Authors: Shotaro Tabata 1, Hiroki Hosoi 2, Shogo Murata 1, Satomi Takeda 1, Toshiki Mushino 1, Takashi Sonoki 1PMID: 34920343
PMCID: PMC8668346I: 10.1016/j.jaut.2021.102782 J Autoimmun. 2022 Jan; 126: 102782.Published online 2021 Dec 14. doi: 10.1016/j.jaut.2021.102782
Abstract
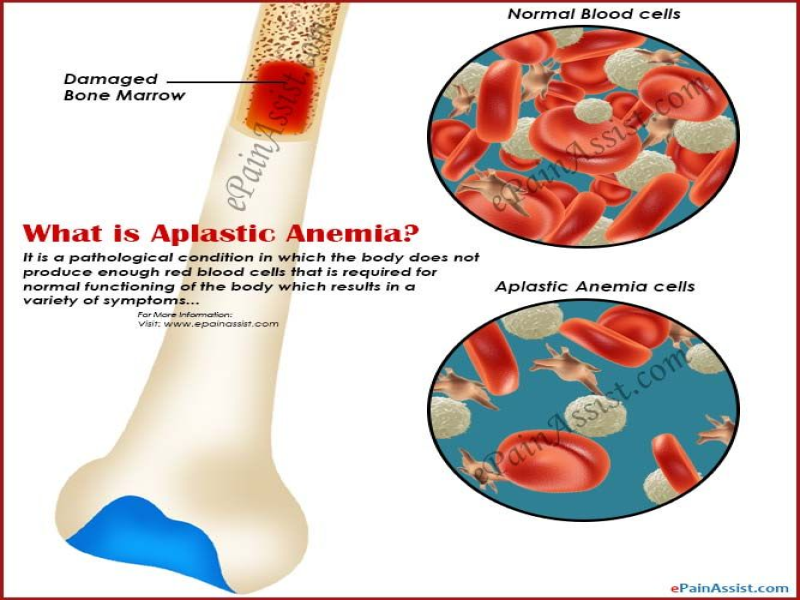
The development of various autoimmune diseases has been reported after COVID-19 infections or vaccinations. However, no method for assessing the relationships between vaccines and the development of autoimmune diseases has been established. Aplastic anemia (AA) is an immune-mediated bone marrow failure syndrome. We report a case of severe AA that arose after the administration of a COVID-19 vaccine (the Pfizer-BioNTech mRNA vaccine), which was treated with allogeneic hematopoietic stem cell transplantation (HSCT). In this patient, antibodies against the SARS-CoV-2 spike protein were detected both before and after the HSCT. After the patient’s hematopoietic stem cells were replaced through HSCT, his AA improved despite the presence of anti-SARS-CoV-2 antibodies. In this case, antibodies derived from the COVID-19 vaccine may not have been directly involved in the development of AA. This case suggests that the measurement of vaccine antibody titers before and after allogeneic HSCT may provide clues to the pathogenesis of vaccine-related autoimmune diseases. Although causality was not proven in this case, further evaluations are warranted to assess the associations between vaccines and AA.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a global pandemic of coronavirus disease 2019 (COVID-19). The introduction of SARS-CoV-2 vaccines has drastically reduced the transmission rate of the disease. Studies have confirmed the safety and efficacy of the available SARS-CoV-2 vaccines. However, rare cases of adverse immunological reactions to SARS-CoV-2 vaccines have been reported, including cases involving immune-mediated disease [[1], [2], [3]]. Although evaluating the associations between SARS-CoV-2 vaccines and the development of autoimmune diseases is important, no method for assessing such relationships has been established. Aplastic anemia (AA), a bone marrow failure syndrome, appears to be immune-mediated [4,5]. In addition to T lymphocytes and cytokines, autoantibodies are involved in the development of AA as immunological factors [4]. Here, we report a case of AA that developed after the administration of a SARS-CoV-2 vaccine and discuss the association between AA and vaccination.
