- Authors:Rajesh Kumar1, Jathinder Kumar1, Caroline Daly and Sadat Ali Edroos http://orcid.org/0000-0002-3267-63502
Abstract
The COVID-19 pandemic is a highly contagious viral illness which conventionally manifests primarily with respiratory symptoms. We report a case whose first manifestation of COVID-19 was pericarditis, in the absence of respiratory symptoms, without any serious complications. Cardiac involvement in various forms is possible in COVID-19. We present a case where pericarditis, in the absence of the classic COVID-19 signs or symptoms, is the only evident manifestation of the disease. This case highlights an atypical presentation of COVID-19 and the need for a high index of suspicion to allow early diagnosis and limit spread by isolation.
This article is made freely available for use in accordance with BMJ’s website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.https://bmj.com/coronavirus/usage
http://dx.doi.org/10.1136/bcr-2020-237617
Background
The global COVID-19 pandemic is caused by severe acute respiratory syndrome coronavirus 2, an enveloped single-stranded RNA virus of zoonotic origin. Transmission is mainly by aerosolised droplet contact, although surface fomite contact and faecal transmission are reported. Symptoms of coronavirus include high-grade fever, severe cough and breathlessness. Cytokine induction causes heavy neutrophilia in the alveoli, with capillaritis, fibrin deposition and thick mucositis causing respiratory failure, acute lung injury and death. Conversely approximately one in eight patients are estimated to have an entirely benign course, transmitting the virus with no clinical manifestation of the disease.1 2 Chest pain in COVID-19 may have cardiac causes, including acute coronary syndrome, pericarditis and myocarditis.3 We present the first described case of acute pericarditis in the absence of initial respiratory symptoms secondary to COVID-19.
Case presentation
A 66-year-old farmer was admitted with 1-day history of acute-onset severe pleuritic chest pain, with four episodes lasting 10–15 min. The pain was worse when lying flat and relieved by leaning forward. He had no sweating nor fever. His history includes Crohn’s disease, hypertension and benign prostatic hyperplasia. His medications were esomeprazole, ramipril and tamsulosin. He had a 40 pack-year smoking history and a significant familial premature coronary disease. His vaccination schedule was up to date, and he had not travelled recently. On examination his temperature was 36.9°C, blood pressure was 134/83 mm Hg, heart rate was 86 beats/min, respiratory rate was 16 breaths/min and an O2 saturation of 99% on ambient air. His general, cardiovascular and respiratory examinations were normal.
Investigations
Full blood count, urea and electrolytes, coagulation profile, and liver function tests were normal. His C reactive protein (CRP) was 7 mg/L (normal <5 mg/L). High sensitivity cardiac troponin T (hs-cTnT) on admission and at 6 hours were 10 ng/L and 13 ng/L, respectively (normal <14 ng/L). His ECG showed ST segment elevation in most leads with PR interval depression, and his chest X-ray (CXR) confirmed clear lungs with no abnormality (figure 1). Transthoracic echocardiogram (TTE) confirmed normal structure and function, although his pericardium was echo bright with no pericardial effusion (figure 2). CT of the thorax, abdomen and pelvis was normal.

Figure 1
Admission ECG and chest X-ray on day 1. There is minimal ST segment elevation in most leads with PR interval depression.

Figure 2
Transthoracic echocardiogram showing brightened pericardium (white arrows) with no effusion.
Serum, nasopharyngeal and oropharyngeal swab specimen samples were sent for aetiological viruses associated with pericarditis. However, the patient presented in February 2020, which was early in the chronology of COVID-19 in Ireland and he did not have routine COVID-19 screening swabs. Complement levels, erythrocyte sedimentation rate and connective tissue screens were negative. Nucleic acid amplification tests for influenza A and B were negative. Cardiac MRI (cMRI) with adenosine stress perfusion showed a structurally normal heart with no effusion, fibrosis, infarction or infiltration. No inducible perfusion defects were evident during adenosine stress. His pericardium appeared mildly thickened (figure 3).

Figure 3
Cardiac MRI of the patient with perfusion showing normal left ventricle muscle (black arrows). The pericardium, pointed by white arrows, shows mild thickening (bold white) with no effusion.
Differential diagnosis
Differential diagnoses included myocarditis, acute coronary syndrome, pericarditis or pleuritis.
Treatment
A diagnosis of pericarditis was made based on typical chest pain, ECG presentation and TTE. He was started on oral colchicine two times per day for 2 weeks and was discharged on day 4.
Outcome and follow-up
The patient was readmitted on day 6 with recurrence of intermittent pleuritic chest pain and dry cough. Vital signs, physical examination and blood tests were normal. CXR and ECG remained unchanged. Viral serology was negative for routine viruses associated with pericarditis. A COVID-19 viral PCR nasopharyngeal swab was positive.
The public health team was notified and the patient was isolated. On day 8 he developed upper respiratory tract symptoms with peak temperature of 38.7°C. Lymphopaenia (0.3×109, normal >1×109/L) with normal interleukin-6 (5.77, normal 0.09–7.26 pg/mL), CRP and hs-cTnT were seen. Blood culture showed no growth, and serial CXR remained normal. He recovered with symptomatic treatment and oral colchicines and was discharged on day 12.
