Authors: Ariana Eunjung Cha February 21, 2022

Five months after being infected with the coronavirus, Nicole Murphy’s pulse rate is going berserk. Normally in the 70s, which is ideal, it has been jumping to 160, 170 and sometimes 210 beats per minute even when she is at rest — putting her at risk of a heart attack, heart failure or stroke.
No one seems to be able to pinpoint why. She’s only 44, never had heart issues, and when a cardiologist near her hometown of Wellsville, Ohio, ran all of the standard tests, “he literally threw up his hands when he saw the results,” she recalled. Her blood pressure was perfect, there were no signs of clogged arteries, and her heart was expanding and contracting well.
Murphy’s boomeranging heart rate is one of a number of mysterious conditions afflicting Americans weeks or months after coronavirus infections that suggest the potential of a looming cardiac crisis.
A pivotal study that looked at health records of more than 153,000 U.S. veterans published this month in Nature Medicine found that their risk of cardiovascular disease of all types increased substantially in the year following infection, even when they had mild cases. The population studied was mostly White and male, but the patterns held even when the researchers analyzed women and people of color separately. When experts factor in the heart damage probably suffered by people who put off medical care, more sedentary lifestyles and eating changes, not to mention the stress of the pandemic, they estimate there may be millions of new onset cardiac cases related to the virus, plus a worsening of disease for many already affected.
“We are expecting a tidal wave of cardiovascular events in the coming years from direct and indirect causes of covid,” said Donald M. Lloyd-Jones, president of the American Heart Association.
In February 2021, the National Institutes of Health launched an initiative to look at the causes and possible treatments for long covid, the constellation of symptoms from brain fog and exercise fatigue to heart-related issues that some people experience well past their initial infections. In addition, the American College of Cardiology has recognized the serious, longer-term effects of the coronavirus by preparing new guidelines, scheduled out in March, for monitoring and returning to exercise after infection. But many experts and patient advocacy groups say more is needed, and are calling on President Biden and other leaders for comprehensive changes in the health care system that would provide more funding for research and treatment, financial support for people who can no longer work and address the social and emotional consequences of illness in the decades to come.
Zaza Soriano, 32, a software engineer from Millersville, Md., who works for a NASA subcontractor, got covid right before Christmas despite being fully vaccinated and boosted, and since then, her blood pressure has remained very high with the bottom number, or diastolic pressure when the heart rests between beats sometimes as high as 110 when it should be lower than 80. She also has brain fog and her joints ache.
“It’s so frustrating we still know so little about why this is happening,” she said.
Ziyad Al-Aly, an assistant professor of medicine at Washington University and a Veterans Affairs physician who co-authored the Nature Medicine study, describes the pandemic as an earthquake. “When the earth stops shaking and the dust settles, we will have to be able to deal with the aftermath on heart and other organ systems,” he said.
“Governments around the world need to pay attention,” Al-Aly emphasized. “We are not sufficiently prepared.”
Heart disease is the planet’s No. 1 killer, responsible for 17.9 million deaths, or a third of the total each year before the pandemic, and there’s already growing evidence of the outsize impact the coronavirus is having on our long-term health.
Multiple studies suggest that Americans’ collective blood pressures has jumped since the crisis began. According to a December study in the journal Circulation, for example, the average blood pressure among a half-million U.S. adults studied from April to December 2020 went up each month for both of the numbers measured by monitors.
The Centers for Disease Control and Prevention as of this month had logged more than 1 million excess deaths or deaths since the start of the pandemic that are beyond what we would have expected in normal times. While most of those were directly caused by the virus, there were also an additional 30,000 deaths due to ischemic heart disease and nearly 62,000 additional deaths due to hypertensive disease.
When the coronavirus first hit the United States in 2020, doctors were surprised by the heart involvement in cases they saw: professional athletes with signs of myocarditis or hardening of the heart walls; patients dying from their illness with hundreds of tiny clots in major organs; children rushed to emergency rooms with an inflammatory reaction involving cardiac complications.
