Ali Tabatabai 1, Joseph Rabin 2, Jay Menaker 2, Ronson Madathil 3, Samuel Galvagno 4, Ashley Menne 5, Jonathan H Chow 4, Alison Grazioli 6, Daniel Herr 1, Kenichi Tanaka 4, Thomas Scalea 2, Michael Mazzeffi 4Affiliations expand
PMID: 32539272 PMCID: PMC7242090 DOI: 10.1213/XAA.0000000000001236
Abstract
Critically ill patients with coronavirus disease 2019 (COVID-19) have been observed to be hypercoagulable, but the mechanisms for this remain poorly described. Factor VIII is a procoagulant factor that increases during inflammation and is cleaved by activated protein C. To our knowledge, there is only 1 prior study of factor VIII and functional protein C activity in critically ill patients with COVID-19. Here, we present a case series of 10 critically ill patients with COVID-19 who had severe elevations in factor VIII activity and low normal functional protein C activity, which may have contributed to hypercoagulability.
The novel coronavirus, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has caused a global pandemic accounting for over 190,000 deaths as of April 24, 2020. In hospitalized patients, mortality is reported to be approximately 25%, and in critically ill patients, who require mechanical lung ventilation mortality is between 65% and 85%.1–3 Most patients who die progress to septic shock and half develop coagulopathy with progressively increasing D-dimer.1 Age, coronary artery disease, and elevated D-dimer are independent predictors of mortality.1
Several reports suggest that SARS-CoV-2 infection is associated with coagulation derangements, particularly hypercoagulability, and that anticoagulation with heparin may improve survival.4–6 In our own experience, we have noted marked hypercoagulability in critically ill patients with coronavirus disease 2019 (COVID-19), including thrombosis of renal replacement therapy filters and extracorporeal membrane oxygenation (ECMO) circuits.
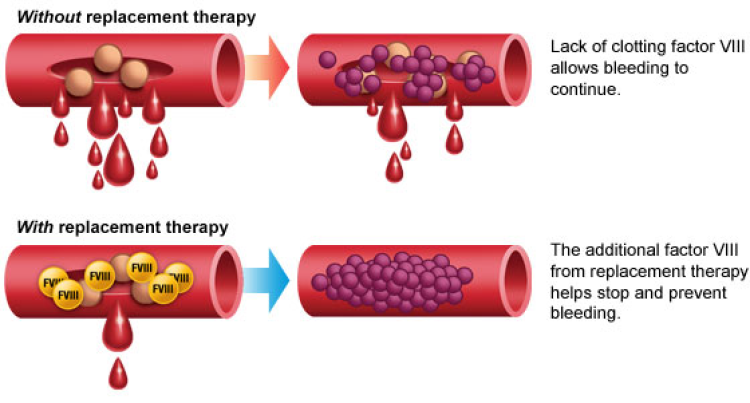
Factor (F) VIII is a procoagulant factor that is stored in endothelial cells and is released during inflammation. It has a critical role in coagulation, because it is a cofactor in the tenase complex, which converts factor X into activated factor X. Protein C is an endogenous anticoagulant protein that, when activated, cleaves FVIII into its inactive form. When FVIII overwhelms activated protein C, prolonged thrombin generation can occur leading to hypercoagulability. To our knowledge, there have been no studies of FVIII activity and functional protein C activity in patients with COVID-19 in the United States. We describe a case series of 10 critically ill patients with COVID-19 who had both FVIII and functional protein C activity measured during their clinical course. The University of Maryland, Baltimore institutional review board approved the case review and exempted the study from written informed consent.
CASE DESCRIPTIONS
Methods
Critically ill adult patients with COVID-19 who were on mechanical lung ventilation in the R Adams Cowley Shock Trauma Center bio-containment unit between April 1, 2020 and April 5, 2020 and had FVIII and functional protein C activity measured were included. FVIII activity and functional protein C activity were measured as part of a comprehensive coagulation evaluation in patients who had clinical evidence of hypercoagulability, including thrombosis in central and peripheral access lines, purpuric skin changes, and elevated D-dimer concentration. All patients had the following coagulation factor and inflammatory markers measured: FVIII activity, functional protein C activity, fibrinogen, antithrombin activity, C-reactive protein, and ferritin. Patients also had standard plasma-based coagulation tests and complete blood counts performed.
Continuous patient variables were summarized as the mean value ± standard deviation, and categorical patient variables were summarized as the number and percentage of patients. Coagulation factor and inflammatory marker concentrations were summarized as the mean value ± standard deviation or median value and interquartile range, depending on whether data were normally distributed or skewed. Normality was checked with the Shapiro-Wilk test. The relationships between age and coagulation factor concentrations were explored using scatterplots with fitted Loess curves. A 95% confidence band was added to Loess curves. Statistical analysis was performed using SAS 9.3 (SAS Corporation, Cary, NC).Go to:
RESULTS
Ten critically ill patients were included in the case series (Table (Table1).1). All patients were on mechanical lung ventilation with acute respiratory distress syndrome (ARDS) related to SARS-CoV-2 infection. The mean number of mechanical lung ventilation days was 9 ± 6 at the time of patients’ coagulation evaluation. Diabetes mellitus was the most common comorbidity, occurring in 70% of patients. Eighty percent of patients were men and 70% had type O blood.
