Authors: Georgios Tsivgoulis, Lina Palaiodimou, Ramin Zand
First Published December 8, 2020 Review Article Find in PubMed https://doi.org /10.1177/1756286420978004
Abstract
Neurological manifestations are not uncommon during infection with the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A clear association has been reported between cerebrovascular disease and coronavirus disease 2019 (COVID-19). However, whether this association is causal or incidental is still unknown. In this narrative review, we sought to present the possible pathophysiological mechanisms linking COVID-19 and cerebrovascular disease, describe the stroke syndromes and their prognosis and discuss several clinical, radiological, and laboratory characteristics that may aid in the prompt recognition of cerebrovascular disease during COVID-19. A systematic literature search was conducted, and relevant information was abstracted. Angiotensin-converting enzyme-2 receptor dysregulation, uncontrollable immune reaction and inflammation, coagulopathy, COVID-19-associated cardiac injury with subsequent cardio-embolism, complications due to critical illness and prolonged hospitalization can all contribute as potential etiopathogenic mechanisms leading to diverse cerebrovascular clinical manifestations. Acute ischemic stroke, intracerebral hemorrhage, and cerebral venous sinus thrombosis have been described in case reports and cohorts of COVID-19 patients with a prevalence ranging between 0.5% and 5%. SARS-CoV-2-positive stroke patients have higher mortality rates, worse functional outcomes at discharge and longer duration of hospitalization as compared with SARS-CoV-2-negative stroke patients in different cohort studies. Specific demographic, clinical, laboratory and radiological characteristics may be used as ‘red flags’ to alarm clinicians in recognizing COVID-19-related stroke.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and has been declared as a Public Health Emergency of International Concern by the World Health Organization.1 Since its outbreak in December 2019, SARS-CoV-2 has spread in more than 235 countries, and as of 25 September 2020, it has infected 32,029,704 patients.2 Characteristically, COVID-19 affects the respiratory system, producing symptoms ranging from mild upper-airway manifestations to pneumonia and severe acute respiratory distress syndrome.3 COVID-19 is increasingly recognized as a multi-system disease with apparent involvement of other organ systems and clinical gastrointestinal, cardiological, dermatological and other extrapulmonary manifestations.4–8
COVID-19 affection of the nervous system has also been reported, including both the central nervous system (CNS) and peripheral nervous system (PNS).9 A growing number of case series and cohort studies have been published identifying neurological symptoms associated with COVID-19. CNS manifestations may include headache, dizziness, seizures, confusion, delirium, and coma. PNS involvement may be presented as hypogeusia, hyposmia, other cranial neuropathies or generalized weakness due to Guillain–Barré and intensive-care-unit-acquired polyneuropathy or myopathy.
In the first case series reporting on the neurological manifestations of COVID-19, cerebrovascular disease was reported with a higher prevalence in COVID-19 patients who were more seriously infected.10 Since then, multiple studies have been published, arguing whether there is a causal or coincidental relationship between COVID-19 and cerebrovascular disease.
In this narrative review, we present the possible pathophysiological mechanisms linking cerebrovascular disease and COVID-19, describe the clinical syndromes and their prognosis and provide a ‘red flag’ system to alert clinicians for prompt recognition of cerebrovascular disease during COVID-19.
Methods
We systematically searched the literature through MEDLINE and EMBASE, using the following keywords and their combination: SARS-CoV-2, COVID-19, cerebrovascular disease, stroke, ischemic stroke, intracranial hemorrhage, subarachnoid hemorrhage, cerebral venous thrombosis, cerebral sinus, and vein thrombosis. We evaluated only peer-reviewed articles that had been published or had been officially accepted for publication. References of retrieved articles were also screened. Case reports, case series, editorials, reviews, case-control, and cohort studies were evaluated, and relevant information was abstracted. The literature search protocol was conducted by three independent authors (GT, LP, and AHK). The last literature search was conducted on 1 September 2020. Characteristic images of cerebrovascular disease manifestations in COVID-19 patients have been provided by co-authors using previously unpublished data from COVID-19 tertiary care referral centers from Europe, North America, and Asia.
Results
Possible pathophysiological mechanisms linking cerebrovascular disease and COVID-19
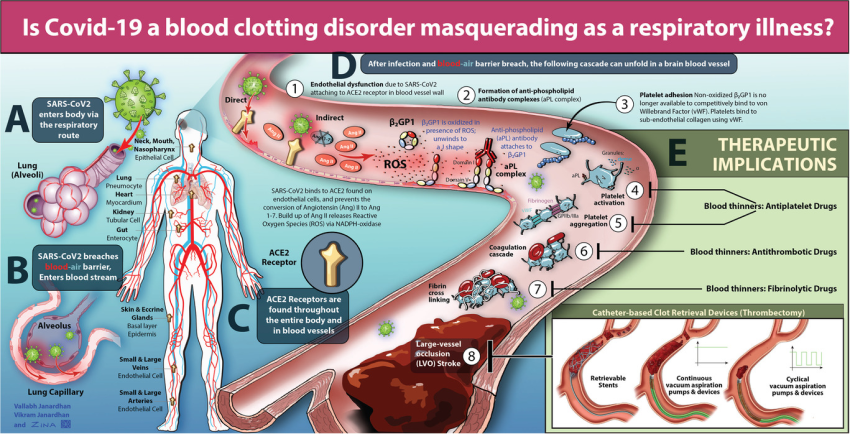
Several common cerebrovascular risk factors have been associated with severe COVID-19 as well, including cardiovascular disease, diabetes mellitus, hypertension, smoking, advanced age, and previous history of stroke.11 This raises the question whether their relationship is causal or if they just coincide. Several possible pathophysiological mechanisms have been recently described (Figure 1).
Figure 1. Potential pathophysiological mechanisms underlying cerebrovascular involvement in COVID-19.
SARS-CoV-2 binds to angiotensin-converting enzyme 2 (ACE2) receptors, leading to the receptors’ inactivation. ACE2 dysregulation contributes to the post-ischemic inflammation cascade, resulting in decreased perfusion in the ischemic zone and the development of larger infarct volume in the case of ischemic stroke (IS). In addition, ACE2 dysfunction may subsequently cause hypertensive peaks and impairment of cerebrovascular endothelium, contributing to the pathogenesis of intracerebral hemorrhage (ICH). Virus-related cardiac injury, including myocardial ischemia and cardiac arrhythmias such as atrial fibrillation, may cause cardio-embolism and subsequently, IS. COVID-19-related hypercoagulability may determine in situ arterial thrombosis and IS. Another potential IS mechanism related to hypercoagulability is paradoxical emboli of generated venous thrombi through right-to-left shunts. Cerebral venous thrombosis may also be caused by hypercoagulability and in situ thrombosis. Furthermore, COVID-19-related coagulopathy may present as dysfunctional hemostasis and predispose to ICH, especially when therapeutic anticoagulation is administered. Cytokine storm-mediated endotheliitis and vasculitis of the CNS due to SARS-CoV-2 infection causes vessel remodeling, leading to vessel occlusion or injury and IS or ICH, respectively. Finally, a primarily immune-mediated critical illness during COVID-19, hypoxemia, and systemic hypotension may induce hypoxic/ischemic encephalopathy or cerebral microbleeds with or without leukoencephalopathy.
CNS, central nervous system; COVID-19, coronavirus disease 2019; DVT, deep venous thrombosis; PE, pulmonary embolism; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Targeting angiotensin-converting enzyme 2 (ACE2) receptor
SARS-CoV-2 is known to bind to the ACE2 receptor, causing the inactivation of the receptor and leading to dysfunction in blood pressure regulation.12,13 In turn, this could lead to hypertensive peaks that could be particularly important in the pathogenesis of intracerebral hemorrhage (ICH). However, data to date have suggested that patients with ICH and COVID-19 present with lower systolic blood pressure, relative to spontaneous ICH.14 Furthermore, ACE2 dysregulation may also contribute to the post-ischemic inflammation cascade through the accumulation of angiotensin 2, resulting in decreased perfusion in the ischemic zone and the development of larger infarct volumes.15,16 The impaired endothelial function in cerebral arteries caused by ACE2 inactivation has also been implicated in the pathogenesis of cerebrovascular events, including both ischemic and hemorrhagic stroke.17,18
Cardiovascular complications associated with COVID-19
Virus-related cardiac injury in patients with COVID-19 has been associated with ACE2 dysregulation, imbalanced immune response leading to cytokine storm, hypoxia related to respiratory dysfunction and treatment-adverse events.6 Specifically, SARS-CoV-2 infection can be complicated with decompensated heart failure, myocarditis, acute myocardial infarction and cardiac arrhythmias, including incident atrial fibrillation.6,19,20 The aforementioned cardiac manifestations of COVID-19 may lead to subsequent cardio-embolism and cerebral infarction.
