned by inflammation and including the vaso‐occlusive crises of SCD, so providing a common pathobiology across these respective syndromes. Most importantly, endothelial‐protective agents, such as DF, represent a promising and rational therapeutic strategy in COVID‐19, with DF currently under investigation in a variety of settings and combinations. As a unifying concept, heparanase inhibition, with the modulation of related pathways and other effects on endothelial stress responses may thus be crucial in mediating anti‐viral and anti‐inflammatory activity. In particular, as this relates to endotheliitis, it may directly abrogate CRS and its sequelae, which in turn may lead to improved patient outcome.
Author Contributions
Eleonora Calabretta, Jose M. Moraleda, Israel Vlodavsky, Ruben Jara, Carmelo Carlo‐Stella and Paul Richardson drafted the manuscript; all authors participated in the critical revision and approval of the final report.Go to:
Conflict of interest
Jose M. Moraleda declares Advisory Board fees from Jazz Pharmaceuticals; Antonio Pagliuca has received Advisory Board and Speaker fees from Jazz Pharmaceuticals; Rebecca M. Baron is on a Merck Advisory Board and a Consultant for Genentech. Robert Soiffer serves on the Board of Directors for Kiadis and Be The Match/National Marrow Donor Program; provided consulting for Gilead, Rheos Therapeutics, Cugene, Precision Bioscience, Mana Therapeutics, VOR Biopharma, and Novartis; and Data Safety Monitoring Board for Juno/Celgene; Paul Richardson is an Advisory Committee Member for Jazz Pharmaceuticals; Carmelo Carlo‐Stella is a Consultant/Advisory Board Member for Genente Science srl, ADC Therapeutics, Novartis, Roche, Karyopharm, Sanofi, Boehringer Igelheim and Servier. The remaining authors declare nothing to disclose.
Acknowledgments
This work was supported in part by a grant from the Italian Association for Cancer Research (AIRC, grant #20575 to CC‐S).Go to:
Contributor Information
Carmelo Carlo‐Stella, Email: ue.deminuh@alletsolrac.olemrac.
Paul Richardson, Email: ude.dravrah.icfd@nosdrahcir_luap.Go to:
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. [PMC free article] [PubMed] [Google Scholar]
2. World Health Orgnization (WHO) . Coronavirus disease (COVID‐19) pandemic. Available at: https://www.who.int. Accessed January 2021
3. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. [PMC free article] [PubMed] [Google Scholar]
4. Onder G, Rezza G, Brusaferro S. Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. JAMA. 2020;323:1775–6. [PubMed] [Google Scholar]
5. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81. [PMC free article] [PubMed] [Google Scholar]
6. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in Hospitalized Patients with Covid‐19 – preliminary report. N Engl J Med. 2020. [Online ahead of print]. 10.1056/NEJMoa2021436. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid‐19 – final report. N Engl J Med. 2020;383:1813–26. [PMC free article] [PubMed] [Google Scholar]
8. Siddiqi HK, Mehra MR. COVID‐19 illness in native and immunosuppressed states: a clinical‐therapeutic staging proposal. J Heart Lung Transplant. 2020;39:405–7. [PMC free article] [PubMed] [Google Scholar]
9. Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade‐Long Structural Studies of SARS Coronavirus. J Virol. 2020. [Online ahead of print]. DOI: 10.1128/JVI.00127‐20. [PMC free article] [PubMed] [Google Scholar]
