Authors: Baher Al Abbasi 1, Pedro Torres 1, Fergie Ramos-Tuarez 2, Nakeya Dewaswala 1, Ahmed Abdallah 1, Kai Chen 1, Mohamed Abdul Qader 1, Riya Job 1, Samar Aboulenain 1, Karolina Dziadkowiec 1, Huzefa Bhopalwala 3, Jesus E Pino 2, Robert D Chait 2
Abstract
Background: The number of fatalities due to coronavirus disease 2019 (COVID-19) is escalating with more than 800,000 deaths globally. The scientific community remains in urgent need of prognostic tools to determine the probability of survival in patients with COVID-19 and to determine the need for hospitalization.
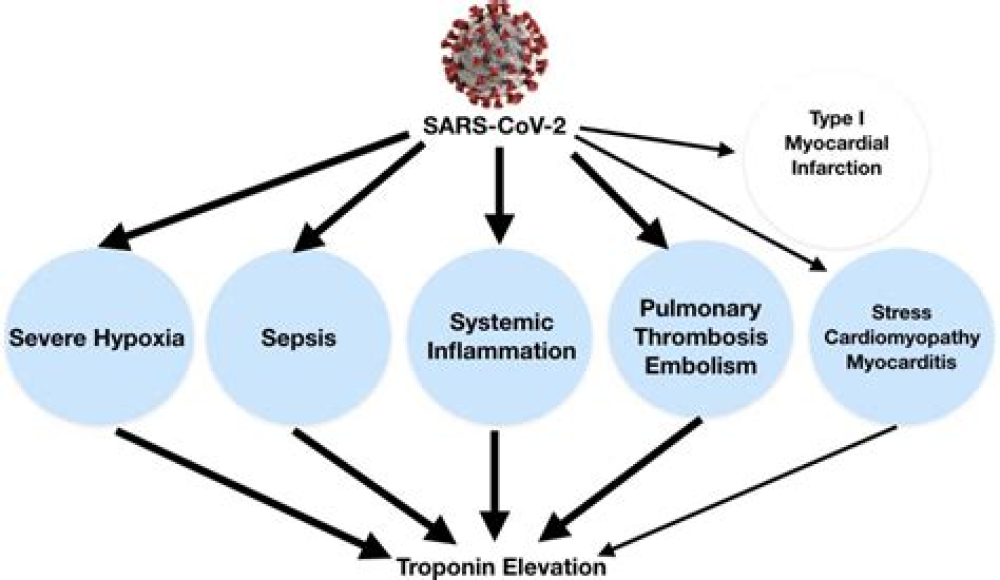
Methods: This is a retrospective cohort study of patients with a diagnosis of COVID-19 admitted to a tertiary center between March 2020 and July 2020. Patients age 18 years and older were stratified into two groups based on their troponin-I level in the first 24 h of admission (groups: elevated vs. normal). The aim of the study is to explore the utility of cardiac troponin-I level for early prognostication of patients with COVID-19.
Results: This cohort of 257 patients included 122/257 (47%) women with a mean age of 63 ± 17 years. Patients with an elevated troponin-I level were more likely to be older (77 ± 13 vs. 58 ± 16 years, P < 0.0001), have a history of hypertension (P < 0.0001), diabetes mellitus (P = 0.0019), atrial fibrillation or flutter (P = 0.0009), coronary artery disease (P < 0.0001), and chronic heart failure (P = 0.0011). Patients with an elevated troponin-I level in the first 24 h of admission were more likely to have higher in-hospital mortality (52% vs. 10%, P < 0.0001). Troponin-I level in the first 24 h of admission had a negative predictive value of 89.7% and a positive predictive value of 51.9% for all-cause in-hospital mortality.
Conclusions: Troponin-I elevation is commonly seen in patients with COVID-19 and is significantly associated with fatal outcomes. However, a normal troponin-I level in the first 24 h of admission had a high negative predictive value for all-cause in-hospital mortality, thereby predicting favorable survival at the time of discharge.
For More Information: https://pubmed.ncbi.nlm.nih.gov/33224386/