Coagulopathy associated with COVID-19
Various reports have been published regarding hypercoagulability associated with severe COVID-19 illness, due to immobilization, dehydration, inflammation, elevated fibrinogen, endothelial cell injury, and platelet activation.21–24 The hypercoagulability may further add to the risk of developing cerebral venous thrombosis (CVT) or ischemic stroke (IS).23–25 The COVID-19-associated prothrombotic state is accompanied by high D-dimer levels, elevated ferritin, and in some cases, detectable lupus anticoagulant, anticardiolipin immunoglobulin A (IgA), and antiphospholipid IgA and immunoglobulin M (IgM) autoantibodies directed against β2-glycoprotein-1.22,26 On the other hand, it is well established that such autoantibodies appear in many conditions characterized by profound immune activation with no apparent pathogenic role.
Hypercoagulability due to SARS-CoV-2 infection has also been associated with a higher incidence of deep vein thrombosis.27,28 Right-to-left shunt and paradoxical embolism of generated venous thrombi through a patent foramen ovale might act as an etiopathogenic mechanism in younger patients with cryptogenic cerebral ischemia without any vascular risk factors for stroke. In addition to intracardiac shunts, the right-to-left shunt may be associated with intrapulmonary causes, such as pulmonary vascular dilatations or pulmonary arteriovenous malformations. In a recently published study, contrast-enhanced transcranial Doppler was performed in mechanically ventilated patients with COVID-19 pneumonia and detected microbubbles in 83% of the patients.29 The detection of microbubbles was attributable to pulmonary vasodilatations which may also explain the disproportionate hypoxemia seen in COVID-19 patients.29
On the other hand, coagulopathy associated with COVID-19 may present as dysfunctional hemostasis, prolonged prothrombin time and bleeding disorder, especially in severely infected patients. The characteristics of COVID-19 coagulopathy are similar but not perfectly matched to those of disseminated intravascular coagulopathy.30 Characteristically, COVID-19 coagulopathy manifests with significantly elevated D-dimers, but only mild thrombocytopenia and slightly prolonged prothrombin time, and rarely meets the diagnostic criteria of disseminated intravascular coagulopathy according to the International Society on Thrombosis and Haemostasis.31,32 Nevertheless, the disruption of hemostasis in COVID-19 may contribute to an increased risk of secondary intracranial hemorrhage, especially when therapeutic anticoagulation is also administered.
Triggering CNS vasculitis and endotheliitis
SARS-CoV-2 viral-like particles may be detected in brain capillary endothelium, as was recently noted in an autopsy study.33 This finding supports the viral neurotropism and potentially implicates SARS-CoV-2 in a direct effect on cerebral vessels with subsequent endothelium dysfunction and degeneration.34 SARS-CoV-2 has also been implicated in triggering CNS vasculitis, possibly through an inflammatory response mediated by the cytokine storm and specifically interleukin-6.35–38 This is not new for viral infections, since other viruses (e.g. varicella zoster, human immunodeficiency virus, hepatitis C virus, hepatitis B, cytomegalovirus, parvovirus b19) may trigger such a response.39 Inflammation of cerebral vasculature may lead to arterial remodeling with either stenosed or dilated, fragile vessels with subsequent ischemic or hemorrhagic stroke, respectively. Reversible cerebral vasoconstriction syndrome and posterior reversible encephalopathy syndrome may mimic primary angiitis of the CNS and have been recently described in COVID-19 patients.40–42 IS, ICH, and convexal subarachnoid hemorrhage are common manifestations of reversible cerebral vasoconstriction syndrome.43
Critical illness due to COVID-19
A significant percentage of patients with SARS-CoV-2 infection present with serious manifestations and may need intubation, mechanical ventilation, and prolonged hospitalization in intensive care units, mostly due to pulmonary complications. Hypoxemia and systemic hypotension due to primarily immune-mediated critical illness may further induce hypoxic/ischemic encephalopathy and contributes to IS, mostly in watershed territories or presenting as cortical laminar necrosis.44 Additionally, prolonged hypoxemia and respiratory failure have been associated with cerebral microbleeds and/or leukoencephalopathy.45
Cerebrovascular manifestations associated with COVID-19
Reports of cerebrovascular complications associated with COVID-19 are continuously increasing.
Ischemic stroke
A recently published, prospective, multinational study reported 123 patients who presented with acute IS out of a total of 17,799 SARS-CoV-2-infected patients.46 This result corresponds to a non-weighted risk of 0.7% for IS among patients hospitalized for COVID-19. Other cohort studies reporting IS risk among hospital admissions for COVID-19 also presented similar results (Table 1). These data underscore that COVID-19 may be associated with a small but non-negligible risk for IS. Another important fact is that IS is reported as the initial manifestation and reason for hospitalization in 26% of COVID-19-confirmed patients.47
| Table 1. Cohort studies reporting cerebrovascular events in COVID-19 patients during general hospital admission. |
Table 1. Cohort studies reporting cerebrovascular events in COVID-19 patients during general hospital admission. View larger version
View larger version
Regarding the IS subtype according to Trial of ORG 10172 in Acute Stroke Treatment classification, COVID-19 was reported to be associated with a higher incidence of cryptogenic stroke.47,48,56,60 According to a retrospective cohort study performed in a major health system in New York, cryptogenic stroke was twice more prevalent in COVID-19 positive patients compared with both a contemporary control group consisting of COVID-19 negative patients and a historical control group derived from patients treated in the same period in 2019.48 The presented high rates of cryptogenic stroke could further alarm clinicians regarding hypercoagulability state, in situ arterial thrombosis from endothelitis and occult cardioembolism or paradoxical embolism, both of which require deeper investigation and consideration of therapeutic anticoagulation.61–63 Other studies, which also included hospitalized COVID-19 patients, reported an incidence of up to 35% for cryptogenic stroke among IS patients.51,52,64 Finally, it should be noted that different case series of stroke complicating COVID-19 patients have reported a decreased prevalence of lacunar infarction (⩽10%) among IS patients.46,48 This observation indicates the potential lack of association between COVID-19 and intrinsic small-vessel disease. However, since lacunar strokes are generally associated with less severe symptoms compared with large-vessel occlusion (LVO) strokes, the patients may have not undergone neuroimaging evaluation with brain MRI and ascertainment of acute cerebral ischemia mechanism leading to the under-representation of lacunar strokes in patient cohorts.
Another important observation regarding IS incidence in patients with COVID-19 is the report of younger patients without known risk factors presenting with stroke due to LVO.65 Also, COVID-19 patients with LVO were younger compared with both contemporary controls of COVID-19-negative patients and historical controls, as investigated in different studies.66,67 In another case series, it was shown that among patients hospitalized for stroke due to LVO, more than half tested positive for SARS-CoV-2.67 Almost a quarter of COVID-19 patients admitted for acute IS is reported to be due to LVO.52,68 An illustrative case of a patient with LVO stroke and concurrent COVID-19 is presented in Figure 2. Multifocal LVOs is another matter of concern in those patients, since multivessel obstruction is presented significantly more frequently in SARS-CoV-2 positive patients.66,68
Figure 2. Imaging evaluation of a patient with acute proximal occlusion of the right middle cerebral artery during hospitalization for COVID-19.
A 65-year-old man with a history of hypertension and diabetes mellitus presented with acute left-sided hemiplegia, dysarthria, neglect, and right-gaze deviation. He had minimal respiratory symptoms. Emergency brain CT and CTA scanning were performed. Acute proximal right middle cerebral artery (MCA) occlusion was demonstrated on CTA (panel A, arrow) with evolving right MCA infarction. Right MCA occlusion was also confirmed on CTA 3D reconstruction (panel B, dotted circle). At that time, D-dimer levels were 2.8 ng/ml (normal values <500 ng/ml). The patient was not eligible for either intravenous thrombolysis due to delayed presentation or mechanical thrombectomy due to an unfavorable perfusion profile. Brain MRI was subsequently performed, showing restricted diffusion in right MCA territory, confirmative of large right MCA infarct (panel C). SARS-CoV-2 infection was confirmed at day 9 of hospitalization. On the 3-month follow up, the patient had modified Rankin Scale score of 4 with persistent severe left hemiparesis.
COVID-19, coronavirus disease 2019; CT, computed tomography; CTA, computed tomography angiography; MRI, magnetic resonance imaging; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In patients admitted with acute IS during the period of COVID-19 restrictions, significant concern has been raised regarding the delivery of acute reperfusion treatments. This gains even more importance, especially in the aforementioned patients with LVO, who may need mechanical thrombectomy. Initially, patients were thought to be reluctant to seek medical help for stroke symptoms due to their fear of contracting COVID-19, and subsequently presented with substantial delay to the emergency department, outside the time window for available acute reperfusion therapies.69,70 Different cohort studies evaluated the management in the acute phase of stroke patients during COVID-19 restrictions compared with historical controls treated in the same periods before the pandemic. Several of them have underscored the negative effect of lockdown on the management of IS, depicting reductions of stroke admissions, the total number of thrombolysis and/or thrombectomy and significant increases in treatment times.71–75
However, the American Heart Association/American Stroke Association Stroke Council Leadership responded promptly with emergency guidance to the need of addressing those issues and securing the delivery of acute stroke treatments.70 A ‘protected code stroke’ was recommended and a focused framework was provided with the aim of COVID-19-specific screening, personal protective equipment, and crisis resource management during acute stroke treatment.76 In addition, the European Society of Neurosonology and Cerebral Hemodynamics issued practice recommendations for neurovascular investigations of acute stroke patients during the COVID-19 pandemic aiming to highlight the utility of ultrasound as a non-invasive, easily repeatable bedside real-time examination of cerebral vessels.77 Finally, the European Stroke Organization and other organizations addressed to the public and underscored that patients with stroke symptoms should seek medical help as soon as possible, despite COVID-19 restrictions.78 Hopefully, such measures will contribute to the stabilization of stroke treatment delivery despite those unprecedented times.