2. Case description
A previously healthy 56-year-old male, who was not taking any medication, was referred to a clinic because of bleeding in the oral cavity after dental therapy. Laboratory tests showed that his white blood cell count (1.6 × 109/l) and platelet count (11 × 109/l) were decreased. Four days before his visit to the clinic, he had received a second dose of the Pfizer-BioNTech mRNA vaccine (three weeks after his first dose). He was admitted to our hospital due to progressive pancytopenia (Supplementary Table 1). He had no history of COVID-19 infection. The Elecsys® anti-SARS-CoV-2 immunoassay (Roche, Basel, Switzerland), which is used to detect anti-SARS-CoV-2 nucleocapsid protein antibodies, produced a negative result. Tests for immunoglobulin G against cytomegalovirus and Epstein-Barr virus produced positive results, but were not indicative of virus reactivation. Serological tests for hepatitis B, hepatitis C, and human immunodeficiency virus produced negative results. A bone marrow biopsy revealed a hypocellular marrow (Fig. 1 ). The patient was diagnosed with very severe AA [6]. Human leukocyte antigen (HLA) testing showed DRB1 04:05 04:05, which is not associated with a high frequency of AA. The administration of granulocyte-colony stimulating factor had no effect on his neutropenia. In spite of the administration of cyclosporine and eltrombopag, his pancytopenia progressed.

Histological findings of the bone marrow biopsy specimen at diagnosis. Panel A: Hematoxylin and eosin (H.E.) staining (x40) of the bone marrow after the administration of a SARS-CoV-2 vaccine showed a markedly hypocellular marrow. Panel B: H.E. staining (x400) showed the replacement of hematopoietic cells by fat and a few nucleated cells.
He underwent an allogeneic hematopoietic stem cell transplantation (HSCT) from an HLA haploidentical related donor (Fig. 2 ). The donor had no history of COVID-19 infection and had not received a SARS-CoV-2 vaccine. The conditioning regimen consisted of 120 mg/m2 fludarabine, 100 mg/kg cyclophosphamide, 2.5 mg/kg anti-thymocyte globulin, and 2 Gy of total body irradiation. Tacrolimus and short-term methotrexate were used as a prophylaxis against graft-versus-host disease (GVHD). Post-transplant cyclophosphamide was not administered because the patient’s HLA-A, C, and DR were homologous, which would not increase the risk of GVHD. The transplanted cells collected from the donor’s bone marrow were transfused into the patient after the removal of red blood cells and plasma. Twenty-one days after the HSCT, neutrophil engraftment was achieved. Chimerism analysis performed on day 29 after the HSCT revealed complete chimerism in the peripheral blood. The patient developed acute GVHD (skin grade 1), which was ameliorated with a topical corticosteroid alone.

Evaluation of neutrophil count, The X-axis indicates the number of days after the 2nd dose of the COVID-19 vaccine was administered. The allogeneic BMT was conducted at 34 days after the 2nd dose of the COVID-19 vaccine was administered. The gray boxes indicate the titers of antibodies against the SARS-CoV-2 spike protein (log scale). BMT, bone marrow transplantation; COVID-19, coronavirus disease 2019; CyA, cyclosporine A; TAC, tacrolimus.
The titers of antibodies against SARS-CoV-2 were measured before and after the HSCT to examine the association between the SARS-CoV-2 vaccine the patient received and the development of AA. The measurement of anti-SARS-CoV-2 spike protein antibody titers was performed by SRL, Inc. (Tokyo, Japan) using the Elecsys® anti-SARS-CoV-2 S immunoassay (Roche, Basel, Switzerland). The titers of antibodies against SARS-CoV-2 before the conditioning regimen and 63 days after the HSCT were 540 and 34.9 U/mL (reference range, <0.8 U/mL), respectively (Fig. 2). These results suggest that the AA was ameliorated by the allogeneic HSCT even though anti-SARS-CoV-2 spike protein antibodies continued to be detected after the HSCT.Go to:
3. Discussion
We report a case in which AA developed after the administration of a SARS-CoV-2 vaccine. No association between new-onset AA and SARS-CoV-2 vaccines has been reported. The patient in this case underwent allogeneic HSCT. In this patient, antibodies against the SARS-CoV-2 spike protein were detected both before and after the HSCT. After the allogeneic HSCT, the patient’s AA was ameliorated despite the presence of antibodies against SARS-CoV-2. Our results did not reveal a direct association between antibodies derived from the SARS-CoV-2 vaccine and the development of AA. Further studies are needed to investigate the impairment of hematopoiesis induced by immune reactions after SARS-CoV-2 vaccine administration.