10. Ferrario CM, Trask AJ, Jessup JA. Advances in biochemical and functional roles of angiotensin‐converting enzyme 2 and angiotensin‐(1–7) in regulation of cardiovascular function. Am J Physiol Heart Circ Physiol. 2005;289:H2281–90. [PMC free article] [PubMed] [Google Scholar]
11. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID‐19. Lancet. 2020;395:1417–8. [PMC free article] [PubMed] [Google Scholar]
12. Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, et al. Multiorgan and renal tropism of SARS‐CoV‐2. N Engl J Med. 2020;383:590–2. [PMC free article] [PubMed] [Google Scholar]
13. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid‐19. N Engl J Med. 2020;383:120–8. [PMC free article] [PubMed] [Google Scholar]
14. Stahl K, Gronski PA, Kiyan Y, Seeliger B, Bertram A, Pape T, et al. Injury to the Endothelial Glycocalyx in Critically Ill COVID‐19 Patients. Am J Respir Crit Care Med. 2020. [PMC free article] [PubMed] [Google Scholar]
15. Azouz E, Yang S, Monnier‐Cholley L, Arrivé L. Systemic arterial thrombosis and acute mesenteric ischemia in a patient with COVID‐19. Intensive Care Med. 2020;46:1464–5. [PMC free article] [PubMed] [Google Scholar]
16. Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, et al. Endotheliopathy in COVID‐19‐associated coagulopathy: evidence from a single‐centre, cross‐sectional study. Lancet Haematol. 2020;7:e575–82. [PMC free article] [PubMed] [Google Scholar]
17. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–43. [PMC free article] [PubMed] [Google Scholar]
18. Moore JB, June CH. Cytokine release syndrome in severe COVID‐19. Science. 2020;368:473–4. [PubMed] [Google Scholar]
19. Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T‐cells and inflammatory monocytes incite inflammatory storms in severe COVID‐19 patients. Nati Sci Rev. 2020;7:998–1002. [Google Scholar]
20. Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, et al. Single‐cell landscape of bronchoalveolar immune cells in patients with COVID‐19. Nat Med. 2020;26:842–4. [PubMed] [Google Scholar]
21. Merad M, Martin JC. Pathological inflammation in patients with COVID‐19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–62. [PMC free article] [PubMed] [Google Scholar]
22. Hottz ED, Azevedo‐Quintanilha IG, Palhinha L, Teixeira L, Barreto EA, Pão CRR, et al. Platelet activation and platelet‐monocyte aggregate formation trigger tissue factor expression in patients with severe COVID‐19. Blood. 2020;136:1330–41. [PMC free article] [PubMed] [Google Scholar]
23. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–7. [PMC free article] [PubMed] [Google Scholar]
24. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID‐19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–8. [PMC free article] [PubMed] [Google Scholar]
25. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Investig. 2020;130:2620–9. [PMC free article] [PubMed] [Google Scholar]
26. Price CC, Altice FL, Shyr Y, Koff A, Pischel L, Goshua G, et al. Tocilizumab treatment for cytokine release syndrome in hospitalized COVID‐19 patients: survival and clinical outcomes. Chest. 2020;158:1397–1408. [PMC free article] [PubMed] [Google Scholar]
27. Rosas I, Bräu N, Waters M, Go RC, Hunter BD, Bhagani S, et al. Tocilizumab in hospitalized patients with COVID‐19 pneumonia. medRxiv. 2020;2020.08.27.20183442. [Google Scholar]
28. Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID‐19: the vasculature unleashed. Nat Rev Immunol. 2020;20:389–91. [PMC free article] [PubMed] [Google Scholar]
29. Hildebrandt GC, Chao N. Endothelial cell function and endothelial‐related disorders following haematopoietic cell transplantation. Br J Haematol. 2020;190:508–19. [PMC free article] [PubMed] [Google Scholar]
30. Valla DC, Cazals‐Hatem D. Sinusoidal obstruction syndrome. Clin Res Hepatol Gastroenterol. 2016;40:378–85. [PubMed] [Google Scholar]
31. Richardson PG, Corbacioglu S, Ho VT, Kernan NA, Lehmann L, Maguire C, et al. Drug safety evaluation of defibrotide. Expert Opin Drug Saf. 2013;12:123–36. [PubMed] [Google Scholar]
32. Vlodavsky I, Ilan N, Sanderson RD. Forty years of basic and translational heparanase research. Adv Exp Med Biol. 2020;1221:3–59. [PMC free article] [PubMed] [Google Scholar]
33. Coppell JA, Richardson PG, Soiffer R, Martin PL, Kernan NA, Chen A, et al. Hepatic veno‐occlusive disease following stem cell transplantation: incidence, clinical course, and outcome. Biol Blood Marrow Transplant. 2010;16:157–68. [PMC free article] [PubMed] [Google Scholar]
34. Bunte MC, Patnaik MM, Pritzker MR, Burns LJ. Pulmonary veno‐occlusive disease following hematopoietic stem cell transplantation: a rare model of endothelial dysfunction. Bone Marrow Transplant. 2008;41:677–86. [PubMed] [Google Scholar]
35. Mandel J, Mark EJ, Hales CA. Pulmonary veno‐occlusive disease. Am J Respir Crit Care Med. 2000;162:1964–73. [PubMed] [Google Scholar]
36. Altmann T, Slack J, Slatter MA, O’Brien C, Cant A, Thomas M, et al. Endothelial cell damage in idiopathic pneumonia syndrome. Bone Marrow Transplant. 2018;53:515–8. [PubMed] [Google Scholar]
37. Ando M, Miyazaki E, Abe T, Ehara C, Goto A, Masuda T, et al. Angiopoietin‐2 expression in patients with an acute exacerbation of idiopathic interstitial pneumonias. Respir Med. 2016;117:27–32. [PubMed] [Google Scholar]
38. Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, et al. Angiopoietin‐2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID‐19 patients. Angiogenesis. 2020;23:611–20. [PMC free article] [PubMed] [Google Scholar]
39. Batts ED, Lazarus HM. Diagnosis and treatment of transplantation‐associated thrombotic microangiopathy: real progress or are we still waiting? Bone Marrow Transplant. 2007;40:709–19. [PubMed] [Google Scholar]
40. Seaby EG, Gilbert RD. Thrombotic microangiopathy following haematopoietic stem cell transplant. Pediatr Nephrol. 2018;33(9):1489–500. [PMC free article] [PubMed] [Google Scholar]
41. Ghimire S, Weber D, Mavin E, Wang XN, Dickinson AM, Holler E. Pathophysiology of GvHD and Other HSCT‐related major complications. Front Immunol. 2017;8:79. [PMC free article] [PubMed] [Google Scholar]
42. Seidel C, Ringdén O, Remberger M. Increased levels of syndecan‐1 in serum during acute graft‐versus‐host disease. Transplantation. 2003;76:423–6. [PubMed] [Google Scholar]
43. Holtan SG, Pasquini M, Weisdorf DJ. Acute graft‐versus‐host disease: a bench‐to‐bedside update. Blood. 2014;124:363–73. [PMC free article] [PubMed] [Google Scholar]
44. Riesner K, Shi Y, Jacobi A, Kräter M, Kalupa M, McGearey A, et al. Initiation of acute graft‐versus‐host disease by angiogenesis. Blood. 2017;129:2021–32. [PubMed] [Google Scholar]
45. Mir E, Palomo M, Rovira M, Pereira A, Escolar G, Penack O, et al. Endothelial damage is aggravated in acute GvHD and could predict its development. Bone Marrow Transplant. 2017;52:1317–25. [PubMed] [Google Scholar]