Many of those presentations turned out to be rare or rarely serious. But they led researchers to an important discovery: that SARS-CoV-2 could directly attack the heart and blood vessels, in addition to the lungs.
Myocarditis has mostly been a transient issue, impacting activity or becoming life-threatening in only a small minority of cases; the clotting is more widespread but something that usually can be controlled with blood thinners; and the pediatric inflammatory syndrome has affected only about 6,400 children out of millions of cases, as of January.
The idea that infections increase cardiovascular risk is not new. It has been documented in cases of influenza and other viruses as well. But in coronavirus, that impact seems “enhanced,” said Antonio Abbate, a professor of cardiology at the VCU Pauley Heart Center. And the early and obvious cases, he said, should serve “as a kind of warning” for the type of longer-term cases we may see into the future.
Indeed, as the months since their infections have turned into years, people who initially had mild or even some asymptomatic coronavirus cases are pouring into cardiology practices across the country.
At Memorial Hermann-Texas Medical Center in Houston, Abhijeet Dhoble, an associate professor of cardiovascular medicine, said they are seeing an increase in arrhythmia, an abnormality in the timing of the heartbeat, and cardiomyopathy, a heart muscle disease. The patients, who previously had covid, range in age from their 30s to 70s and many had no previous heart disease.
“We are seeing the same patterns at university clinics and the hospital,” he said.
Two different processes may be at play, according to David Goff, director of the National Heart, Lung and Blood Institute’s division of cardiovascular sciences. The virus may inflict direct damage to the heart muscle cells, some of which could die, resulting in a weaker heart that does not pump as well. Another possibility is that after causing damage to blood vessels through clots and inflammation, the healing process involves scarring that stiffens vessels throughout the body, increasing the work of the heart.
“It could lead over time to failure of the heart to be able to keep up with extra work,” he explained.
Blood vessels and fatigue
David Systrom, a pulmonary and critical care doctor at Brigham and Women’s Hospital in Boston, said he believes blood vessel damage may be responsible for one of the most common and frustrating symptoms of long covid — fatigue.
Systrom and his colleagues recruited 20 people who were having trouble exercising. Ten had long covid. The other half had not been infected with the virus. He inserted catheters into their veins to provide test information before putting them on stationary bikes and took a number of detailed measurements. The study was published in the journal Chest in January.
In the long covid group, he found that they had normal lung function and at peak exercise, their oxygen levels were normal even as they were short of breath. What was abnormal was that some veins and arteries did not appear to be delivering oxygen efficiently to the muscles.
He theorized this could be due to a malfunction in the body’s autonomic nervous system, which controls involuntary actions such as the rate at which the heart beats, or the widening or narrowing of blood vessels.
“When exercising, it acts like a traffic cop that distributes blood flow to muscles away from organ systems like the kidney and gut that don’t need it. But when that is dysfunctional, what results is inadequate oxygen extraction,” he said. That may lead to the feeling of overwhelming exhaustion that covid long haulers are experiencing.
The overall the message from providers is that “covid by itself is a risk factor for heart disease” like obesity, diabetes, or high blood pressure, according to Saurabh Rajpal, a cardiologist at Ohio State University Wexner Medical Center.
“This is a virus that really knocks people down,” agreed Nicole Bhave, a cardiologist with Michigan Medicine and member of the American College of Cardiology’s science committee. “Even young, healthy people don’t often feel very normal for weeks to months, and it’s a real challenge to distinguish what’s just your body slowly healing versus a new pathological problem.”
“People experiencing what appear to be heart issues should have a “a low threshold for seeing their primary care doctor,” she said.
Heart beats
Unexplained high blood pressure has been a common symptom after covid infection.
Lindsay Polega, 28, an attorney from St. Petersburg, Fla., had never had any medical issues before covid. She had been an all-state swimmer in high school and ran, swam or otherwise exercised an hour or more every day since. But after two bouts with covid, the first in early 2020 and the second in spring 2021, she’s been having what doctors call “hypertensive spikes” that result in shooting pains in her chest that make her shaky and weak. During those incidents, which sometimes occur a few times a day, her blood pressure has gone as high as 210/153 — far above the 120/80, that is considered normal.