One of the most feared adverse reactions to vaccines is the development of autoimmune disease. To the best of our knowledge, only six cases of newly diagnosed acquired AA have been reported after vaccination [[7], [8], [9], [10], [11]] (Table 1 ). However, in general, AA is not recognized as a vaccine-related adverse event [12]. The mRNA vaccines against SARS-CoV-2 have a novel mechanism of action. Therefore, it is important to collect information about their adverse events. Various cases of autoimmune disease have been reported after SARS-CoV-2 vaccine administration, including autoimmune hepatitis, type 1 diabetes mellitus, immune thrombocytopenia, and acquired hemophilia [3,[13], [14], [15]]. Patients with AA after COVID-19 infection were also reported [16,17]. Further epidemiological evaluations of the incidence of AA after COVID-19 infection and SARS-CoV-2 vaccination are warranted.
Table 1
Reported cases of newly diagnosed aplastic anemia after vaccinations.
| Age (years) | Sex | Vaccine | Time to symptom onset | Treatment | Outcome | Reference |
|---|---|---|---|---|---|---|
| 16 | F | Recombinant hepatitis B | 3 weeks after 3rd dose | Corticosteroid | Improved | Viallard et al. [7] |
| 19 | F | Recombinant hepatitis B | 10 days after 3rd dose | Corticosteroid | Improved | Ashok Shenoy et al. [8] |
| 25 | M | Hepatitis B | 7 days after 2nd dose | Allogeneic HSCT | N.A. | Shah et al. [9] |
| 19 | M | Anthrax | 1 month | Allogeneic HSCT | N.A. | Shah et al. [9] |
| 1.5 | F | Varicella zoster | 3 weeks | None | Improved | Angelini et al. [10] |
| 25 | M | H1N1 influenza | 2 weeks | Allogeneic HSCT | Improved | Donnini et al. [11] |
| 56 | M | SARS-Cov-2 | 4 days after 2nd dose | Allogeneic HSCT | Improved | This case |
HSCT, hematopoietic stem cell transplantation; N.A., not applicable; SARS-Cov-2, severe acute respiratory syndrome coronavirus 2.
Various cases of vaccine-related autoimmune disease have been reported. Most of these reports have linked vaccination to the development of autoimmune disease based on clinical observations of temporal associations. There is no established method for examining the relationships between vaccines and the development of autoimmune diseases. The pathogenetic mechanisms by which vaccines cause the development of autoimmune disease are still unclear. The major hypotheses relating to such immunological reactions involve epitope mimicry [18,19]. For example, it has been reported that vaccine-derived antibodies may exhibit structural similarities with autoantibodies [18,19]. There is significant evidence that AA is an immune-mediated condition, mainly based on the effectiveness of immunosuppressive therapy against AA. In addition to T cells and cytokines, autoantibodies are one of the factors that contribute to the pathogenesis of AA [4]. However, autoantibodies specific to AA and the role of autoantibodies for the pathogenesis of AA are unclear. The allogeneic HSCT replaces the recipient’s hematopoietic and associated immune systems with those of the donor. The measurement of vaccine antibody titers before and after allogeneic HSCT may provide a clue to the pathogenesis of vaccine-related autoimmune diseases. The clonal expansion of effector T cells was also reported to occur following vaccination [20]. To understand the link between COVID-19 vaccination and the development of AA, the following needs to be examined: the exploration of autoantibodies against stem cells, the role for molecular mimicry between mRNA vaccine encoded antigens and stem cells, and T-cell subset dynamics after vaccination.