46. Dietrich S, Falk CS, Benner A, Karamustafa S, Hahn E, Andrulis M, et al. Endothelial vulnerability and endothelial damage are associated with risk of graft‐versus‐host disease and response to steroid treatment. Biol Blood Marrow Transplant. 2013;19:22–7. [PubMed] [Google Scholar]
47. Choi SW, Kitko CL, Braun T, Paczesny S, Yanik G, Mineishi S, et al. Change in plasma tumor necrosis factor receptor 1 levels in the first week after myeloablative allogeneic transplantation correlates with severity and incidence of GVHD and survival. Blood. 2008;112:1539–42. [PMC free article] [PubMed] [Google Scholar]
48. Conran N, Belcher JD. Inflammation in sickle cell disease. Clin Hemorheol Microcirc. 2018;68:263–99. [PMC free article] [PubMed] [Google Scholar]
49. Pathare A, Al Kindi S, Alnaqdy AA, Daar S, Knox‐Macaulay H, Dennison D. Cytokine profile of sickle cell disease in Oman. Am J Hematol. 2004;77:323–8. [PubMed] [Google Scholar]
50. Sakamoto TM, Lanaro C, Ozelo MC, Garrido VT, Olalla‐Saad ST, Conran N, et al. Increased adhesive and inflammatory properties in blood outgrowth endothelial cells from sickle cell anemia patients. Microvasc Res. 2013;90:173–9. [PubMed] [Google Scholar]
51. Duits AJ, Pieters RC, Saleh AW, van Rosmalen E, Katerberg H, Berend K, et al. Enhanced levels of soluble VCAM‐1 in sickle cell patients and their specific increment during vasoocclusive crisis. Clin Immunol Immunopathol. 1996;81:96–8. [PubMed] [Google Scholar]
52. Embury SH, Matsui NM, Ramanujam S, Mayadas TN, Noguchi CT, Diwan BA, et al. The contribution of endothelial cell P‐selectin to the microvascular flow of mouse sickle erythrocytes in vivo. Blood. 2004;104:3378–85. [PubMed] [Google Scholar]
53. Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–44. [PubMed] [Google Scholar]
54. Anea CB, Lyon M, Lee IA, Gonzales JN, Adeyemi A, Falls G, et al. Pulmonary platelet thrombi and vascular pathology in acute chest syndrome in patients with sickle cell disease. Am J Hematol. 2016;91:173–8. [PMC free article] [PubMed] [Google Scholar]
55. Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID‐19: a post‐mortem study. Lancet. Microbe. 2020;1:e245–53. [PMC free article] [PubMed] [Google Scholar]
56. James J, Srivastava A, Varghese MV, Eccles CA, Zemskova M, Rafikova O, et al. Heme induces rapid endothelial barrier dysfunction via the MKK3/p38MAPK axis. Blood. 2020;136:749–54. [PMC free article] [PubMed] [Google Scholar]
57. Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, et al. Angiotensin‐Converting Enzyme 2: SARS‐CoV‐2 Receptor and Regulator of the Renin‐Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020;126:1456–74. [PMC free article] [PubMed] [Google Scholar]
58. Grimes JM, Grimes KV. p38 MAPK inhibition: a promising therapeutic approach for COVID‐19. J Mol Cell Cardiol. 2020;144:63–5. [PMC free article] [PubMed] [Google Scholar]
59. Schots R, Kaufman L, Van Riet I, Ben Othman T, De Waele M, Van Camp B, et al. Proinflammatory cytokines and their role in the development of major transplant‐related complications in the early phase after allogeneic bone marrow transplantation. Leukemia. 2003;17:1150–6. [PubMed] [Google Scholar]
60. Gugliotta L, Catani L, Vianelli N, Gherlinzoni F, Miggiano MC, Bandini G, et al. High plasma levels of tumor necrosis factor‐alpha may be predictive of veno‐occlusive disease in bone marrow transplantation. Blood. 1994;83:2385–6. [PubMed] [Google Scholar]
