Authors: Aneel A. Ashrani, MD, MS1; Daniel J. Crusan, BS2; Tanya Petterson, MS2; et al
JAMA Intern Med. 2022;182(1):80-83. doi:10.1001/jamainternmed.2021.6352
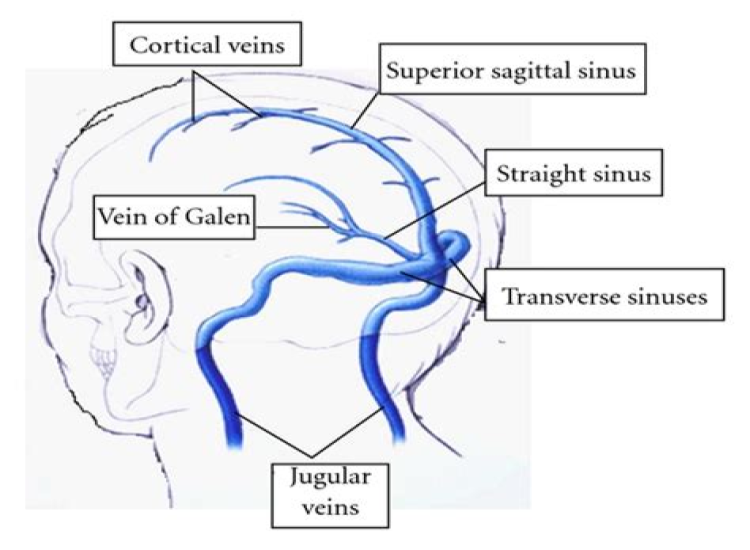
Recent reports1–4 suggest a possible association between Ad26.COV2.S (Johnson & Johnson/Janssen) COVID-19 vaccination and cerebral venous sinus thrombosis (CVST). Estimates of postvaccination CVST risk require accurate age- and sex-specific prepandemic CVST incidence rates; however, reported rates vary widely.5 We compared the age- and sex-specific CVST rates after Ad26.COV2.S vaccination with the prepandemic CVST rate in the population.Methods
In this population-based cohort study, to estimate the risk of CVST after Ad26.COV2.S vaccination, we first identified all incident cases of CVST in Olmsted County, Minnesota from January 1, 2001, through December 31, 2015 (eMethods in the Supplement). Sex-and age-adjusted incidence rates were adjusted to the 2010 US census population. We used CDC Vaccine Adverse Event Reporting System (VAERS) data from February 28, 2021 (vaccine approval date) to May 7, 2021, to estimate the incidence of CVST after Ad26.COV2.S vaccination assuming 3 (15, 30, and 92 days) plausible postvaccination periods during which individuals were considered to be at risk of CVST. We then compared post-Ad26.COV2.S vaccination CVST rates with prepandemic rates to estimate postvaccination CVST risk. This study was approved by the Mayo Clinic institutional review board. Medical records of Olmsted County residents with CVST were reviewed only if the residents had signed an authorization for accessing their medical records for research purposes. SAS, version 9.4 (SAS Institute Inc) and R, version 4.0.3 (R Project for Statistical Computing) were used for statistical analyses. Significance was set at a 2-sided P < .05.Results
From 2001 through 2015, 39 Olmsted County residents developed acute incident CVST. A total of 29 patients (74.4%) had a predisposing venous thromboembolism risk factor (eg, infection, active cancer, or oral contraceptives [for women]) within 92 days before the event. The median age at diagnosis was 41 years (range, 22-84 years); 22 residents with CVST (56.4%) were female. The overall age- and sex-adjusted CVST incidence was 2.34 per 100 000 person-years (PY) (95% CI, 1.60-3.08 per 100 000 PY). Age-adjusted CVST rates for female and male individuals were 2.46 per 100 000 PY (95% CI, 1.43-3.49 per 100 000 PY) and 2.34 per 100 000 PY (95% CI, 1.22-3.46 per 100 000 PY), respectively. Men aged 65 years or older had the highest CVST rate (6.22 per 100 000 PY; 95% CI, 2.50-12.82 per 100 000 PY), followed by women aged 18 to 29 years (4.71 per 100 000 person-years; 95% CI, 2.26-8.66 per 100 000 PY) (Table 1).
As of May 7, 2021, 8 727 851 Ad26.COV2.S vaccine doses had been administered in the US; 46 potential CVST events occurring within 92 days after Ad26.COV2.S vaccination were reported to VAERS. Eight events were excluded because they were potentially duplicate reports (4) or were not objectively diagnosed (4). Twenty-seven of 38 objectively diagnosed cases of CVST after Ad26.COV2.S vaccination (71.1%) occurred in female individuals. The median patient age was 45 years (range, 19-75 years). The median time from vaccination to CVST was 9 days (IQR, 6-13 days; range, 1-51 days); 31 of 38 cases of CVST (81.6%) occurred within 15 days after vaccination, and 36 (94.7%) occurred within 30 days.