In conclusion, the administered SARS-CoV-2 mRNA vaccine may have contributed to the pathogenesis of AA in this case. However, it is not clear whether antibodies derived from the SARS-CoV-2 vaccine directly contributed to the development of AA because the anti-SARS-CoV-2 antibodies remained after the patient’s pancytopenia had been ameliorated by the allogeneic HSCT. Further evaluations in large cohorts are warranted to elucidate the associations between AA and SARS-CoV-2 vaccines.Go to:
Authors’ contributions
Shotaro Tabata: Data curation, Investigation, Writing – original draft; Hiroki Hosoi: Conceptualization, Data curation, Investigation, Writing – original draft and Review & Editing; Shogo Murata: Investigation, Writing – review & editing; Satomi Takeda: Data curation, Writing – review & editing; Toshiki Mushino: Writing – review & editing; Takashi Sonoki: Writing – review & editing, Supervision.Go to:
Declaration of competing interest
There are no funding sources associated with the writing of this manuscript. Written consent for publication was obtained from the patient.Go to:
Acknowledgements
We thank the patients and clinical staff at Wakayama Medical University Hospital for their participation in this study. We also wish to thank Dr. Takashi Ozaki and Mr. Masaya Morimoto from Kinan Hospital for their helpful diagnostic support.Go to:
Footnotes
Appendix ASupplementary data to this article can be found online at https://doi.org/10.1016/j.jaut.2021.102782.Go to:
Appendix A. Supplementary data
The following is the Supplementary data to this article:Multimedia component 1:Click here to view.(12K, xlsx)Multimedia component 1Go to:
References
1. Arepally G.M., Ortel T.L. Vaccine-induced immune thrombotic thrombocytopenia: what we know and do not know. Blood. 2021;138:293–298. https://doi:10.1182/blood.2021012152 [PMC free article] [PubMed] [Google Scholar]
2. Lee E.J., Cines D.B., Gernsheimer T., Kessler C., Michel M., Tarantino M.D., et al. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am. J. Hematol. 2021;96:534–537. https://doi:10.1002/ajh.26132 [PMC free article] [PubMed] [Google Scholar]
3. Vuille-Lessard E., Montani M., Bosch J., Semmo N. Autoimmune hepatitis triggered by SARS-CoV-2 vaccination. J. Autoimmun. 2021;123 https://doi:10.1016/j.jaut.2021.102710 [PMC free article] [PubMed] [Google Scholar]
4. Dolberg O.J., Levy Y. Idiopathic aplastic anemia: diagnosis and classification. Autoimmun. Rev. 2014;13:569–573. https://doi:10.1016/j.autrev.2014.01.014 [PubMed] [Google Scholar]
5. Young N.S. Aplastic Anemia. N. Engl. J. Med. 2018;379:1643–1656. https://doi:10.1056/NEJMra1413485 [PMC free article] [PubMed] [Google Scholar]
6. Killick S.B., Bown N., Cavenagh J., Dokal I., Foukaneli T., Hill A., et al. Guidelines for the diagnosis and management of adult aplastic anaemia. Br. J. Haematol. 2016;172:187–207. https://doi:10.1111/bjh.13853 [PubMed] [Google Scholar]
7. Viallard J.F., Boiron J.M., Parrens M., Moreau J.F., Ranchin V., Reiffers J., et al. Severe pancytopenia triggered by recombinant hepatitis B vaccine. Br. J. Haematol. 2000;110:230–233. https://doi:10.1046/j.1365-2141.2000.02171.x [PubMed] [Google Scholar]