61. Symington FW, Symington BE, Liu PY, Viguet H, Santhanam U, Sehgal PB. The relationship of serum IL‐6 levels to acute graft‐versus‐host disease and hepatorenal disease after human bone marrow transplantation. Transplantation. 1992;54:457–62. [PubMed] [Google Scholar]
62. Remberger M, Ringden O. Serum levels of cytokines after bone marrow transplantation: increased IL‐8 levels during severe veno‐occlusive disease of the liver. Eur J Haematol. 1997;59:254–62. [PubMed] [Google Scholar]
63. Palomo M, Diaz‐Ricart M, Rovira M, Escolar G, Carreras E. Defibrotide prevents the activation of macrovascular and microvascular endothelia caused by soluble factors released to blood by autologous hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2011;17:497–506. [PubMed] [Google Scholar]
64. Li X, Ma X. The role of heparin in sepsis: much more than just an anticoagulant. Br J Haematol. 2017;179:389–98. [PubMed] [Google Scholar]
65. Shi C, Wang C, Wang H, Yang C, Cai F, Zeng F, et al. The potential of low molecular weight heparin to mitigate cytokine storm in severe COVID‐19 patients: a retrospective clinical study. Clin Transl Sci. 2020;13:1087–95. [PMC free article] [PubMed] [Google Scholar]
66. Lindahl U, Li JP. Heparin – an old drug with multiple potential targets in Covid‐19 therapy. J Thromb Haemost. 2020;18:2422–2424. [PMC free article] [PubMed] [Google Scholar]
67. Agelidis A, Deepak S. Heparanase, heparan sulfate and viral infection. Adv Exp Med Biol. 2020;1221:759–70. [PubMed] [Google Scholar]
68. Mycroft‐West C, Su D, Elli S, Guimond S, Miller G, Turnbull J, et al.The 2019 coronavirus (SARS‐CoV‐2) surface protein (Spike) S1 receptor binding domain undergoes conformational change upon heparin binding. bioRxiv 2020; 2020.02.29.971093.
69. Hondermarck H, Bartlett NW, Nurcombe V. The role of growth factor receptors in viral infections: an opportunity for drug repurposing against emerging viral diseases such as COVID‐19? FASEB Bioadv. 2020;2:296–303. [PMC free article] [PubMed] [Google Scholar]
70. Clausen TM, Sandoval DR, Spliid CB, Pihl J, Perrett HR, Painter CD, et al. SARS‐CoV‐2 infection depends on cellular heparan sulfate and ACE2. Cell. 2020;183:1043–57. [PMC free article] [PubMed] [Google Scholar]
71. Khanna M, Ranasinghe C, Browne AM, Li JP, Vlodavsky I, Parish CR. Is host heparanase required for the rapid spread of heparan sulfate binding viruses? Virology. 2019;529:1–6. [PubMed] [Google Scholar]
72. Hadigal SR, Agelidis AM, Karasneh GA, Antoine TE, Yakoub AM, Ramani VC, et al. Heparanase is a host enzyme required for herpes simplex virus‐1 release from cells. Nat Commun. 2015;6:6985. [PMC free article] [PubMed] [Google Scholar]
73. Agelidis AM, Hadigal SR, Jaishankar D, Shukla D. Viral activation of Heparanase drives pathogenesis of herpes simplex virus‐1. Cell Rep. 2017;20:439–50. [PMC free article] [PubMed] [Google Scholar]
74. Koganti R, Suryawanshi R, Shukla D. Heparanase, cell signaling, and viral infections. Cell Mol Life Sci. 2020;77:5059–77. [PMC free article] [PubMed] [Google Scholar]
75. Goodall KJ, Poon IK, Phipps S, Hulett MD. Soluble heparan sulfate fragments generated by heparanase trigger the release of pro‐inflammatory cytokines through TLR‐4. PLoS One. 2014;9:e109596. [PMC free article] [PubMed] [Google Scholar]