Discussion
COVID-19 has numerous adverse effects on the cardiovascular system. Cardiac injury with troponin leak is associated with increased mortality in COVID-19, and its clinical and radiographic features are difficult to distinguish from those of heart failure.4–6 One reported COVID-19 case with upper respiratory tract symptoms had haemorrhagic pericardial effusion with tamponade.7 To our knowledge this is the first case where COVID-19 presents as pericarditis, in the absence of evident respiratory or myocardial involvement.
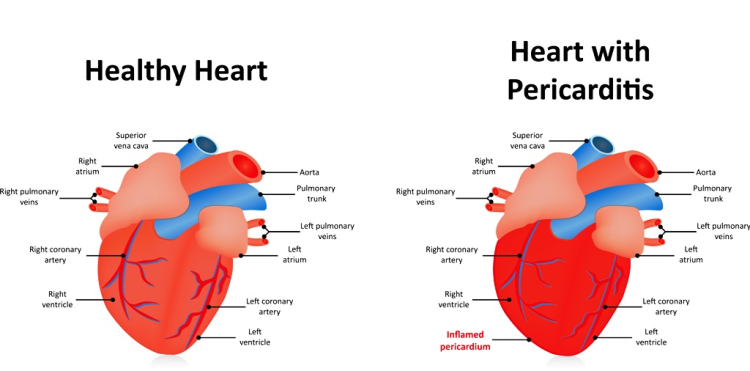
Acute pericarditis is the most common disease of the pericardium and is responsible for 0.2% of chest pain-related hospitalisations. Conversely 40%–85% of pericarditis cases are of unknown aetiology, probably due to difficulty in obtaining diagnostic pericardial samples. It is commonly seen in viral infections, including coxsackie, enterovirus, herpes simplex, cytomegalovirus, H1N1, respiratory syncytial virus, parvovirus B19, influenza, varicella, HIV, rubella, echovirus, and hepatitis B and C, although the viruses responsible in a given patient may be different genotypes of the same virus or different coexistent viruses.8 9
In this patient respiratory swabs were initially negative, and viraemia first manifested with dry pericarditic symptoms, with a later diagnosis of COVID-19. Defining the underlying causative virus is not always possible. Serological tests are only suggestive of a diagnosis of pericarditis and may yield false negative results. Pericardial inflammation may prompt symptoms, yet may precede the generation of an observable pericardial effusion. TTE is recommended to exclude significant effusion, although the absence of fluid does not rule out active pericarditis. cMRI can describe pericardial thickening or small effusions, which are not appreciated on TTE, assess for myocarditis on T2-weighted imaging, define pericardial inflammation on late gadolinium phase and quantify systolic function.10 Pericardiocentesis is the gold standard for definition of the underlying cause, providing a sufficient depth of fluid at a favourable angle is seen on TTE, although this carries associated risk of serious cardiac injury and a clinical diagnosis may be made if other supportive features are present.
Acute pericarditis is usually self-limiting, although it recurs in up to 30% of cases. Most patients recover in 2–4 weeks with supportive measures, which would conventionally include non-steroidal anti-inflammatory drugs (NSAIDs), colchicines and treating the causative disease. Applying this to a patient with COVID-19 requires balancing this conventional approach with an emerging understanding of pharmacotherapy in COVID-19. Colchicine inhibits microtubule, cell adhesion molecule and inflammasome activity, and is of use in preventing relapse in pericarditis at first presentation.11 It is being trialled as a potential therapeutic anticytokine agent in COVID-19 in Italy, with one report of its use being associated with improvement.12 Conversely the use of NSAIDs in COVID-19 may be harmful, with previously recognised increased risks of stroke and myocardial infarction (MI) with NSAIDs in acute respiratory infections raising concerns. No effective respiratory benefit has been seen with glucocorticoid use in COVID-19, although their use in pericarditis may promote relapse.13 14
Currently, our understanding of the transmission dynamics and the spectrum of clinical illness of COVID-19 is limited. Cardiac involvement with various ECG presentations is possible and clinicians all across the globe need to be aware of this possibility. This case highlights the importance of recognising COVID-19 infection with atypical clinical presentations such as pericarditis and non-specific ECG changes, and coordination with healthcare team regarding prompt isolation to decrease the risk of transmission of the virus and if any need of early hospitalisation. This case report is helpful in treating patients with this unique clinical presentation.