8. Ashok Shenoy K., Prabha Adhikari M.R., Chakrapani M., Shenoy D., Pillai A. Pancytopenia after recombinant hepatitis B vaccine–an Indian case report. Br. J. Haematol. 2001;114 https://doi:10.1046/j.1365-2141.2001.03006-2.x [PubMed] [Google Scholar]
9. Shah C., Lemke S., Singh V., Gentile T. Case reports of aplastic anemia after vaccine administration. Am. J. Hematol. 2004;77 https://doi:10.1002/ajh.20153 [PubMed] [Google Scholar]
10. Angelini P., Kavadas F., Sharma N., Richardson S.E., Tipples G., Roifman C., et al. Aplastic anemia following varicella vaccine. Pediatr. Infect. Dis. J. 2009;28:746–748. https://doi:10.1097/INF.0b013e31819b6c1f [PubMed] [Google Scholar]
11. Donnini I., Scappini B., Guidi S., Longo G., Bosi A. Acquired severe aplastic anemia after H1N1 influenza virus vaccination successfully treated with allogeneic bone marrow transplantation. Ann. Hematol. 2012;91:475–476. https://doi:10.1007/s00277-011-1278-0 [PubMed] [Google Scholar]
12. Dudley M.Z., Halsey N.A., Omer S.B., Orenstein W.A., O’Leary S.T., Limaye R.J., et al. The state of vaccine safety science: systematic reviews of the evidence. Lancet Infect. Dis. 2020;20:e80–e89. https://doi:10.1016/S1473-3099(20)30130-4 [PubMed] [Google Scholar]
13. Patrizio A., Ferrari S.M., Antonelli A., Fallahi P. A case of Graves’ disease and type 1 diabetes mellitus following SARS-CoV-2 vaccination. J. Autoimmun. 2021;125 https://doi:10.1016/j.jaut.2021.102738 [PMC free article] [PubMed] [Google Scholar]
14. Tarawneh O., Tarawneh H. Immune thrombocytopenia in a 22-year-old post Covid-19 vaccine. Am. J. Hematol. 2021;96:E133–E134. https://doi:10.1002/ajh.26106 [PMC free article] [PubMed] [Google Scholar]
15. Radwi M., Farsi S. A case report of acquired hemophilia following COVID-19 vaccine. J. Thromb. Haemostasis. 2021;19:1515–1518. https://doi:10.1111/jth.15291 [PMC free article] [PubMed] [Google Scholar]
16. Avenoso D., Marsh J.C.W., Potter V., Pagliuca A., Slade S., Dignan F., et al. SARS-CoV-2 Infection in Aplastic Anaemia. Haematologica. 2021 https://doi:10.3324/haematol.2021.279928 [PMC free article] [PubMed] [Google Scholar]
17. Chakravarthy R., Murphy M.L., Ann Thompson M., McDaniel H.L., Zarnegar-Lumley S., Borinstein S.C. SARS-CoV-2 infection coincident with newly diagnosed severe aplastic anemia: a report of two cases. Pediatr. Blood Cancer. 2021 https://doi:10.1002/pbc.29433 [PMC free article] [PubMed] [Google Scholar]
18. Wraith D.C., Goldman M., Lambert P.H. Vaccination and autoimmune disease: what is the evidence? Lancet. 2003;362:1659–1666. https://doi:10.1016/S0140-6736(03)14802-7 [PubMed] [Google Scholar]
19. Vadala M., Poddighe D., Laurino C., Palmieri B. Vaccination and autoimmune diseases: is prevention of adverse health effects on the horizon? EPMA J. 2017;8:295–311. https://doi:10.1007/s13167-017-0101-y [PMC free article] [PubMed] [Google Scholar]
20. Ritz C., Meng W., Stanley N.L., Baroja M.L., Xu C., Yan P., et al. Postvaccination graft dysfunction/aplastic anemia relapse with massive clonal expansion of autologous CD8+ lymphocytes. Blood Adv. 2020;4:1378–1382. https://doi:10.1182/bloodadvances. 2019000853 [PMC free article] [PubMed] [Google Scholar]