- Authors: Joram Huckriede, Sara Bülow Anderberg, Albert Morales, Femke de Vries, Michael Hultström, Anders Bergqvist, José T. Ortiz-Pérez, Jan Willem Sels, Kanin Wichapong, Miklos Lipcsey, Marcel van de Poll, Anders Larsson, Tomas Luther, Chris Reutelingsperger, Pablo Garcia de Frutos, Robert Frithiof & Gerry A. F. Nicolaes Scientific Reports volume 11, Article number: 15701 (2021) Cite this article
Abstract
Coronavirus disease 19 (COVID-19) presents with disease severities of varying degree. In its most severe form, infection may lead to respiratory failure and multi-organ dysfunction. Here we study the levels and evolution of the damage associated molecular patterns (DAMPS) cell free DNA (cfDNA), extracellular histone H3 (H3) and neutrophil elastase (NE), and the immune modulators GAS6 and AXL in relation to clinical parameters, ICU scoring systems and mortality in patients (n = 100) with severe COVID-19. cfDNA, H3, NE, GAS6 and AXL were increased in COVID-19 patients compared to controls. These measures associated with occurrence of clinical events and intensive care unit acquired weakness (ICUAW). cfDNA and GAS6 decreased in time in patients surviving to 30 days post ICU admission. A decrease of 27.2 ng/mL cfDNA during ICU stay associated with patient survival, whereas levels of GAS6 decreasing more than 4.0 ng/mL associated with survival. The presence of H3 in plasma was a common feature of COVID-19 patients, detected in 38% of the patients at ICU admission. NETosis markers cfDNA, H3 and NE correlated well with parameters of tissue damage and neutrophil counts. Furthermore, cfDNA correlated with lowest p/f ratio and a lowering in cfDNA was observed in patients with ventilator-free days.
Introduction
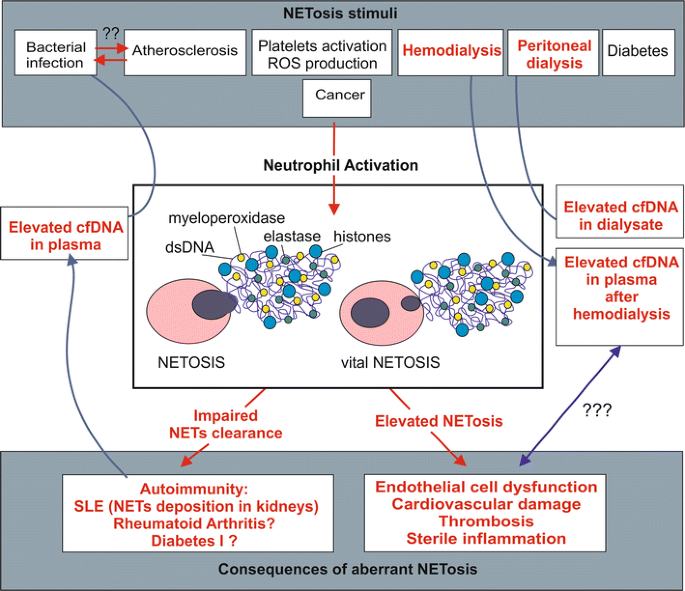
In severe cases, COVID-19 disease develops into acute respiratory distress syndrome (ARDS), an acute lung injury causing patients to be dependent of ventilator support, which may be accompanied by development of multiple organ failure (MOF)1. Mortality is seen primarily in patients over the age of 652,3,4,5 and is highest for infected individuals with underlying comorbidities such as hypertension, cardiovascular disease or diabetes6,7,8. For patients who are taken into the intensive care unit (ICU), a high SOFA (sequential organ failure assessment) score and increased levels of fibrin D-dimers have been reported9 to associate with poor prognosis. Thromboembolic complications develop in 35–45% of COVID-19 patients10, including thrombotic microangiopathies and disseminated intravascular coagulation (DIC) reminiscent of bacterial sepsis. Yet, COVID-19 has distinct features11 that point at a somewhat different pathological mechanism. The involvement of immune regulatory and hemostatic pathways appears evident, and recent findings have confirmed that the innate immune system and more in particular neutrophil extracellular traps (NETs) play a role in COVID-19 disease pathogenesis. NETs, networks of DNA fibers that are decorated with proteins such as histones and elastase, are released from neutrophils to bind and neutralize viral proteins, bacteria and fungi12. While extracellular histones and NE serve a protective, antimicrobial function, they are potentially harmful to the host.
NETs are abundant in lung capillaries13 and are known to be pro-coagulant due to their intrinsic capacity to activate platelets14.
Excessive NET production, initiated by several pathways that also include complement activation13, results in collateral damage to lung tissues, a disturbed microcirculation of the lung15, loss of alveolar-capillary barrier function and further release of pro-inflammatory cytokines16.
During the preparation of this work it was reported that cellular components that are released upon cellular disruption, so-called damage associated molecular patterns (DAMPs) and NETosis are involved in COVID-19 disease1718. This is fully in line with the observation that in ARDS, NETs contribute to disease progress19. Extracellular histones are cytotoxic DAMPs irrespective of their origin. They may appear during NETosis12,14,20 or originate from damaged tissues21, while cell free DNA (cfDNA) and the protease neutrophil elastase (NE) are released concomitantly22. Cellular free deoxyribonucleic acid (cfDNA) and histones promote proinflammatory cytokine release23,24. Histones have been shown to activate and recruit leukocytes25, damage alveolar macrophages26, activate erythrocytes27, epithelial and endothelial cells, in particular pulmonary endothelial cells28,29,30. If not cleared from circulation, cfDNA as well as histones facilitate severe systemic inflammation and worsen the clinical condition31,32. Presence of NE in plasma is associated with exacerbations, lung function decline and disease severity in patients with chronic obstructive pulmonary disease (COPD), bronchiectasis and cystic fibrosis33,34,35 and decrease of NE levels in bronchiectasis patients improved lung function and airway inflammation36.
At the same time that it provides a first line of defense against infections, the innate immune system initiates self-control responses to prevent damage to the host. One mechanism involved in early immunomodulation is the growth arrest-specific 6 (GAS6)/TAM ligand/receptor system37,38. The GAS6/AXL axis regulates the immune response by modulating cytokine production, inducing a reparative cellular response and by mediating efferocytosis, removing irreversibly damaged cells. The system also provides a mechanism of regulating endothelial and platelet activation and interaction39. Plasma concentrations of GAS6 and AXL increase in a diverse spectrum of inflammatory conditions40, including sepsis and septic shock; but also systemic inflammatory response syndrome (SIRS) without infection41. In several studies, GAS6 at IC admission correlated with severity of organ damage (i.e. SOFA) or with damage of specific organs41,42,43,44,45. This is also the case in viral infections46. These studies illustrate the modulatory role of the innate response provided by GAS6 and suggest that the presence of these components in plasma could be an early event in the orchestration of the immune response to viral infections.
cfDNA, extracellular histones and GAS6 are implicated in regulation of inflammatory and hemostatic pathways in the context of severe viral infections and ARDS, all of which are implicated in COVID-19. While other studies have reported the presence of DAMPs and NETosis markers in smaller COVID-19 populations, here we study a group of 100 severely ill COVID-19 patients admitted to the intensive care unit (ICU). Our hypothesis was twofold:
First, cfDNA, NE, histones and GAS6/AXL are activated in severe COVID-19. Second, cfDNA, NE, histones and GAS6/AXL are related to the severity of illness and reflect organ dysfunction in severe COVID-19.
For More Information: https://www.nature.com/articles/s41598-021-95209-x