Cerebral hemorrhage
Several case reports and cohort studies have recently been published presenting COVID-19 patients with parenchymal hemorrhage,58,59,79–85 subarachnoid hemorrhage,14,58,59,86 and subdural hematoma.59 A retrospective case series of five patients showed that COVID-19 patients with ICH were younger than expected and mostly suffered from lobar ICH.85 One of the patients described in this report had multifocal ICH without any underlying vascular abnormality.85 Similar results were presented in a retrospective cohort study, that showed 0.5% of hospitalized COVID-19 patients to be diagnosed with hemorrhagic stroke, with coagulopathy being the most common etiology.58 A large, deep intracerebral hematoma with an irregular, multi-lobular shape identified in a COVID-19 patient is presented in Figure 3.
Figure 3. Imaging evaluation of a COVID-19 patient with large, multi-lobular intracerebral hemorrhage.
A 55-year-old woman with a history of diabetes mellitus and hypertension was quarantined at home due to SARS-CoV-2 infection with mild respiratory symptoms. At 12 days later, she deteriorated, presenting dyspnea and respiratory failure. She was admitted to the ICU for mechanical ventilation. On day 11 of hospitalization, she became apneic on the ventilator, with fixed, dilated pupils. An emergent brain CT scan was performed showing a large, left-sided intracerebral hemorrhage causing compression of the ipsilateral lateral ventricle and midline shift to the right (panel A). The hematoma had an irregular, multi-lobular shape (panel A and B). No hypertensive spike was confirmed. The patient expired 1 day after neurological worsening.
COVID-19, coronavirus disease 2019; CT, computed tomography; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
However, among general hospital admissions of COVID-19 patients, only a minor proportion exhibited ICH (Table 1). Similarly, COVID-19 patients who were hospitalized in neurological wards did not have significantly more cerebral hemorrhagic events compared with non-COVID-19 patients.87 Based on these observations, it remains unknown whether COVID-19 has a causal association with ICH through ACE2 inactivation, endothelial dysfunction/degeneration, coagulopathy or hypocoagulability, or rather, whether secondary effects of COVID-19 such as renal failure/cirrhosis with concomitant therapeutic anticoagulation in a critically ill older population is the culprit. The atypical multifocal nature of many of the reported ICH cases to date would suggest some form of underlying vasculopathy which likely acts synergistically with the aforementioned factors in causing ICH. One pathological report to date has confirmed underlying endothelial reactivity, as well as endothelial and neuropil degeneration in a COVID-19 patient with ICH.34
Cerebral microbleeds have also been demonstrated in critically ill COVID-19 patients and can present with or without leukoencephalopathy.45,88 The atypical location of cerebral microbleeds in the corpus callosum and juxtacortical region may raise the suspicion of SARS-CoV-2 infection in critically ill patients.42 However, a very similar pattern has previously been presented in critically ill non-COVID-19 patients with respiratory failure.89,90 These neuroimaging findings are associated with worse neurological status and longer hospitalization in COVID-19, and likely reflect a more advanced stage of critical illness.45
Cerebral venous thrombosis
Venous thromboembolic events, such as pulmonary embolism and deep venous thrombosis, are detected with high frequency in COVID-19 patients hospitalized in intensive care units, even despite anticoagulation treatment.91 The risk of thrombosis associated with COVID-19 may also be responsible for CVT. Numerous case reports have been published about COVID-19 patients presenting with CVT.92–99 In addition, cases with more atypical presentations, such as cortical or deep cerebral venous thrombosis, have been described.100,101 Six patients were diagnosed with CVT among 17,799 hospitalized SARS-CoV-2 patients.46 Headache and impaired consciousness may complicate or even be the presenting symptoms of both COVID-19 and CVT (Figure 4). For that reason, clinicians should be quite vigilant in order to timely diagnose CVT-complicating COVID-19.102 Clinicians should also be able to differentiate COVID-19 patients with primary ICH and hemorrhagic infarction due to CVT, since the latter requires anticoagulant treatment in therapeutic dosage.103 Finally, CVT involving the internal cerebral veins may be challenging to differentiate from acute hemorrhagic necrotizing encephalitis (Weston–Hurst syndrome), which is another COVID-19 CNS complication that may symmetrically affect basal ganglia and thalami with hemorrhagic lesions.104
Figure 4. Imaging evaluation of a COVID-19 patient with cerebral venous thrombosis.
A 59-year-old woman presented with a thunderclap headache followed by a severe progressive headache. Her neurological examination revealed bilateral papilledema. In the brain CT scan, she had an ischemic occipital lesion (panel A). Brain MRV demonstrated lack of flow in the left transverse and sigmoid sinuses, confirming the diagnosis of cerebral venous sinus thrombosis (panel B). In addition, the patient reported she had a fever, cough, and sore throat 10 days before her neurological symptoms. Chest CT showed diffuse ground-glass opacification (panel C). A positive SARS-CoV2 PCR confirmed the diagnosis of COVID-19.
COVID-19, coronavirus disease 2019; CT, computed tomography; MRV, magnetic resonance venography; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Red flags for COVID-19-associated stroke diagnosis
Prompt diagnosis and treatment of acute cerebrovascular disease complicating COVID-19 are essential since co-existing stroke appears to negatively influence the outcome in patients with SARS-CoV-2 infection.50,105 Several clinical and neuroimaging characteristics are present and can raise suspicion in COVID-19 associated stroke diagnosis. The adjunctive use of artificial intelligence may expedite an accurate diagnosis and is already developing in the field of COVID-19-related brain injury.106
Ischemic strokes in COVID-19 patients often present with multi-territorial arterial distribution, embolic pattern, and hemorrhagic transformation.64,107–114 A COVID-19 patient diagnosed with multi-territorial arterial infarctions of an embolic pattern in the absence of vascular risk factors is shown in Figure 5. Large cerebral vessel occlusions with significant thrombus burden and a propensity for clot fragmentation is well documented in the literature.46,65,67,68,108,110,115 Characteristically, LVO may affect younger patients without known risk factors for stroke, it is associated with higher in-hospital mortality and may represent the initial manifestation leading to hospitalization during SARS-CoV-2 infection.65,67,115,116 Hypercoagulable state, cardioembolism, or paradoxical embolism due to COVID-19 may be potential reasons for such a stroke presentation. Furthermore, unexpected IS locations, such as in the corpus callosum or a frequent involvement of posterior circulation, have been associated with COVID-19.117–119 Increased incidence of hemorrhagic transformation of ischemic infarcts has also been observed in COVID-19 stroke patients.56,111 Whether the dysfunctional hemostasis or the increased use of anticoagulants could be associated with the likelihood of hemorrhagic transformation remains currently unknown. Finally, level of consciousness was recently reported as an important component in a risk stratification score related to severe COVID-19.120 Confusion may not only be an important parameter relating to the severity of a multisystem disease like COVID-19, but in addition, it may underlie the presence of cerebrovascular disease. Unsuccessful recovery after ventilation weaning should alarm clinicians about the possibility of cerebrovascular disease development, and mandates appropriate neuroimaging studies.111
Figure 5. Imaging evaluation of a COVID-19 patient with multi-territorial ischemic infarcts.
An 83-year-old man with a history of hypertension, diabetes, hyperlipidemia, and prior ischemic stroke with no residual symptoms, presented to the emergency department with seizure-like activity and acute respiratory failure, likely due to aspiration. Brain MRI was performed showing restricted diffusion in the territories of both the right middle cerebral artery (MCA; panel A) and the right posterior cerebral artery (PCA; panel B), indicating right MCA and PCA acute ischemic stroke. He was intubated in the emergency department for decreased level of consciousness, hypoxia, and airway protection and initially admitted to the medical ICU. On presentation and the day after presentation, nasopharyngeal swab tests were performed and were both negative for SARS-CoV-2. At 10 days after initial presentation, a third nasopharyngeal swab was performed and found positive, confirming SARS-CoV-2 infection. Despite initial hypoxia and multiorgan failure, the patient improved systematically and was eventually weaned off the ventilator after 1 month of ICU hospitalization. However, the neurological examination did not improve accordingly, and the patient did not fully regain his level of consciousness. For that reason, a brain MRI was repeated and disclosed acute left MCA (panel C and D) and additional right MCA (panel D) territory recurrent ischemic infarcts. The patient was finally discharged to a long-term nursing facility and expired approximately 2.5 months after his initial presentation.