The overall incidence rate of post–Ad26.COV2.S vaccination CVST was 8.65 per 100 000 PY (95% CI, 5.88-12.28 per 100 000 PY) at 15 days, 5.02 per 100 000 PY (95% CI, 3.52-6.95 per 100 000 PY) at 30 days, and 1.73 per 100 000 PY (95% CI, 1.22-2.37 per 100 000 PY) at 92 days (Table 2). The 15-day postvaccination CVST incidence rates for female and male individuals were 13.01 per 100 000 PY (95% CI, 8.24-19.52 per 100 000 PY) and 4.41 per 100 000 PY (95% CI, 1.90-8.68 per 100 000 PY), respectively. The postvaccination CVST rate among females was 5.1-fold higher compared with the pre-COVID-19 pandemic rate (13.01 vs 2.53 per 100 000 PY; P < .001) (Table 2). This risk was highest among women aged 40 to 49 years (29.50 per 100 000 PY; 95% CI, 13.50-55.95 per 100 000 PY), followed by women aged 30 to 39 years (26.50 per 100 000 PY; 10.65-54.63 per 100 000 PY).Discussion
In this population-based cohort study, we found that the CVST incidence rate 15 days after Ad26.COV2.S vaccination was significantly higher than the prepandemic rate. However, the higher rate of this rare adverse effect must be considered in the context of the effectiveness of the vaccine in preventing COVID-19 (absolute reduction of severe or critical COVID-19 of 940 per 100 000 PY).6
Most CVST events occurred within 15 days after vaccination, which is likely the highest at-risk period. The postvaccination CVST rate among females was higher than the prepandemic rate among females. The highest risk was among women aged 30 to 49 years, but the absolute CVST risk was still low in this group (up to 29.5 per 100 000 PY among women aged 40-49 years). The reason that women had a higher incidence of postvaccination CVST is unclear; concomitant CVST risk factors or autoantibody production might have been involved.2 The overall prepandemic CVST incidence rate was slightly higher in our study than in other studies (0.22-1.57 per 100 000 PY)5 likely because we captured all objectively diagnosed incident CVST cases in a well-defined population, including those discovered at autopsy.
The present study avoided referral bias and included only objectively diagnosed and confirmed cases. Only cases with adequate details or imaging findings reported on VAERS were used. Study limitations include possible ascertainment bias by including only objectively diagnosed CVST cases. VAERS reporting is voluntary and subject to reporting biases. VAERS monitors vaccine adverse events but does not prove causality.Back to topArticle Information
Accepted for Publication: September 12, 2021.
Published Online: November 1, 2021. doi:10.1001/jamainternmed.2021.6352
Corresponding Author: Aneel A. Ashrani, MD, MS, Division of Hematology, Department of Internal Medicine, Mayo Clinic, 200 First St SW, Rochester, MN 55905 (ashrani.aneel@mayo.edu).
Author Contributions: Dr Ashrani and Mr Crusan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Ashrani, Petterson, Bailey, Heit.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Ashrani, Crusan, Petterson.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Crusan, Petterson, Bailey.
Obtained funding: Ashrani, Heit.
Administrative, technical, or material support: Ashrani, Heit.
Supervision: Ashrani, Petterson, Bailey, Heit.
Conflict of Interest Disclosures: Dr Ashrani reported receiving grants from the National Heart, Lung and Blood Institute (NHLBI), National Institutes of Health (NIH) during the conduct of the study. Mr Crusan reported receiving grants from the NIH during the conduct of the study. Dr Heit reported receiving grants from the NHLBI, NIH during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was supported in part by grant R01HL66216 from the NHLBI, NIH (Drs Ashrani and Bailey), the Rochester Epidemiology Project (grant R01AG034676 from the National Institute on Aging, NIH), and the Mayo Foundation.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
1.Centers for Disease Control and Prevention. Cases of cerebral venous sinus thrombosis with thrombocytopenia after receipt of the Johnson & Johnson COVID-19 vaccine New release. April 13, 2021. Accessed April 21, 2021. https://emergency.cdc.gov/han/2021/han00442.asp
2.See I, Su JR, Lale A, et al. US case reports of cerebral venous sinus thrombosis with thrombocytopenia after Ad26.COV2.S vaccination, March 2 to April 21, 2021. JAMA. 2021;325(24):2448-2456. doi:10.1001/jama.2021.7517
ArticlePubMedGoogle ScholarCrossref
3.Shay DK, Gee J, Su JR, et al. Safety monitoring of the Janssen (Johnson & Johnson) COVID-19 vaccine—United States, March-April 2021. MMWR Morb Mortal Wkly Rep. 2021;70(18):680-684. doi:10.15585/mmwr.mm7018e2PubMedGoogle ScholarCrossref
4.Shimabukuro T. Update: thrombosis with thrombocytopenia syndrome (TTS) following COVID-19 vaccination. Paper presented at: Advisory Committee on Immunization Practices; May 12, 2021.
5.Devasagayam S, Wyatt B, Leyden J, Kleinig T. Cerebral venous sinus thrombosis incidence is higher than previously thought: a retrospective population-based study. Stroke. 2016;47(9):2180-2182. doi:10.1161/STROKEAHA.116.013617PubMedGoogle ScholarCrossref
6.Sadoff J, Gray G, Vandebosch A, et al; ENSEMBLE Study Group. Safety and efficacy of single-dose Ad26.COV2.S vaccine against COVID-19. N Engl J Med. 2021;384(23):2187-2201. doi:10.1056/NEJMoa2101544PubMedGoogle ScholarCrossref