76. Mayfosh AJ, Baschuk N, Hulett MD. Leukocyte heparanase: a double‐edged sword in tumor progression. Front Oncol. 2019;9:331. [PMC free article] [PubMed] [Google Scholar]
77. Seifert C, Wittig S, Arndt C, Gruhn B. Heparanase polymorphisms: influence on incidence of hepatic sinusoidal obstruction syndrome in children undergoing allogeneic hematopoietic stem cell transplantation. J Cancer Res Clin Oncol. 2015;141:877–85. [PubMed] [Google Scholar]
78. Palmer KJ, Defibrotide GK. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in vascular disorders. Drugs. 1993;45:259–94. [PubMed] [Google Scholar]
79. Thiemermann C, Thomas GR, Vane JR. Defibrotide reduces infarct size in a rabbit model of experimental myocardial ischaemia and reperfusion. Br J Pharmacol. 1989;97:401–8. [PMC free article] [PubMed] [Google Scholar]
80. Stein C, Castanotto D, Krishnan A, Nikolaenko L. Defibrotide (Defitelio): a new addition to the stockpile of food and drug administration‐approved oligonucleotide drugs. Mol Ther Nucleic Acids. 2016;5:e346. [PMC free article] [PubMed] [Google Scholar]
81. Pescador R, Mantovani M, Prino G, Madonna M. Pharmacokinetics of Defibrotide and of its profibrinolytic activity in the rabbit. Thromb Res. 1983;30:1–11. [PubMed] [Google Scholar]
82. Falanga A, Vignoli A, Marchetti M, Barbui T. Defibrotide reduces procoagulant activity and increases fibrinolytic properties of endothelial cells. Leukemia. 2003;17:1636–42. [PubMed] [Google Scholar]
83. Cella G, Sbarai A, Mazzaro G, Motta G, Carraro P, Andreozzi GM, et al. Tissue factor pathway inhibitor release induced by defibrotide and heparins. Clin Appl Thromb Hemost. 2001;7:225–8. [PubMed] [Google Scholar]
84. Echart CL, Graziadio B, Somaini S, Ferro LI, Richardson PG, Fareed J, et al. The fibrinolytic mechanism of defibrotide: effect of defibrotide on plasmin activity. Blood Coagul Fibrinolysis. 2009;20:627–34. [PubMed] [Google Scholar]
85. Niada R, Mantovani M, Prino G, Pescador R, Berti F, Omini C, et al. Antithrombotic activity of a polydeoxyribonucleotidic substance extracted from mammalian organs: a possible link with prostacyclin. Thromb Res. 1981;23:233–46. [PubMed] [Google Scholar]
86. Francischetti IM, Oliveira CJ, Ostera GR, Yager SB, Debierre‐Grockiego F, Carregaro V, et al. Defibrotide interferes with several steps of the coagulation‐inflammation cycle and exhibits therapeutic potential to treat severe malaria. Arterioscler Thromb Vasc Biol. 2012;32:786–98. [PMC free article] [PubMed] [Google Scholar]
87. U.S. Food & Drug Administration (FDA) . Defitelio (defibrotide sodium). Available at: https://www.fda.gov/drugs/resources‐information‐approved‐drugs/defitelio‐defibrotide‐sodium. Accessed January 2021
88. Richardson PG, Riches ML, Kernan NA, Brochstein JA, Mineishi S, Termuhlen AM, et al. Phase 3 trial of defibrotide for the treatment of severe veno‐occlusive disease and multi‐organ failure. Blood. 2016;127:1656–65. [PMC free article] [PubMed] [Google Scholar]
89. Richardson PG, Grupp SA, Pagliuca A, Krishnan A, Ho VT, Corbacioglu S. Defibrotide for the treatment of hepatic veno‐occlusive disease/sinusoidal obstruction syndrome with multiorgan failure. Int J Hematol Oncol. 2017;6:75–93. [PMC free article] [PubMed] [Google Scholar]