COVID-19, coronavirus disease 2019; ICU, intensive care unit; MRI, magnetic resonance imaging; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
ICH may complicate in COVID-19 patients that are younger than expected for conventional ICH.85 Coagulopathy was reported as the most common etiology of ICH, whereas COVID-19-negative patients most often suffered from hypertension-related ICH.58 Coagulopathy is reflected by the significantly higher levels of D-dimers, which may be considered as a ‘red flag’ for COVID-19-associated ICH.58 Furthermore, although spontaneous ICH most typically presents as deep hemorrhage in patients with negative COVID-19 history, lobar and multi-focal hematomas without underlying macrovascular abnormalities are commonly reported in COVID-19 patients.58,85 Cerebral microbleeds represent a recently described neuroimaging finding in COVID-19 patients, which is associated with critical illness.45,88 In addition, anticoagulation treatment prior to the manifestation of hemorrhagic stroke in COVID-19 patients has been consistently reported in a recent case series from New York City.75
Development of CVT in patients without other risk factors of hypercoagulability should alert clinicians to the possibility of SARS-CoV-2 infection, especially in the presence of excessively high (>2.0 ng/ml) D-dimer levels. Persisting headache and altered consciousness with confusion and/or agitation, coupled with high levels of D-dimers, may be a hint for CVT complication that should be promptly diagnosed and anticoagulated.103
Prognosis of cerebrovascular events associated with COVID-19
Data regarding the long-term prognosis of COVID-19 patients with cerebrovascular events are scarce. Most studies report clinical outcomes at discharge. In a single-center study, it was shown that positive patients had higher National Institutes of Health Stroke Scale score and were less likely to achieve functional independency at discharge.87 Moreover, the mortality rate in COVID-19 stroke patients was higher compared with contemporary SARS-CoV-2-negative stroke patients.87 Similar results are confirmed in other cohort studies investigating cerebrovascular disease in COVID-19 patients compared with COVID-19-negative patients (Table 2). A high mortality rate was also reported in a multinational cohort study, for both ischemic and hemorrhagic COVID-19 stroke patients.56 Additionally, in the same study it was shown that 17.4% of COVID-19 IS patients suffered from a hemorrhagic transformation of the infarction.56
| Table 2. Cohort studies reporting clinical outcomes at discharge of COVID-19 patients with cerebrovascular disease compared with COVID-19-negative patients. |
Table 2. Cohort studies reporting clinical outcomes at discharge of COVID-19 patients with cerebrovascular disease compared with COVID-19-negative patients. View larger version
View larger version
Irrespective of SARS-CoV-2 positivity, the COVID-19 pandemic and the subsequently imposed restrictions had a negative influence on mortality and functional outcomes in stroke patients in general. Higher incidence of mortality and worse functional outcomes at discharge were reported in different cohort studies evaluating stroke patients who were admitted during the COVID-19 pandemic, compared with historical controls of the pre-COVID-19 period.60,64,71,72,122–125 These alarming results may be attributable to delays in the presentation of stroke patients and subsequent lower rates of recanalization therapies. Furthermore, longer hospitalization stay was needed for the acute management of stroke patients during COVID-19 pandemic.60,64,71,72,122 Severe neurological impairment of the stroke patients, limited medical and laboratory resources, assignment, and transfer of medical personnel from stroke wards to COVID-19 designated wards might explain the need for the extension of hospitalization.
Apart from the observation that SARS-CoV-2 is a risk factor of mortality in stroke patients, it has also been shown that COVID-19 patients who experienced an acute IS during the infection had significantly lower rates of survival compared with those without a stroke.50,105 In addition, a previous history of stroke was an independent risk factor for severe pneumonia leading to critical illness, the need for ventilation, and mortality in COVID-19 patients.126,127
In ICH patients, COVID-19 was negatively associated with prognosis. A higher mortality rate was observed in COVID-19 patients compared to both contemporary and historical negative controls with ICH.58 In another cohort, all COVID-19 patients with hemorrhagic lesions on brain MRI suffered from acute respiratory distress syndrome and were hospitalized in intensive care units.88 A total of 20% patients with hemorrhagic lesions died during hospitalization, compared with 6% of COVID-19 patients with other non-hemorrhagic lesions.88
Impact of COVID-19 pandemic on stroke management
The COVID-19 pandemic and the imposed restrictions severely impacted stroke management.9,69 Since the first weeks of the outbreak, declining numbers of stroke admissions have been reported in the literature.128,129 Patients with transient or minor stroke symptoms are more likely to avoid seeking medical help due to their fear of contracting the virus.130 Moreover, the availability of acute reperfusion therapies, including both intravenous thrombolysis and mechanical thrombectomy has been limited, according to recent reports from North America and Europe.71–75 When administered, treatment time metrics are prolonged, negatively impacting the effectiveness of the treatments.131 The performance of the more time-consuming, multiparametric stroke neuroimaging techniques is reported to have also declined, which, in turn, impedes the recognition of eligible patients for acute reperfusion therapies.132
In order to safely implement acute stroke management during the COVID-19-imposed restrictions, a ‘protected code stroke’ has been proposed.76 When a stroke patient presents to the emergency department, the clinicians should specifically ask for signs and symptoms compatible with COVID-19 infection, such as a history of fever, cough, dyspnea, diarrhea, hyposmia, or hypogeusia.133 History taking regarding COVID-19 should not be limited to the stroke patient, but should also include patients’ close contacts. Temperature checks can be used as an initial, feasible, and inexpensive screening tool upon patient presentation. In cases of positive COVID-19 history or confirmed fever, a nasopharyngeal swab should be tested for SARS-CoV-2 and repeated if negative and clinical suspicion is high, according to local COVID-19 protocols. Rapid antigen tests with high sensitivity and specificity can be used while in triage and may be a game changer in this regard. However, in cases of acute stroke, the management should not be delayed, and the patient should be treated as suspected COVID-19 by the minimum number of medical personnel and appropriate infection control measures, in order to minimize exposure.134
When indicated, intravenous thrombolysis with bolus tenecteplase might be considered as an alternative to alteplase bolus, and 1 h infusion to reduce the acute treatment duration and staff exposure.135 In addition, a minimum number of medical personnel, who should be experienced in donning and doffing personal protective equipment with safety, should perform mechanical thrombectomy procedures. If possible, mechanical thrombectomy under conscious sedation should be considered as the first line if the patient is stable.136 If general anesthesia and endotracheal intubation are needed, extreme caution is mandatory, since the latter is an aerosol and airborne-generating procedure. Ideally, intubation, mechanical ventilation, and extubation of the patient should be performed in negative-pressure rooms.136 Finally, acute stroke care should be provided by experienced stroke teams and the involved specialized personnel should not be redeployed to other hospital departments due to COVID-19-specific demands.137
During further hospitalization, transcranial ultrasound may be used to monitor intracranial vessel patency in IS patients who have received recanalization treatments, since it is a feasible, bedside test and can limit patient transportation.77 If further neuroimaging is needed, brain MRI may be performed for the differential diagnosis of COVID-19 patients with neurological manifestations.138 Moreover, regarding secondary prevention treatment in the subacute phase, prophylactic anticoagulant treatment is indicated in COVID-19 stroke patients.139,140 Finally, possible underlying mechanisms and deteriorating factors, such as hypoxia, coagulation disorder, and electrolyte imbalance should be managed, and cardiac function should be supported if needed during stroke hospitalization.
As for the long-term management and functional improvement, the COVID-19 stroke patients will not only require rehabilitation for their stroke, but also for the long-term consequences associated with a severe COVID-19 infection. The multidisciplinary stroke rehabilitation team needs to adapt to cater for both needs. It is of importance to initiate and maintain an inpatient rehabilitation program for the most severely affected patients.141 Tele-rehabilitation through electronic communication technologies may be a viable procedure for milder cases and their caregivers, limiting unnecessary transportation and close contacts, and providing protection against SARS-CoV-2 transmission.142,143 Finally, mental health should also be preserved. Stroke patients may often experience depression and anxiety, while anxiety itself may act as an additional trigger factor for acute stroke.144,145 Psychiatric support becomes even more important during the COVID-19 pandemic, since self-isolation, physical distancing, imposed restrictions and the fear of contracting the virus may pose additional emotional threats.146
Discussion
The causative versus incidental relationship between SARS-CoV-2 and stroke may still be debatable. Our narrative review presents the potential underlying mechanisms of the association between COVID-19 and cerebrovascular disease. ACE2 receptor dysregulation, excessive immune response, coagulation disorders, cardiac complications, and critical illness can lead to the development of different cerebrovascular disease manifestations during SARS-CoV-2 infection. However, stroke incidence in COVID-19 patients appears to be lower (0.5–1.5%) than what was originally reported from the Wuhan outbreak (5–6%).10,46–48 This discrepancy might partially be explained by the fact that during the first weeks of the pandemic, prophylactic anticoagulation treatment was not administered as a standard of care in every COVID-19 patient.
Several key aspects should be summarized based on the presented review. Cryptogenic ischemia due to LVO appears to be the most common manifestation of acute cerebral ischemia, while lacunar stroke is rarely reported to complicate SARS-CoV-2 infection. Coagulation disorders, in situ arterial thrombosis, paradoxical embolization through right-to-left shunts, and occult paroxysmal atrial fibrillation should be scrutinized as indicated. Lobar or subcortical ICH that may be temporally associated with the initiation of anticoagulation therapy appears to be the most prevalent hemorrhagic CNS manifestation of COVID-19. CVT may also present as a hemorrhagic transformation of the cerebral venous infarction and should be included in the differential diagnosis of hemorrhagic lesions in COVID-19 patients. Importantly, CVT may seldom (≈0.5%) represent the initial manifestation of COVID-19 in patients with underlying hypercoagulability.