One incident happened during a light Pilates class and she had to go to the emergency room. Other times, it has happened while walking. “Sometimes I’ll just be on the couch,” she said.
Each specialist she saw referred her to another — endocrinology, immunology, cardiology, neurology. Finally, she found herself at a long-covid clinic where the doctor theorized the issue may be with her adrenal gland. Scientists have documented that the virus can target the adrenal glands, which produce hormones that help regulate blood pressure among other essential functions. Polega was put on a heavy-duty blood pressure drug called eplerenone that’s typically used in patients after a heart attack, and it has helped to reduce but not eliminate the episodes.
The scariest part for Polega is that women taking eplerenone are cautioned against pregnancy due to research in animals showing low birth weights and other potential dangers. Polega and her boyfriend of six years had recently purchased a house together, and were talking about starting a family soon.
“That’s a big thing to have taken away at my age — my future,” she said.
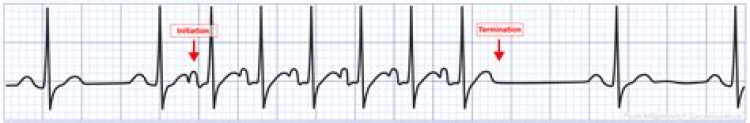
Of all the symptoms of long covid, among the most baffling have been erratic heart rates and skipped heartbeats with no clear cause.
Tiffany Brakefield, a 36-year-old pharmacy tech from Bonita Springs, Fla., who had covid in June 2020, said the spikes are so unpredictable that she found herself having to sit down on the floor at Walmart during a recent shopping excursion.
“I felt like I was going to fall down, and all I could do was wait for it to calm down on its own,” she said. Her doctors had put her on a heart medication, metoprolol, but it has not helped.
Rick Templeton, a 52-year-old community college instructor in Lynchburg, Va., felt chest tightness along with a racing heart rate, but in his case it disappeared five to six months after his infection in September 2020, and doctors never knew why it happened because his test results were normal.
Rajpal, the cardiologist in Ohio, said a large majority of his post-covid cases are similarly vexing.
“The most common type of long haulers we are seeing have shortness of breath, chest discomfort, and fast heart rate. But when we investigate them for heart disease they come back as normal,” he said.
Goff, the NIH scientist, said the presentation looks similar to a condition known as POTS, or postural orthostatic tachycardia syndrome, in which symptoms such as lightheadedness and heart rate changes are related to reduced blood volume, typically worsened by changing positions. A body of emerging evidence suggests that for many people, it could be a post-viral syndrome.
He said the unstable heart rate for many post-covid patients “can be quite serious and debilitating, and can really interfere with ordinary day-to-day activities.” Doctors can use blood pressure medications to try to stabilize heart rates but because they depress blood pressures at the same time, they can be tricky to use.
Murphy, the Ohio long covid patient, said that when her heart rate soars, which happens several times an hour, she said “it feels like a hamster in my chest.”
Her troubles began on Sept. 5, when she and her teenage daughter tested positive for the virus. Her daughter got over her illness in a few days. Murphy was acutely ill for about three weeks, and many of her symptoms never went away.
The 44-year-old single mom says she’s extraordinarily weak and has trouble with her memory sometimes. Before she was infected, she worked 12-hour days as a day care provider, a waitress and a cashier. Now she’s lucky if she can last three to four hours at her job as a DoorDash driver.
She’s tried to stay active by taking walks but sometimes “when I take steps, it’ll be like stars.” When she saw the cardiologist, she passed out during the stress test on the treadmill.
“I constantly live in fear I’m going to have a heart attack or stroke,” she said.
After all her heart tests came back fine except for her EKG, which showed the jumping heart rate, her doctors referred her to the Cleveland Clinic’s long covid group. She hopes they will help her find answers.