90. Richardson PG, Soiffer RJ, Antin JH, Uno H, Jin Z, Kurtzberg J, et al. Defibrotide for the treatment of severe hepatic veno‐occlusive disease and multiorgan failure after stem cell transplantation: a multicenter, randomized, dose‐finding trial. Biol Blood Marrow Transplant. 2010;16:1005–17. [PMC free article] [PubMed] [Google Scholar]
91. Richardson PG, Murakami C, Jin Z, Warren D, Momtaz P, Hoppensteadt D, et al. Multi‐institutional use of defibrotide in 88 patients after stem cell transplantation with severe veno‐occlusive disease and multisystem organ failure: response without significant toxicity in a high‐risk population and factors predictive of outcome. Blood. 2002;100:4337–43. [PubMed] [Google Scholar]
92. Corbacioglu S, Cesaro S, Faraci M, Valteau‐Couanet D, Gruhn B, Rovelli A, et al. Defibrotide for prophylaxis of hepatic veno‐occlusive disease in paediatric haemopoietic stem‐cell transplantation: an open‐label, phase 3, randomised controlled trial. Lancet. 2012;379:1301–9. [PubMed] [Google Scholar]
93. Palomo M, Mir E, Rovira M, Escolar G, Carreras E, Diaz‐Ricart M. What is going on between defibrotide and endothelial cells? Snapshots reveal the hot spots of their romance. Blood. 2016;127:1719–27. [PMC free article] [PubMed] [Google Scholar]
94. Schröder H. Defibrotide protects endothelial cells, but not L929 tumour cells, from tumour necrosis factor‐alpha‐mediated cytotoxicity. J Pharm Pharmacol. 1995;47:250–2. [PubMed] [Google Scholar]
95. Mitsiades CS, Rouleau C, Echart C, Menon K, Teicher B, Distaso M, et al. Preclinical studies in support of defibrotide for the treatment of multiple myeloma and other neoplasias. Clin Cancer Res. 2009;15:1210–21. [PMC free article] [PubMed] [Google Scholar]
96. Eissner G, Multhoff G, Gerbitz A, Kirchner S, Bauer S, Haffner S, et al. Fludarabine induces apoptosis, activation, and allogenicity in human endothelial and epithelial cells: protective effect of defibrotide. Blood. 2002;100:334–40. [PubMed] [Google Scholar]
97. Ferraresso M, Rigotti P, Stepkowski SM, Chou TC, Kahan BD. Immunosuppressive effects of defibrotide. Transplantation. 1993;56:928–33. [PubMed] [Google Scholar]
98. Scalia R, Kochilas L, Campbell B, Lefer AM. Effects of defibrotide on leukocyte‐endothelial cell interaction in the rat mesenteric vascular bed: role of P‐selectin. Methods Find Exp Clin Pharmacol. 1996;18:669–76. [PubMed] [Google Scholar]
99. García‐Bernal D, Palomo M, Martínez CM, Millán‐Rivero JE, García‐Guillén AI, Blanquer M, et al. Defibrotide inhibits donor leucocyte‐endothelial interactions and protects against acute graft‐versus‐host disease. J Cell Mol Med. 2020;24:8031–44. [PMC free article] [PubMed] [Google Scholar]
100. Bianchi G, Barone D, Lanzarotti E, Tettamanti R, Porta R, Moltrasio D, et al. Defibrotide, a single‐stranded polydeoxyribonucleotide acting as an adenosine receptor agonist. Eur J Pharmacol. 1993;238:327–34. [PubMed] [Google Scholar]
101. Ko IG, Hwang JJ, Chang BS, Kim SH, Jin JJ, Hwang L, et al. Polydeoxyribonucleotide ameliorates lipopolysaccharide‐induced acute lung injury via modulation of the MAPK/NF‐κB signaling pathway in rats. Int Immunopharmacol. 2020;83:106444. [PubMed] [Google Scholar]
102. Richardson PG, Carreras E, Iacobelli M, Nejadnik B. The use of defibrotide in blood and marrow transplantation. Blood Adv. 2018;2:1495–509. [PMC free article] [PubMed] [Google Scholar]