The adverse outcomes of COVID-19 patients with co-existing cerebrovascular disease mandate physician alertness for timely diagnosis and swift delivery of available acute stroke therapies. Several clinical and neuroimaging characteristics may be utilized as red flags to promote diagnosis. Younger age of patients, the absence of known stroke risk factors, difficulties in weaning from mechanical ventilation, high D-dimer levels, spontaneously prolonged international normalized ratio (INR)/partial thromboplastin time (PTT), multi-territorial acute infarctions, unexpected stroke locations (e.g. splenium of the corpus callosum), and LVOs should alarm clinicians about the co-existence of stroke and SARS-CoV-2 infection. Despite COVID-19-imposed restrictions, acute treatment should be offered as indicated through a safe pathway for both the patients and the medical personnel. Tele-neurology and remote imaging access may minimize exposure of vascular neurologists during the management of SARS-CoV-2 infected patients and should be used when feasible.147,148
The limitations of the present review should be acknowledged. First, this is a narrative review of the literature with the aim of discussing the association between COVID-19 and stroke. Cohort studies and case series included in this review are highly heterogenous regarding stroke diagnostic work-up, acute management, study populations, and use of contemporary versus historical controls. Furthermore, we did not review studies that have been submitted but not accepted to international medical journals. Ideally, an up-to-date systematic review and meta-analysis of included cohort studies may be conducted, investigating the incidence, treatment, and outcomes of cerebrovascular disease in COVID-19 patients and providing future directions in stroke diagnosis and management in the COVID-19 era.
Conclusion
Neurological manifestations are not uncommon during SARS-CoV-2 infection. Among those, cerebrovascular disease was initially reported with an alarming incidence of 6% in a small Chinese cohort.10 However, recent studies in the international larger dataset report a smaller but non-negligible risk of stroke (0.5–1.5%) in infected patients.46–48 Whether this smaller risk could be attributed to the standard prophylactic anticoagulation given in every hospitalized patient is not known. ACE2 receptor dysregulation, inflammation, coagulopathy, COVID-19-associated cardiac involvement with subsequent cardio-embolism, and critical illness may all act as pathogenetic mechanisms for developing IS, hemorrhagic stroke, and CVT. Longer duration of hospitalization, worse functional outcomes at discharge, and higher in-hospital mortality are reported in COVID-19 associated stroke. For that reason, prompt stroke diagnosis and preservation of high-quality acute stroke treatment should be emphasized. Several clinical characteristics, such as younger age of patients and lack of known stroke risk factors, as well as neuroimaging (multi-territorial cerebral ischemia of embolic pattern due to underlying LVO) and laboratory (excessive elevation of D-dimer levels and spontaneously prolonged INR/PTT at hospital admission) caveats could further assist clinicians in diagnosing cerebrovascular disease in patients with SARS-CoV-2 infection.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement
The authors declare that there is no conflict of interest.
References
| 1. | World Health Organization . Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV), https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (2020, accessed 1 September 2020). Google Scholar |
| 2. | World Health Organization . Coronavirus disease (COVID-19) pandemic, https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (2020, accessed 25 September 2020). Google Scholar |
| 3. | Chen, N, Zhou, M, Dong, X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–513. Google Scholar | Crossref | Medline |
| 4. | Lai, CC, Ko, WC, Lee, PI, et al. Extra-respiratory manifestations of COVID-19. Int J Antimicrob Agents 2020; 56: 106024. Google Scholar | Crossref |
| 5. | Patel, KP, Patel, PA, Vunnam, RR, et al. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J Clin Virol 2020; 128: 104386. Google Scholar | Crossref | Medline |
| 6. | Kochi, AN, Tagliari, AP, Forleo, GB, et al. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol 2020; 31: 1003–1008. Google Scholar | Crossref | Medline |
| 7. | Gupta, A, Madhavan, MV, Sehgal, K, et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020; 26: 1017–1032. Google Scholar | Crossref | Medline |
| 8. | Gavriatopoulou, M, Korompoki, E, Fotiou, D, et al. Organ-specific manifestations of COVID-19 infection. Clin Exp Med 2020; 20: 493–506. Google Scholar | Crossref | Medline |
| 9. | Tsivgoulis, G, Palaiodimou, L, Katsanos, AH, et al. Neurological manifestations and implications of COVID-19 pandemic. Ther Adv Neurol Disord 2020; 13: 1756286420932036. Google Scholar | SAGE Journals |
| 10. | Mao, L, Jin, H, Wang, M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020; 77: 683–690. Google Scholar | Crossref | Medline |
| 11. | Kummer, BR, Klang, E, Stein, LK, et al. History of stroke is independently associated with in-hospital death in patients with COVID-19. Stroke 2020; 51: 3112–3114. Google Scholar | Crossref | Medline |
| 12. | Zhao, Y, Zhao, Z, Wang, Y, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv 2020.01.26.919985. DOI: 10.1101/2020.01.26.919985. Google Scholar | Crossref |
| 13. | Wang, H-Y, Li, X-L, Yan, Z-R, et al. Potential neurological symptoms of COVID-19. Ther Adv Neurol Disord 2020; 13: 1756286420917830. Google Scholar | SAGE Journals |
| 14. | Hernández-Durán, S, Salfelder, C, Schaeper, J, et al. Mechanical ventilation, sedation and neuromonitoring of patients with aneurysmal subarachnoid hemorrhage in Germany: results of a nationwide survey. Neurocrit Care. Epub ahead of print 24 June 2020. DOI: 10.1007/s12028-020-01029-8. Google Scholar | Crossref |
| 15. | Kaushik, P, Kaushik, M, Parveen, S, et al. Cross-talk between key players in patients with COVID-19 and ischemic stroke: a review on neurobiological insight of the pandemic. Mol Neurobiol 2020; 57: 4921–4928. Google Scholar | Crossref | Medline |
| 16. | Arroja, MMC, Reid, E, McCabe, C. Therapeutic potential of the renin angiotensin system in ischaemic stroke. Exp Transl Stroke Med 2016; 8: 8. Google Scholar | Crossref | Medline |
| 17. | Wang, H, Tang, X, Fan, H, et al. Potential mechanisms of hemorrhagic stroke in elderly COVID-19 patients. Aging (Albany NY) 2020; 12: 10022–10034. Google Scholar | Crossref | Medline |
| 18. | Peña Silva, RA, Chu, Y, Miller, JD, et al. Impact of ACE2 deficiency and oxidative stress on cerebrovascular function with aging. Stroke 2012; 43: 3358–3363. Google Scholar | Crossref | Medline |
| 19. | Aghagoli, G, Gallo Marin, B, Soliman, LB, et al. Cardiac involvement in COVID-19 patients: risk factors, predictors, and complications: a review. J Card Surg 2020; 35: 1302–1305. Google Scholar | Crossref | Medline |
| 20. | Bhatla, A, Mayer, MM, Adusumalli, S, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm 2020; 17: 1439–1444. Google Scholar | Crossref | Medline |
| 21. | Becker, RC. COVID-19 update: Covid-19-associated coagulopathy. J Thromb Thrombolysis 2020; 50: 54–67. Google Scholar | Crossref | Medline |
| 22. | Zhang, Y, Xiao, M, Zhang, S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020; 382: e38. Google Scholar | Crossref |
| 23. | Klok, FA, Kruip, M, Van der Meer, NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020; 191: 145–147. Google Scholar | Crossref | Medline |
| 24. | Helms, J, Tacquard, C, Severac, F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020; 46: 1089–1098. Google Scholar | Crossref | Medline |
| 25. | Kananeh, MF, Thomas, T, Sharma, K, et al. Arterial and venous strokes in the setting of COVID-19. J Clin Neurosci 2020; 79: 60–66. Google Scholar | Crossref | Medline |
| 26. | Beyrouti, R, Adams, ME, Benjamin, L, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry 2020; 91: 889–891. Google Scholar | Crossref | Medline |
| 27. | Ren, B, Yan, F, Deng, Z, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation 2020; 142: 181–183. Google Scholar | Crossref | Medline |