Patient’s perspective
I woke up one day and I had a nagging pain in the center of my chest, which I never had or felt before, sharp like a knife and pressure on top of it as well. It was a constant nagging pain. It was relieving when I was sitting forward and back worsened as I was lying down in the bed. I felt more weak that day and had no energy. Then pain got a bit worse at midday and my wife advised me to visit my doctor -general practitioner as a felt weak. After my doctor saw me, he advised me to go to the hospital and get myself check out to make sure I am not having a heart attack. I and my wife got very nervous. We came urgent to hospital emergency where a nurse examined me first, followed by a doctor and suggested they don’t think that I am having a heart attack. He referred me to heart expert, who suggested that I have to be admitted in the hospital for more tests. They kept me for three days and all my tests like chest and body scans and bloods suggested that I have inflammation around the layers of heart. I was given some medication and discharged home that it will get better in a few days. I went home, the pain was there, it didn’t went completely but improved slightly. It was worse with lying down in the bed. It wasn’t going away despite me doing all what I was told for next few days. I came back to emergency department in 1st march as the pain wasn’t settling at all with the medication. I went through all this process again. I was isolated, swabbed my nose for this new virus-COVID-19. I did not had any sick contact or any other viral contact. I was nervous, and the result came positive. I was kept in separate part of hospital with no direct visitors to me and my family called me on the phone. I thought I am going to die but all the doctors and nurses reassured me. I developed slight cough and flu like illness for 2 days and then I got better next few days and I came home. I was told to follow strict isolation and precautions. No issues since discharge feeling very well. It’s an unpleasant experience to be part of virus and I thought I won’t make it as there was uncertainty about future events. I am greatly thankful to all the team who were involved in my care.
Learning points
- Pericarditis is a potential presentation of COVID-19.
- COVID-19 can have an atypical presentation with non-respiratory symptoms.
- Recognition of an atypical symptom of COVID-19 allows for early isolation and limits the spread.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.doi:10.1016/S0140-6736(20)30183-5pmid:http://www.ncbi.nlm.nih.gov/pubmed/31986264CrossRefPubMedGoogle Scholar
- Zhu J, Ji P, Pang J, et al. Clinical characteristics of 3062 COVID‐19 patients: a meta‐analysis. J Med Virol 2020;54. doi:doi:10.1002/jmv.25884. [Epub ahead of print: 15 Apr 2020].Google Scholar
- Hu H, Ma F, Wei X, et al. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J 2020. doi:doi:10.1093/eurheartj/ehaa190. [Epub ahead of print: 16 Mar 2020].pmid:http://www.ncbi.nlm.nih.gov/pubmed/32176300Google Scholar
- Han Y. Initial COVID-19 affecting cardiac patients in China. Eur Heart J 2020;41:1719. doi:10.1093/eurheartj/ehaa257pmid:http://www.ncbi.nlm.nih.gov/pubmed/32232395PubMedGoogle Scholar
- Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020. doi:doi:10.1001/jamacardio.2020.1096. [Epub ahead of print: 27 Mar 2020].pmid:http://www.ncbi.nlm.nih.gov/pubmed/32219357Google Scholar
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020. doi:doi:10.1001/jamacardio.2020.0950. [Epub ahead of print: 25 Mar 2020].pmid:http://www.ncbi.nlm.nih.gov/pubmed/32211816Google Scholar
- Dabbagh MF, Aurora L, D’Souza P, et al. Cardiac tamponade secondary to COVID-19. JACC Case Rep 2020;2:1326–30.doi:10.1016/j.jaccas.2020.04.009 pmid:http://www.ncbi.nlm.nih.gov/pubmed /32328588PubMedGoogle Scholar
- Fancello L, Monteil S, Popgeorgiev N, et al. Viral communities associated with human pericardial fluids in idiopathic pericarditis. PLoS One 2014;9:e93367. doi:10.1371/journal.pone.0093367 pmid:http://www.ncbi.nlm.nih.gov/pubmed/24690743CrossRefPubMedGoogle Scholar
- Kytö V, Sipilä J, Rautava P. Clinical profile and influences on outcomes in patients hospitalized for acute pericarditis. Circulation 2014;130:1601–6.doi:10.1161/CIRCULATIONAHA.114.010376 pmid:http://www.ncbi.nlm.nih.gov/pubmed/25205801Abstract/FREE Full TextGoogle Scholar
- Koos R, Schröder J, Kühl HP. Acute viral pericarditis without typical electrocardiographic changes assessed by cardiac magnetic resonance imaging. Eur Heart J 2009;30:2844. doi:10.1093/eurheartj/ehp407mid:http://www.ncbi.nlm.nih.gov/pubmed/19825810CrossRefPubMedGoogle Scholar
- Bayes-Genis A, Adler Y, de Luna AB, et al. Colchicine in pericarditis. Eur Heart J 2017;38:1706–9.doi:10.1093/eurheartj/ehx246pmid:http://www.ncbi.nlm.nih.gov/pubmed/30052886PubMedGoogle Scholar
- Gandolfini I, Delsante M, Fiaccadori E, et al. COVID-19 in kidney transplant recipients. Am J Transplant 2020.Google Scholar
- Perricone C, Triggianese P, Bartoloni E, et al. The anti-viral facet of anti-rheumatic drugs: lessons from COVID-19. J Autoimmun 2020;111:102468. doi:10.1016/j.jaut.2020.102468 pmid:http://www.ncbi.nlm.nih.gov/pubmed/32317220PubMedGoogle Scholar
- Zhang W, Zhao Y, Zhang F, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the perspectives of clinical immunologists from China. Clin Immunol 2020;214:108393. doi:10.1016/j.clim.2020.108393 pmid:http://www.ncbi.nlm.nih.gov/pubmed/32222466 CrossRefPubMedGoogle Scholar