By Lisa L. Colangelolisa.colangelo@newsday.com@lisalcolangelo, Newsday
People who have had multiple bouts of COVID-19, had it severely, and those who were unvaccinated when first infected had an increased risk of developing long COVID, according to a new study by researchers at the Renaissance School of Medicine at Stony Brook University in conjunction with the Stony Brook World Trade Center Health and Wellness Program.
The study looked at 2,522 people in the program who had a positive COVID-19 test between March 2020 and February 2024 and determined 475 had long COVID. Of that number, 403 or almost 85%, had been infected with the virus that causes COVID several times.
Everyone in the study was considered an essential worker and most were first responders. The program treats and monitors people with health problems related to the Sept. 11, 2001, terrorist attacks.
“We found a significant association” between the risk of long COVID and multiple re-infections, severity and vaccination status at first infection, according to the report, published this month in “The Lancet Regional Health-Americas” journal.
The study said a “large proportion” of participants who were not vaccinated at the time of their first infection experienced long COVID.
Lead author and Stony Brook professor Sean Clouston said researchers accounted for different medical conditions but that age and gender didn’t really make a difference other than if they contributed to the severity of the infections.
“We had some younger people who had more severe COVID that was associated with a higher risk of long COVID,” said Clouston, a professor in the department of Family, Population and Preventative Medicine at the Renaissance School of Medicine.
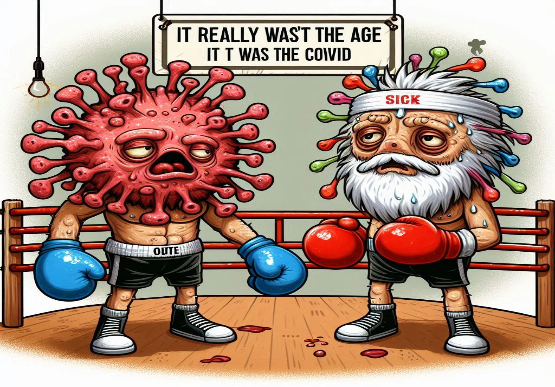
“It really wasn’t the age anymore, it was the COVID.”
Long COVID, also known as post-acute sequelae, has a number of symptoms ranging from mental fog, loss or altered sense of taste and smell to wheezing, coughs and chest pain.
People who have continuing or new symptoms three months after they contract COVID-19 are classified as having long COVID, with symptoms lasting at least two months.
Experts say the continuing study of long COVID is vital, because while deaths and severe illness from COVID-19 have dropped since the early days of the pandemic, there are still many questions about the lingering impacts of an infection and it’s still not fully understood.
“Long COVID is now the threat,” said Dr. Reynold A. Panettiere, Jr., vice chancellor at the Rutgers Institute for Translational Medicine and Science who was not involved in the study.
“Before it was death. People didn’t want to go into intensive care and be on a ventilator,” he said. “Now if you get it and you get it more frequently, the potential for long COVID and sustained symptoms is greater.”
While the COVID-19 vaccines have been important in decreasing the number of people who get severely sick and die from the disease, they have not prevented or stopped infections, said Dr. Benjamin Luft, an infectious disease specialist and director of the Stony Brook World Trade Center Health and Wellness Program, co-author of the study.
“Long COVID-19 has been so debilitating and so harmful that you really need something that is effective against that — whether that’s a vaccine or a therapeutic,” Luft said.
The number of people getting the COVID-19 vaccine overall has dropped compared to initial years, as some people express frustration with its inability to prevent infections, though the rate grew in 2024 compared to the prior year.
“Instead of saying ‘We’re not going to get the vaccine,’ people should be asking for a better vaccine … one that prevents the infection,” he said. “We need new and better strategies for the development of the next generation vaccine.”