| 28. | Zhang, L, Feng, X, Zhang, D, et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China. Circulation 2020; 142: 114–128. Google Scholar | Crossref | Medline |
| 29. | Reynolds, AS, Lee, AG, Renz, J, et al. Pulmonary vascular dilatation detected by automated transcranial doppler in COVID-19 pneumonia. Am J Respir Crit Care Med 2020; 202: 1037–1039. Google Scholar | Crossref | Medline |
| 30. | Iba, T, Levy, JH, Connors, JM, et al. The unique characteristics of COVID-19 coagulopathy. Crit Care 2020; 24: 360. Google Scholar | Crossref | Medline |
| 31. | Levi, M. COVID–19 coagulopathy vs disseminated intravascular coagulation. Blood Adv 2020; 4: 2850. Google Scholar | Crossref | Medline |
| 32. | Taylor, FB, Toh, CH, Hoots, WK, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 2001; 86: 1327–1330. Google Scholar | Crossref | Medline | ISI |
| 33. | Paniz-Mondolfi, A, Bryce, C, Grimes, Z, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol 2020; 92: 699–702. Google Scholar | Crossref | Medline |
| 34. | Hernández-Fernández, F, Valencia, HS, Barbella-Aponte, RA, et al. Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain 2020; 143: 3089–3103. Google Scholar | Crossref | Medline |
| 35. | Vaschetto, R, Cena, T, Sainaghi, PP, et al. Cerebral nervous system vasculitis in a Covid-19 patient with pneumonia. J Clin Neurosci 2020; 79: 71–73. Google Scholar | Crossref | Medline |
| 36. | Dixon, L, Coughlan, C, Karunaratne, K, et al. Immunosuppression for intracranial vasculitis associated with SARS-CoV-2: therapeutic implications for COVID-19 cerebrovascular pathology. J Neurol Neurosurg Psychiatry. Epub ahead of print 27 August 2020. DOI: 10.1136/jnnp-2020-324291. Google Scholar | Crossref |
| 37. | Hanafi, R, Roger, PA, Perin, B, et al. COVID-19 neurologic complication with CNS vasculitis-like pattern. AJNR Am J Neuroradiol 2020; 41: 1384–1387. Google Scholar | Crossref | Medline |
| 38. | Ellul, MA, Benjamin, L, Singh, B, et al. Neurological associations of COVID-19. Lancet Neurol 2020; 19: 767–783. Google Scholar | Crossref | Medline |
| 39. | John, S, Hajj-Ali, RA. CNS vasculitis. Semin Neurol 2014; 34: 405–412. Google Scholar | Crossref | Medline |
| 40. | Dakay, K, Kaur, G, Gulko, E, et al. Reversible cerebral vasoconstriction syndrome and dissection in the setting of COVID-19 infection. J Stroke Cerebrovasc Dis 2020; 29: 105011. Google Scholar | Crossref |
| 41. | Princiotta Cariddi, L, Tabaee Damavandi, P, Carimati, F, et al. Reversible encephalopathy syndrome (PRES) in a COVID-19 patient. J Neurol 2020; 267: 3157–3160. Google Scholar | Crossref | Medline |
| 42. | Franceschi, AM, Ahmed, O, Giliberto, L, et al. Hemorrhagic posterior reversible encephalopathy syndrome as a manifestation of COVID-19 infection. AJNR Am J Neuroradiol 2020; 41: 1173–1176. Google Scholar | Crossref | Medline |
| 43. | Nawabi, J, Morotti, A, Wildgruber, M, et al. Clinical and imaging characteristics in patients with SARS-CoV-2 infection and acute intracranial hemorrhage. J Clin Med 2020; 9: 2543. Google Scholar | Crossref |
| 44. | Fan, S, Xiao, M, Han, F, et al. Neurological manifestations in critically ill patients with COVID-19: a retrospective study. Front Neurol 2020; 11: 806. Google Scholar | Crossref | Medline |
| 45. | Agarwal, S, Jain, R, Dogra, S, et al. Cerebral microbleeds and leukoencephalopathy in critically ill patients with COVID-19. Stroke 2020; 51: 2649–2655. Google Scholar | Crossref | Medline |
| 46. | Shahjouei, S, Naderi, S, Li, J, et al. Risk of stroke in hospitalized SARS-CoV-2 infected patients: a multinational study. EBioMedicine 2020; 59: 102939. Google Scholar | Crossref | Medline |
| 47. | Merkler, AE, Parikh, NS, Mir, S, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol 2020; 77: 1–7. Google Scholar | Crossref |
| 48. | Yaghi, S, Ishida, K, Torres, J, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke 2020; 51: 2002–2011. Google Scholar | Crossref | Medline |
| 49. | Lodigiani, C, Iapichino, G, Carenzo, L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020; 191: 9–14. Google Scholar | Crossref | Medline |
| 50. | Jain, R, Young, M, Dogra, S, et al. COVID-19-related neuroimaging findings: a signal of thromboembolic complications and a strong prognostic marker of poor patient outcome. J Neurol Sci 2020; 414: 116923. Google Scholar | Crossref | Medline |
| 51. | Cantador, E, Núñez, A, Sobrino, P, et al. Incidence and consequences of systemic arterial thrombotic events in COVID-19 patients. J Thromb Thrombolysis 2020; 50: 543–547. Google Scholar | Crossref | Medline |
| 52. | Rothstein, A, Oldridge, O, Schwennesen, H, et al. Acute cerebrovascular events in hospitalized COVID-19 patients. Stroke 2020; 51: e219–e222. Google Scholar | Crossref | Medline |
| 53. | Li, Y, Wang, M, Zhou, Y, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3550025 (2020, accessed 4 April 2020). Google Scholar |
| 54. | Romero-Sánchez, CM, Díaz-Maroto, I, Fernández-Díaz, E, et al. Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology 2020; 95: e1060–e1070. Google Scholar | Crossref | Medline |
| 55. | Katz, JM, Libman, RB, Wang, JJ, et al. Cerebrovascular complications of COVID-19. Stroke 2020; 51: e227–e231. Google Scholar | Crossref | Medline |
| 56. | Siegler, JE, Cardona, P, Arenillas, JF, et al. EXPRESS: cerebrovascular events and outcomes in hospitalized patients with COVID-19: the SVIN COVID-19 multinational registry. Int J Stroke. Epub ahead of print 30 September 2020. DOI: 10.1177/1747493020959216. Google Scholar | Crossref |
| 57. | Requena, M, Olivé-Gadea, M, Muchada, M, et al. COVID-19 and stroke: incidence and etiological description in a high-volume center. J Stroke Cerebrovasc Dis 2020; 29: 105225. Google Scholar | Crossref | Medline |
| 58. | Kvernland, A, Kumar, A, Yaghi, S, et al. Anticoagulation use and hemorrhagic stroke in SARS-CoV-2 patients treated at a New York healthcare system. Neurocrit Care. Epub ahead of print 24 August 2020. DOI: 10.1007/s12028-020-01077-0. Google Scholar | Crossref |
| 59. | Altschul, DJ, Unda, SR, de La Garza Ramos, R, et al. Hemorrhagic presentations of COVID-19: risk factors for mortality. Clin Neurol Neurosurg 2020; 198: 106112. Google Scholar | Crossref | Medline |
| 60. | Naccarato, M, Scali, I, Olivo, S, et al. Has COVID-19 played an unexpected “stroke” on the chain of survival? J Neurol Sci 2020; 414: 116889. Google Scholar | Crossref | Medline |
| 61. | Tsivgoulis, G, Katsanos, AH, Ornello, R, et al. Ischemic stroke epidemiology during the COVID-19 pandemic. Stroke 2020; 51: 1924–1926. Google Scholar | Crossref | Medline |
| 62. | Fara, MG, Stein, LK, Skliut, M, et al. Macrothrombosis and stroke in patients with mild Covid-19 infection. J Thromb Haemost 2020; 18: 2031–2033. Google Scholar | Crossref | Medline |
| 63. | Esenwa, C, Cheng, NT, Lipsitz, E, et al. COVID-19-associated carotid atherothrombosis and stroke. AJNR Am J Neuroradiol 2020; 41: 1993–1995. Google Scholar | Crossref | Medline |
| 64. | Siegler, JE, Heslin, ME, Thau, L, et al. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020; 29: 104953. Google Scholar | Crossref |
| 65. | Oxley, TJ, Mocco, J, Majidi, S, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med 2020; 382: e60. Google Scholar | Crossref | Medline |
| 66. | Escalard, S, Chalumeau, V, Escalard, C, et al. Early brain imaging shows increased severity of acute ischemic strokes with large vessel occlusion in COVID-19 patients. Stroke 2020; 51: 3366–3370. Google Scholar | Crossref | Medline |
| 67. | Majidi, S, Fifi, JT, Ladner, TR, et al. Emergent large vessel occlusion stroke during New York City’s COVID-19 outbreak: clinical characteristics and paraclinical findings. Stroke 2020; 51: 2656–2663. Google Scholar | Crossref | Medline |
| 68. | Kihira, S, Schefflein, J, Mahmoudi, K, et al. Association of coronavirus disease (COVID-19) with large vessel occlusion strokes: a case-control study. AJR Am J Roentgenol. Epub ahead of print 29 July 2020. DOI: 10.2214/ajr.20.23847. Google Scholar | Crossref |
| 69. | Zhao, J, Rudd, A, Liu, R. Challenges and potential solutions of stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke 2020; 51: 1356–1357. Google Scholar | Crossref | Medline |