103. Tekgündüz E, Kaya AH, Bozdağ SC, Koçubaba Ş, Kayıkçı Ö, Namdaroğlu S, et al. Does defibrotide prophylaxis decrease the risk of acute graft versus host disease following allogeneic hematopoietic cell transplantation? Transfus Apher Sci. 2016;54:30–4. [PubMed] [Google Scholar]
104. Yeates L, Slatter MA, Bonanomi S, Lim FL, Ong SY, Dalissier A, et al. Use of defibrotide to treat transplant‐associated thrombotic microangiopathy: a retrospective study of the Paediatric Diseases and Inborn Errors Working Parties of the European Society of Blood and Marrow Transplantation. Bone Marrow Transplant. 2017;52:762–4. [PubMed] [Google Scholar]
105. Nadir Y. Heparanase in the coagulation system. Adv Exp Med Biol. 2020;1221:771–84. [PubMed] [Google Scholar]
106. Buijsers B, Yanginlar C, Grondman I, de Nooijer A, Maciej‐Hulme ML, Jonkman I, et al. Increased plasma heparanase activity in COVID‐19 patients. medRxiv. 2020;2020.06.12.20129304. [PMC free article] [PubMed] [Google Scholar]
107. Klein OR, Choi S, Haile A, Ktena YP, Pierce E, Smith M, et al. Defibrotide Modulates Pulmonary Endothelial Cell Activation and Protects Against Lung Inflammation in Pre‐Clinical Models of LPS‐Induced Lung Injury and Idiopathic Pneumonia. Syndrome. 2020;26:S138–9. [Google Scholar]
108. Richardson E, Carlo‐Stella C, Jara R, Vlodavsky I, Iacobelli M, Fareed J, et al. Response to Maccio et al., “Multifactorial Pathogenesis of COVID‐19‐related Coagulopathy: Can defibrotide have a role in the early phases of coagulation disorders?. J Thromb Haemost. 2020;18:3111–3. [PubMed] [Google Scholar]
109. Lang P, Eichholz T, Bakchoul T, Streiter M, Petrasch M, Bösmüller H, et al. Defibrotide for the treatment of PIMS‐TS in two pediatric patients. J Pediatr Infect Dis Soc. 2020;9:622–5. [Google Scholar]
110. Chen S, He Y, Hu Z, Lu S, Yin X, Ma X, et al. Heparanase Mediates Intestinal Inflammation and Injury in a Mouse Model of Sepsis. J Histochem Cytochem. 2017;65:241–9. [PMC free article] [PubMed] [Google Scholar]
111. Huang X, Han S, Liu X, Wang T, Xu H, Xia B, et al. Both UFH and NAH alleviate shedding of endothelial glycocalyx and coagulopathy in LPS‐induced sepsis. Exp Ther Med. 2020;19:913–22. [PMC free article] [PubMed] [Google Scholar]
112. Masola V, Bellin G, Vischini G, Dall’Olmo L, Granata S, Gambaro G, et al. Inhibition of heparanase protects against chronic kidney dysfunction following ischemia/reperfusion injury. Oncotarget. 2018;9:36185–201. [PMC free article] [PubMed] [Google Scholar]
113. Koliesnik IO, Kuipers HF, Medina CO, Zihsler S, Liu D, Van Belleghem JD, et al. The heparan sulfate mimetic PG545 modulates T cell responses and prevents delayed‐type hypersensitivity. Front Immunol. 2020;11:132. [PMC free article] [PubMed] [Google Scholar]
114. Abassi Z, Hamoud S, Hassan A, Khamaysi I, Nativ O, Heyman SN, et al. Involvement of heparanase in the pathogenesis of acute kidney injury: nephroprotective effect of PG545. Oncotarget. 2017;8:34191–204. [PMC free article] [PubMed] [Google Scholar]
115. Ostapoff KT, Awasthi N, Cenik BK, Hinz S, Dredge K, Schwarz RE, et al. PG545, an angiogenesis and heparanase inhibitor, reduces primary tumor growth and metastasis in experimental pancreatic cancer. Mol Cancer Ther. 2013;12:1190–201. [PubMed] [Google Scholar]
116. Guimond SE, Mycroft‐West CJ, Gandhi NS, Tree JA, Buttigieg KR, Coombes N, et al. Pixatimod (PG545), a clinical‐stage heparan sulfate mimetic, is a potent inhibitor of the SARS‐CoV‐2 virus. bioRxiv. 2020;2020.06.24.169334. [Google Scholar]