Authors: Isaak Quast1 and David Tarlinton1,∗
Immunological memory is a mechanism to protect us against reinfection. Antibodies produced by B cells are integral to this defense strategy and underlie virtually all vaccine success. Here, we explain how B cell memory is generated by infection and vaccination, what influences its efficacy and its persistence, and how characterizing these parameters in the immune response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will help achieve protective immunity through vaccination.
Basic concepts of immunological memory
Creating a memory requires an event to change the status quo in a way that persists beyond the event itself. For the immune system, events that induce memory include infections with viruses and bacteria as well as vaccinations. These challenges trigger immune responses that can leave a footprint of their occurrence that can then persist for decades. Spread over the many years of our lives, we will encounter many infectious threats—some once and others multiple times. But if the first encounter created an immunologically protective state that persists, these repeat exposures can pass essentially unnoticed, producing no or very mild symptoms of infection. During the first (or primary) response, our immune system “learns” how to neutralize the invading organism, and this knowledge is retained as immunological memory, providing ongoing protection from the pathogen; this is immunity. Immunity can exist as a shield, functioning to block infection at the outset, or it can be reactive, triggered into rapid action by re-exposure to a pathogen that has avoided or overwhelmed the shield. However, having immune memory to a pathogen does not necessarily mean having immunity to reinfection; sometimes, immune responses are directed at irrelevant targets on the pathogen, and sometimes, the protective components of the immune memory can diminish to a point of non-functionality. Knowing if and for how long memory confers immunity and the requirements for generating and sustaining such memory, be that from infection or vaccination, are challenging but critical questions to be answered in understanding how to prevent infection.
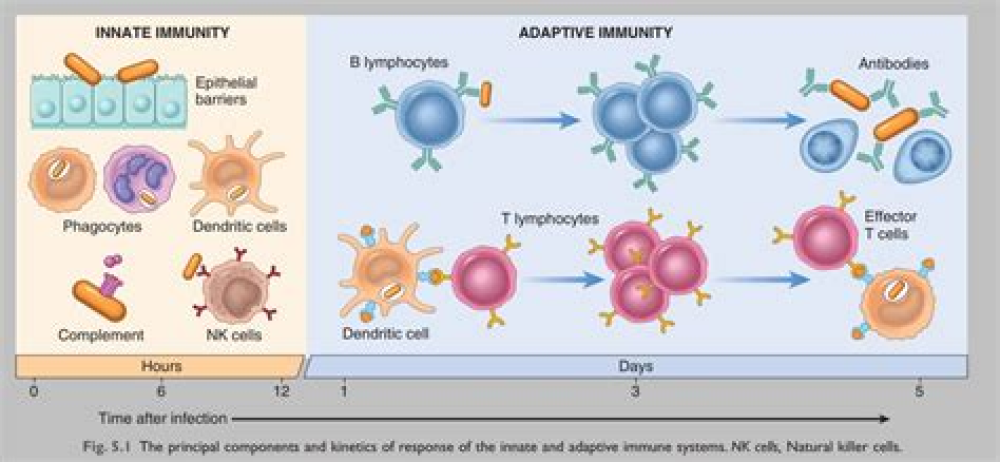
Memory is a cardinal feature of so-called adaptive immune responses, which are those involving lymphocytes, key cells of the immune system. When an infection triggers a lymphocyte response, it induces a small number of pre-existing B and T cells (two types of lymphocytes) to proliferate, creating a small army of cells specific for, and thus able to combat, the infectious agent. B and T cells are triggered to respond by recognizing a part of the pathogen through their antigen receptors with a certain strength. Each B cell and T cell expresses on their surface an antigen receptor that is different to all others such that all possible invaders have their own, pre-existing, matching B and T cells ready to respond if and when required. During the response, some pathogen-specific B cells are induced to differentiate and secrete their antigen receptors into the blood in form of antibodies (Abs), which circulate through the body, binding to the pathogen that triggered the response wherever it occurs. Once the pathogen has been subdued and the response is effectively over, most pathogen-specific B and T cells die, but a small number of these recent combatants—B cells, T cells, and Ab-secreting plasma cells (PCs)—persist as specialized, long-lived immune memory cells.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7826135/