By Lana Barhum November 16, 2022
Medically reviewed by Susan Russell, MD
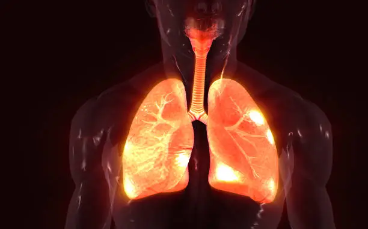
Interstitial lung disease (ILD) includes more than 200 conditions that cause inflammation and scarring of lung tissue.1 The damage done by interstitial lung disease makes it harder for oxygen to enter the bloodstream from the air sacs of the lungs.
The prevalence of ILD in the US is 179.7 out of 100,000 In males and 218.9 out of 100,000 In females.2 Here is what you need to know about interstitial lung disease, including types, causes, symptoms, diagnosis, and treatment.
Types of Interstitial Lung Disease
All types of interstitial lung disease affect the interstitium, a system of tissues running through the lungs. The interstitium supports the alveoli, the tiny balloon-like sacs of the lungs. Blood vessels travel through the interstitium, allowing for the blood to receive oxygen and rid the body of any excess carbon dioxide. Most disorders of the interstitium thicken lung tissues with scarring, inflammation, and fluid.3 That thickening eventually makes it difficult for the blood to absorb oxygen, causing symptoms of ILD.
Idiopathic pulmonary fibrosis is the most common type of interstitial lung disease, accounting for 20% of all the cases.4
Some ILD disorders are:
- Interstitial pneumonia: This is a lung infection affecting the interstitium.
- Chronic silicosis: A lung disease related to occupation and caused by breathing too much silica dust.
- Idiopathic pulmonary fibrosis: Chronic scarring of the interstitium of an unknown cause.
- Nonspecific interstitial pneumonitis: This ILD disorder is caused by an autoimmune disease and leads to damage of the interstitium.
- Connective tissue-related pulmonary fibrosis: Also caused by autoimmune diseases and connective tissue conditions, this type of ILD leads to inflammation and/or scarring of the lungs.
- Hypersensitivity pneumonitis: This type of ILD is caused by inhalation of allergens or other harmful substances, such as mold.
- Sarcoidosis: This inflammatory ILD condition of the interstitium causes swollen lymph nodes and granuloma throughout the body, most often In the heart, eyes, joints, skin, and/or nerves.
- Asbestosis: This ILD condition can be caused by exposure to asbestos and leads to scar tissue on the lungs and inflammation of the lungs.
- Familial pulmonary fibrosis: This is a type of ILD that causes scar tissue buildup in the lungs. It is known for affecting two or more members of a family.
- Desquamative interstitial pneumonitis: This ILD disorder causes lung inflammation and is more common in people who smoke.5
Interstitial Lung Disease Symptoms
People with interstitial lung disease cannot get enough oxygen in their blood. As a result, they experience shortness of breath, especially with activity. As the condition worsens, ILD will affect the ability to breathe, even with rest.6
Additional symptoms may include:
- A dry, unproductive cough
- Extreme fatigue and weakness
- Loss of appetite and weight loss
- Mild chest pain
- Labored breathing—an increased effort to breathe
- Bleeding in the lungs, which can cause shortness of breath, chest tightness, and coughing up blood
Symptoms of interstitial lung disease may get worse with time. You should see your healthcare provider if you experience trouble breathing. Once a diagnosis is made, treatments can help manage inflammation and scarring.
Causes
The causes of interstitial lung disease fall into five broad categories.
These are:7
- Exposure or occupation-related, such as asbestosis and hypersensitivity pneumonitis
- Treatment-related ILD, such as from chemotherapy
- Autoimmune diseases and other connective tissues diseases including rheumatoid arthritis or lupus
- Genetics—some interstitial lung diseases are passed down among families
- Idiopathic ILD is a grouping for those types that have no known cause.