| 70. | AHA/ASA Stroke Council Leadership . Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic. Stroke 2020; 51: 1910–1912. Google Scholar | Crossref | Medline |
| 71. | Rudilosso, S, Laredo, C, Vera, V, et al. Acute stroke care is at risk in the era of COVID-19. Stroke 2020; 51: 1991–1995. Google Scholar | Crossref | Medline |
| 72. | Frisullo, G, Brunetti, V, Di Iorio, R, et al. Effect of lockdown on the management of ischemic stroke: an Italian experience from a COVID hospital. Neurol Sci 2020; 41: 2309–2313. Google Scholar | Crossref | Medline |
| 73. | Pop, R, Quenardelle, V, Hasiu, A, et al. Impact of the COVID-19 outbreak on acute stroke pathways – insights from the Alsace region in France. Eur J Neurol 2020; 27: 1783–1787. Google Scholar | Crossref | Medline |
| 74. | Kerleroux, B, Fabacher, T, Bricout, N, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak. Stroke 2020; 51: 2012–2017. Google Scholar | Crossref | Medline |
| 75. | Zhao, J, Li, H, Kung, D, et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020; 51: 1996–2001. Google Scholar | Crossref | Medline |
| 76. | Khosravani, H, Rajendram, P, Notario, L, et al. Protected code stroke. Stroke 2020; 51: 1891–1895. Google Scholar | Crossref | Medline |
| 77. | Baracchini, C, Pieroni, A, Kneihsl, M, et al. Practice recommendations for neurovascular ultrasound investigations of acute stroke patients in the setting of the COVID-19 pandemic: an expert consensus from the European Society of Neurosonology and Cerebral Hemodynamics. Eur J Neurol. Epub ahead of print 19 May 2020. DOI: 10.1111/ene.14334. Google Scholar | Crossref |
| 78. | Aguiar, de, Sousa, D, Van der Worp, HB, Caso, V, et al. Maintaining stroke care in Europe during the COVID-19 pandemic: results from an international survey of stroke professionals and practice recommendations from the European Stroke Organisation. Eur Stroke J 2020; 5: 230–236. Google Scholar | SAGE Journals |
| 79. | Giorgianni, A, Vinacci, G, Agosti, E, et al. Neuroradiological features in COVID-19 patients: first evidence in a complex scenario. J Neuroradiol 2020; 47: 474–476. Google Scholar | Crossref | Medline |
| 80. | Sharifi-Razavi, A, Karimi, N, Rouhani, N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect 2020; 35: 100669. Google Scholar | Crossref | Medline |
| 81. | Bao, Y, Lin, SY, Cheng, ZH, et al. Clinical features of COVID-19 in a young man with massive cerebral hemorrhage-case report. SN Compr Clin Med. Epub ahead of print 23 May 2020. DOI: 10.1007/s42399-020-00315-y. Google Scholar | Crossref |
| 82. | Khattar, NK, Sharma, M, McCallum, AP, et al. Intracranial hemorrhage in a young COVID-19 patient. Interdiscip Neurosurg 2020; 22: 100878. Google Scholar | Crossref | Medline |
| 83. | Daci, R, Kennelly, M, Ferris, A, et al. Bilateral basal ganglia hemorrhage in a patient with confirmed COVID-19. AJNR Am J Neuroradiol 2020; 41: 1797–1799. Google Scholar | Crossref | Medline |
| 84. | Agarwal, A, Vishnu, VY, Vibha, D, et al. Intracerebral hemorrhage and SARS-CoV-2: association or causation. Ann Indian Acad Neurol 2020; 23: 261–264. Google Scholar | Medline |
| 85. | Benger, M, Williams, O, Siddiqui, J, et al. Intracerebral haemorrhage and COVID-19: clinical characteristics from a case series. Brain Behav Immun 2020; 88: 940–944. Google Scholar | Crossref | Medline |
| 86. | Craen, A, Logan, G, Ganti, L. Novel coronavirus disease 2019 and subarachnoid hemorrhage: a case report. Cureus 2020; 12: e7846. Google Scholar | Medline |
| 87. | Benussi, A, Pilotto, A, Premi, E, et al. Clinical characteristics and outcomes of inpatients with neurologic disease and COVID-19 in Brescia, Lombardy, Italy. Neurology 2020; 95: e910–e920. Google Scholar | Crossref | Medline |
| 88. | Kremer, S, Lersy, F, de Sèze, J, et al. Brain MRI findings in severe COVID-19: a retrospective observational study. Radiology 2020; 297: E242–E251. Google Scholar | Crossref | Medline |
| 89. | Breit, H, Jhaveri, M, John, S. Concomitant delayed posthypoxic leukoencephalopathy and critical illness microbleeds. Neurol Clin Pract 2018; 8: e31–e33. Google Scholar | Crossref | Medline |
| 90. | Fanou, EM, Coutinho, JM, Shannon, P, et al. Critical illness-associated cerebral microbleeds. Stroke 2017; 48: 1085–1087. Google Scholar | Crossref | Medline |
| 91. | Llitjos, J-F, Leclerc, M, Chochois, C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost 2020; 18: 1743–1746. Google Scholar | Crossref | Medline |
| 92. | Cavalcanti, DD, Raz, E, Shapiro, M, et al. Cerebral venous thrombosis associated with COVID-19. AJNR Am J Neuroradiol 2020; 41: 1370–1376. Google Scholar | Crossref | Medline |
| 93. | Klein, DE, Libman, R, Kirsch, C, et al. Cerebral venous thrombosis: a typical presentation of COVID-19 in the young. J Stroke Cerebrovasc Dis 2020; 29: 104989. Google Scholar | Crossref |
| 94. | Garaci, F, Di Giuliano, F, Picchi, E, et al. Venous cerebral thrombosis in COVID-19 patient. J Neurol Sci 2020; 414: 116871. Google Scholar | Crossref | Medline |
| 95. | Hemasian, H, Ansari, B. First case of Covid-19 presented with cerebral venous thrombosis: a rare and dreaded case. Rev Neurol (Paris) 2020; 176: 521–523. Google Scholar | Crossref | Medline |
| 96. | Hughes, C, Nichols, T, Pike, M, et al. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur J Case Rep Intern Med 2020; 7: 001691. Google Scholar | Medline |
| 97. | Bolaji, P, Kukoyi, B, Ahmad, N, et al. Extensive cerebral venous sinus thrombosis: a potential complication in a patient with COVID-19 disease. BMJ Case Rep 2020; 13: e236820. Google Scholar | Crossref | Medline |
| 98. | Poillon, G, Obadia, M, Perrin, M, et al. Cerebral venous thrombosis associated with COVID-19 infection: causality or coincidence? J Neuroradiol. Epub ahead of print 11 May 2020. DOI: 10.1016/j.neurad.2020.05.003. Google Scholar | Crossref |
| 99. | Roy-Gash, F, De Mesmay, M, Devys, J-M, et al. COVID-19-associated acute cerebral venous thrombosis: clinical, CT, MRI and EEG features. Crit Care 2020; 24: 419. Google Scholar | Crossref | Medline |
| 100. | Baudar, C, Duprez, T, Kassab, A, et al. COVID-19 as triggering co-factor for cortical cerebral venous thrombosis? J Neuroradiol. Epub ahead of print 27 June 2020. DOI: 10.1016/j.neurad.2020.06.008. Google Scholar | Crossref |
| 101. | Chougar, L, Mathon, B, Weiss, N, et al. Atypical deep cerebral vein thrombosis with hemorrhagic venous infarction in a patient positive for COVID-19. AJNR Am J Neuroradiol 2020; 41: 1377–1379. Google Scholar | Crossref | Medline |
| 102. | Shakibajahromi, B, Borhani-Haghighi, A, Haseli, S, et al. Cerebral venous sinus thrombosis might be under-diagnosed in the COVID-19 era. eNeurologicalSci 2020; 20: 100256. Google Scholar | Crossref | Medline |
| 103. | Argirò, R, Cirelli, C, Sgreccia, A, et al. Cerebral hemorrhage related to vein thrombosis in Covid-19 patients in different Italian hospitals: view point for clinical and imaging implications. J Neurol Sci 2020; 416: 117023. Google Scholar | Crossref | Medline |
| 104. | Poyiadji, N, Shahin, G, Noujaim, D, et al. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology 2020; 296: E119–E120. Google Scholar | Crossref | Medline |
| 105. | Annie, F, Bates, MC, Nanjundappa, A, et al. Prevalence and outcomes of acute ischemic stroke among patients ⩽50 years of age with laboratory confirmed COVID-19 infection. Am J Cardiol 2020; 130: 169–170. Google Scholar | Crossref | Medline |
| 106. | Suri, JS, Puvvula, A, Biswas, M, et al. COVID-19 pathways for brain and heart injury in comorbidity patients: a role of medical imaging and artificial intelligence-based COVID severity classification: a review. Comput Biol Med 2020; 124: 103960. Google Scholar | Crossref | Medline |
| 107. | Escalard, S, Maïer, B, Redjem, H, et al. Treatment of acute ischemic stroke due to large vessel occlusion with COVID-19: experience from Paris. Stroke 2020; 51: 2540–2543. Google Scholar | Crossref | Medline |
| 108. | John, S, Kesav, P, Mifsud, VA, et al. Characteristics of large-vessel occlusion associated with COVID-19 and ischemic stroke. AJNR Am J Neuroradiol. Epub ahead of print 27 August 2020. DOI: 10.3174/ajnr.A6799. Google Scholar | Crossref |