Smoking is a major risk factor for interstitial lung disease. In fact, according to the American Lung Association, smoking can also make ILD worse when it is caused by another condition.6
Diagnosis
To make a diagnosis of interstitial lung disease, your healthcare provider will start with a health history and physical examination. Your practitioner will also request a variety of tests to measure pulmonary function. Testing may include:
Spirometry: This test uses a spirometer device to check lung function. Your healthcare provider will want to see how well you breathe in and out and how easily and quickly you blow air of your lungs.8 This test is simple and can help your practitioner assess how well your lungs are functioning, look for lung disease, determine the severity of the disease, and check for decreased or restricted airflow.
Imaging: A chest X-ray or computed tomography (CT) scan can help take a better look at the lungs. CT scans are more detailed than X-rays.
Bloodwork: An arterial blood draw may be done to look for amounts of carbon dioxide and oxygen in the blood. Other blood work, such as the metabolic profile, complete blood count (CBC), or antibody tests, can check for overall health and signs of infection.5
Bronchoscopy: Using a flexible tube called a bronchoscope, a clinician directly exams the main airways of the lungs (the bronchi). A bronchoscopy can evaluate lung problems, look for blockages, treat any problems, and remove samples of tissue and fluid for further testing.5 The bronchoscopy may include bronchoalveolar lavage, a biopsy, or both.
Lung biopsy: This test takes a tissue sample from the lung to be checked under a microscope and look for signs of ILD conditions, including scarred tissue and inflammation.
Bronchoalveolar lavage: This test removes fluids from the lower part of the respiratory tract to look for infection and rule out or determine causes. This test is often done if your healthcare provider suspects bleeding in the lungs.5
Treatment
Treatment for interstitial lung disease depends on the type and severity. Often, it focuses on relieving symptoms, slowing down disease progression, and improving a person’s quality of life.5
Treatment for ILD may include:
Pulmonary rehabilitation: Most healthcare providers recommend pulmonary rehabilitation for ILD to strengthen the lungs, stretch lung capacity, and help make breathing easier. One study reported in 2017 looked at the effectiveness of pulmonary rehabilitation for people with ILD.9 The researchers determined that pulmonary rehab was effective for many people with ILD regardless of severity and cause. In fact, the therapy was beneficial for increasing exercise tolerance, managing symptoms, and improving quality of life. Pulmonary rehabilitation may include a variety of activities, including physical exercise, breathing techniques to improve lung function, emotional support, and nutritional counseling.
Supplemental oxygen: Oxygen therapy can be prescribed to improve breathing and the ability to be active. Supplemental oxygen can be delivered to match normal levels of oxygen saturation.9
Anti-inflammatory drugs: Some anti-inflammatory drugs can damage the lungs, but there are ones that can help relieve ILD symptoms.10 Corticosteroid drugs, such as prednisone, are considered anti-inflammatory drugs and can be helpful for managing ILD.
Immune-suppressing drugs: If an autoimmune disease is the source of ILD, your healthcare provider may prescribe immune-suppressing medications to help with reducing damage to the lungs and progression of ILD.5
Antifibrosis medicines: These medications are newer drugs that are believed to block pathways in the body that cause scar tissue to form.11 The two most commonly prescribed antifibrosis medications for ILD are Ofev (nintedanib) and Esbriet (pirfenidone), both of which continue to be studied to determine their effectiveness.
Lung transplant: A lung transplant is an option for people with progressive and advanced disease that has not responded to other treatments.11 You will need to be in good health and not have other serious conditions to qualify for a lung transplant.
Your healthcare provider is in the position to determine the best treatment for you with your unique health situation.
Complications
Left untreated, interstitial lung disease can become severe and lead to life-threatening complications. This may include:
Respiratory failure: This is seen in late-stage, longstanding ILD. Respiratory failure is the result of your lungs are failing to pass oxygen to the bloodstream and remove carbon dioxide.
Pulmonary hypertension: Scar tissue, inflammation, and low oxygen levels can restrict blood flow and eventually result in high blood pressure in the arteries of the lungs.
Right ventricle heart failure (cor pulmonale): Interstitial lung disease can lead to changes in the structure and function of the right ventricle.12 These changes may cause the right ventricle to pump harder to get the blood moving through the lungs. Overexertion and strain can cause the ventricle to fail.