| 109. | Zayet, S, Klopfenstein, T, Kovẚcs, R, et al. Acute cerebral stroke with multiple infarctions and COVID-19, France, 2020. Emerg Infect Dis 2020; 26: 2258–2260. Google Scholar | Crossref |
| 110. | Wang, A, Mandigo, GK, Yim, PD, et al. Stroke and mechanical thrombectomy in patients with COVID-19: technical observations and patient characteristics. J Neurointerv Surg 2020; 12: 648–653. Google Scholar | Crossref | Medline |
| 111. | Díaz-Pérez, C, Ramos, C, López-Cruz, A, et al. Acutely altered mental status as the main clinical presentation of multiple strokes in critically ill patients with COVID-19. Neurol Sci 2020; 41: 2681–2684. Google Scholar | Crossref | Medline |
| 112. | Guillan, M, Villacieros-Alvarez, J, Bellido, S, et al. Unusual simultaneous cerebral infarcts in multiple arterial territories in a COVID-19 patient. Thromb Res 2020; 193: 107–109. Google Scholar | Crossref | Medline |
| 113. | Elshereye, A, Erdinc, B. Multiple lacunar cerebral infarcts as the initial presentation of COVID-19. Cureus 2020; 12: e9638. Google Scholar |
| 114. | Cerasti, D, Ormitti, F, Pardatscher, S, et al. Multiple acute ischemic strokes in a COVID-19 patient: a case report. SN Compr Clin Med. Epub ahead of print 4 July 2020. DOI: 10.1007/s42399-020-00388-9. Google Scholar | Crossref |
| 115. | Alkhaibary, A, Abbas, M, Ahmed, ME, et al. Common carotid artery occlusion in a young patient: can large-vessel stroke be the initial clinical manifestation of COVID-19? World Neurosurg 2020; 144: 140–142. Google Scholar | Crossref | Medline |
| 116. | Altschul, DJ, Esenwa, C, Haranhalli, N, et al. Predictors of mortality for patients with COVID-19 and large vessel occlusion. Interv Neuroradiol 2020; 26: 623–628. Google Scholar | SAGE Journals |
| 117. | Sparr, SA, Bieri, PL. Infarction of the splenium of the corpus callosum in the age of COVID-19: a snapshot in time. Stroke 2020; 51: e223–e226. Google Scholar |
| 118. | Bonardel, C, Bonnerot, M, Ludwig, M, et al. Bilateral posterior cerebral artery territory infarction in a SARS-Cov-2 infected patient: discussion about an unusual case. J Stroke Cerebrovasc Dis 2020; 29: 105095. Google Scholar | Crossref | Medline |
| 119. | D’Amore, F, Vinacci, G, Agosti, E, et al. Pressing issues in COVID-19: probable cause to seize SARS-CoV-2 for its preferential involvement of posterior circulation manifesting as severe posterior reversible encephalopathy syndrome and posterior strokes. AJNR Am J Neuroradiol 2020; 41: 1800–1803. Google Scholar | Crossref | Medline |
| 120. | Knight, SR, Ho, A, Pius, R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: development and validation of the 4C mortality score. BMJ 2020; 370: m3339. Google Scholar |
| 121. | Ntaios, G, Michel, P, Georgiopoulos, G, et al. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke. Stroke 2020; 51: e254–e258. Google Scholar | Crossref |
| 122. | Tulius Silva, M, Quintanilha, G, Giesel, L, et al. The impact of the COVID-19 pandemic on a stroke center in Latin America. Int J Stroke 2020; 15: 813–814. Google Scholar | SAGE Journals | ISI |
| 123. | Rinkel, LA, Prick, JCM, Slot, RER, et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol. Epub ahead of print 20 July 2020. DOI: 10.1007/s00415-020-10069-1. Google Scholar | Crossref |
| 124. | Roushdy, TM, Nahas, NME, Aref, HM, et al. Stroke in the time of coronavirus disease 2019: experience of two university stroke centers in Egypt. J Stroke 2020; 22: 275–277. Google Scholar | Crossref | Medline |
| 125. | Sarfo, FS, Mensah, NO, Opoku, FA, et al. COVID-19 and stroke: experience in a Ghanaian healthcare system. J Neurol Sci 2020; 416: 117044. Google Scholar | Crossref | Medline |
| 126. | Zhang, L, Sun, W, Wang, Y, et al. Clinical course and mortality of stroke patients with coronavirus disease 2019 in Wuhan, China. Stroke 2020; 51: 2674–2682. Google Scholar | Crossref | Medline |
| 127. | Siepmann, T, Sedghi, A, Barlinn, J, et al. Association of history of cerebrovascular disease with severity of COVID-19. J Neurol. Epub ahead of print 6 August 2020. DOI: 10.1007/s00415-020-10121-0. Google Scholar | Crossref |
| 128. | Montaner, J, Barragán-Prieto, A, Pérez-Sánchez, S, et al. Break in the stroke chain of survival due to COVID-19. Stroke 2020; 51: 2307–2314. Google Scholar | Crossref | Medline |
| 129. | Jasne, AS, Chojecka, P, Maran, I, et al. Stroke code presentations, interventions, and outcomes before and during the COVID-19 pandemic. Stroke 2020; 51: 2664–2673. Google Scholar | Crossref | Medline |
| 130. | Diegoli, H, Magalhães, PSC, Martins, SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 2020; 51: 2315–2321. Google Scholar | Crossref | Medline |
| 131. | Katsanos, AH, De Sa Boasquevisque, D, Al-Qami, MA, et al. In-hospital delays for acute stroke treatment delivery during the COVID-19 pandemic. Can J Neurol Sci. Epub ahead of print 3 August 2020. DOI: 10.1017/cjn.2020.170. Google Scholar | Crossref |
| 132. | Kansagra, AP, Goyal, MS, Hamilton, S, et al. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med 2020; 383: 400–401. Google Scholar | Crossref | Medline |
| 133. | Smith, MS, Bonomo, J, Knight, WA, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke 2020; 51: 1902–1909. Google Scholar | Crossref | Medline |
| 134. | Jin, H, Hong, C, Chen, S, et al. Consensus for prevention and management of coronavirus disease 2019 (COVID-19) for neurologists. Stroke Vasc Neurol 2020; 5: 146–151. Google Scholar | Crossref | Medline |
| 135. | Warach, SJ, Saver, JL. Stroke thrombolysis with tenecteplase to reduce emergency department spread of coronavirus disease 2019 and shortages of alteplase. JAMA Neurol. Epub ahead of print 20 July 2020. DOI: 10.1001/jamaneurol.2020.2396. Google Scholar | Crossref |
| 136. | Nguyen, TN, Abdalkader, M, Jovin, TG, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams. Stroke 2020; 51: 1896–1901. Google Scholar | Crossref | Medline |
| 137. | Wira, CR, Goyal, M, Southerland, AM, et al. Pandemic guidance for stroke centers aiding COVID-19 treatment teams. Stroke 2020; 51: 2587–2592. Google Scholar | Crossref | Medline |
| 138. | Kremer, S, Lersy, F, Anheim, M, et al. Neurologic and neuroimaging findings in COVID-19 patients: a retrospective multicenter study. Neurology 2020; 95: e1868–e1882. Google Scholar | Crossref | Medline |
| 139. | Mishra, AK, Sahu, KK, Lal, A, et al. Mechanisms of stroke and the role of anticoagulants in COVID-19. J Formos Med Assoc 2020; 119: 1721–1722. Google Scholar | Crossref | Medline |
| 140. | Aghamohammadi, M, Alizargar, J, Hsieh, N-C, et al. Prophylactic anticoagulant therapy for reducing the risk of stroke and other thrombotic events in COVID-19 patients. J Formos Med Assoc 2020; 119: 1230–1231. Google Scholar | Crossref | Medline |
| 141. | Leocani, L, Diserens, K, Moccia, M, et al. Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur J Neurol. Epub ahead of print 13 May 2020. DOI: 10.1111/ene.14320. Google Scholar | Crossref |
| 142. | Chang, MC, Boudier-Revéret, M. Usefulness of telerehabilitation for stroke patients during the COVID-19 pandemic. Am J Phys Med Rehabil 2020; 99: 582. Google Scholar | Crossref | Medline |
| 143. | Wang, C-C, Chao, J-K, Wang, M-L, et al. Care for patients with stroke during the COVID-19 pandemic: physical therapy and rehabilitation suggestions for preventing secondary stroke. J Stroke Cerebrovasc Dis 2020; 29: 105182. Google Scholar | Crossref |
| 144. | Robinson, RG, Spalletta, G. Poststroke depression: a review. Can J Psychiatry 2010; 55: 341–349. Google Scholar | SAGE Journals | ISI |
| 145. | Sharma, A, Prasad, K, Padma, MV, et al. Prevalence of triggering factors in acute stroke: hospital-based observational cross-sectional study. J Stroke Cerebrovasc Dis 2015; 24: 337–347. Google Scholar | Crossref | Medline |
| 146. | Galea, S, Merchant, RM, Lurie, N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med 2020; 180: 817–818. Google Scholar | Crossref | Medline |
| 147. | Klein, BC, Busis, NA. COVID-19 is catalyzing the adoption of teleneurology. Neurology 2020; 94: 903–904. Google Scholar | Crossref | Medline |
| 148. | Roy, B, Nowak, RJ, Roda, R, et al. Teleneurology during the COVID-19 pandemic: a step forward in modernizing medical care. J Neurol Sci 2020; 414: 116930. Google Scholar | Crossref |