Table 1.
Patient Characteristics
| Variable | Mean ± SD, or n (%) |
|---|---|
| Age (y) | 53 ± 16 |
| Male sex | 8 (80) |
| Body mass index (kg/m2) | 33 ± 8 |
| Diabetes mellitus | 7 (70) |
| Chronic arterial hypertension | 4 (40) |
| Chronic kidney disease | 2 (20) |
| Peripheral vascular disease | 1 (10) |
| Cerebral vascular disease | 1 (10) |
| Chronic obstructive pulmonary disease or asthma | 0 (0) |
| Coronary artery disease | 1 (10) |
| Dyslipidemia | 3 (30) |
| Blood type | |
| O | 7 (70) |
| A | 2 (20) |
| B | 1 (10) |
| AB | 0 (0) |
| Acute respiratory distress syndrome | |
| Severity | |
| Mild | 4 (40) |
| Moderate | 3 (30) |
| Severe | 3 (30) |
| Days on mechanical lung ventilation | 9 ± 6 |
| Extracorporeal membrane oxygenation | 2 (20) |
| Acute renal failure requiring renal replacement | 3 (30) |
n = 10.
Abbreviation: SD, standard deviation.
Table Table22 shows coagulation factor and inflammatory marker concentrations. Median prothrombin time and mean activated partial thromboplastin time were normal. Both median fibrinogen concentration and FVIII activity were markedly elevated in patients with COVID-19, while median antithrombin activity and mean functional protein C activity were low normal. Seven of 10 patients had a FVIII activity above the maximum detectable range for the assay, which is 400%. The 3 patients who did not have an FVIII activity above 400% were all less than 50 years old and 2 of them were female. Median D-dimer and ferritin concentration along with mean C-reactive protein concentration were elevated for all patients in the cohort.
Table 2.
Coagulation Factors and Inflammatory Markers
| Variable | Mean ± SD or Median [Q1, Q3] |
|---|---|
| Prothrombin time (normal = 12–15 s) | 15 [14, 15] |
| International normalized ratio | 1.1 [1.1, 1.2] |
| Activated partial thromboplastin timea (normal = 25–38 s) | 30 ± 5 |
| Fibrinogen concentration (mg/dL) (normal = 216–438 mg/dL) | 763 [478, 1092] |
| Factor VIII activityb (normal = 50%–200%) | 400 [369, 400] |
| Functional protein C activity (normal = 83%–168%) | 104 ± 40 |
| Antithrombin activity (normal = 75%–135%) | 84 [70, 90] |
| D-dimerc (normal < 649 ng/mL FEU) | 2820 [2410, 20,000] |
| C-reactive protein (normal < 1 mg/dL) | 17 ± 14 |
| Ferritin concentration (normal = 18–464 ng/mL) | 1343 [748, 2116] |
n = 10.
Abbreviations: FEU, fibrinogen equivalence units; SD, standard deviation.
aExcludes 3 patients who were receiving therapeutic heparin.
bUpper limit of assay is 400% and 7 of 10 patients were at upper limit.
cUpper limit of assay is 20,000 ng/mL FEU and 3 of 10 patients were at upper limit.
Older patients appeared to have higher fibrinogen concentrations and FVIII activity along with lower antithrombin activity and functional protein C activity (Figure). The 1 patient who died in the cohort at the time of our analysis was 82 years old. He had a fibrinogen concentration of 1092 mg/dL, antithrombin activity of 37%, and functional protein C activity of 37%. Among the remaining 9 patients, 7 were extubated, 4 were discharged from the hospital and 2 remained on ECMO at the time of our report. No patient was diagnosed with symptomatic deep venous thrombosis or pulmonary embolism.Figure.
Relationships between age and coagulation factor concentration and activity.Go to:
DISCUSSION
Extensive cross talk occurs between the immune and coagulation systems. Prior studies have shown that interleukin (IL)-6 and other cytokines activate coagulation.7,8 COVID-19 is associated with a profound inflammatory response in many patients that is characterized by high IL-6, fibrinogen, and ferritin concentrations.1 COVID-19 is also associated with high D-dimer, suggesting extensive thrombin generation and fibrinolysis.1 This pattern may reflect hypercoagulability related to severe inflammation.9 Our case series demonstrates that some critically ill patients with COVID-19 in the United States have a coagulation profile characterized by severely elevated fibrinogen concentration and FVIII activity, as well as low normal antithrombin and functional protein C activity. This hypercoagulable pattern appears to be accentuated with age, particularly in men. These findings have similarities with and differences from a recent study by Panigada et al9 where functional protein C activity was normal in most patients and mean FVIII activity was elevated to 297%. Mean fibrinogen concentration in their study was 680 mg/dL compared to 763 mg/dL in our study. The authors did not explore the impact of age on coagulation profile and there were few details provided about the patients’ comorbidities. We postulate that differences between the 2 studies could be related to a higher prevalence of metabolic syndrome and other comorbidities among adults in the United States leading to more severe coagulation abnormalities.
FVIII and fibrinogen are acute phase reactants that increase during infection, pregnancy, and other inflammatory states.10,11 Antithrombin and protein C are endogenous anticoagulant proteins, both of which decrease in men as they age.12 An imbalance in procoagulant and anticoagulant factor concentrations can predispose patients to thrombotic complications and perhaps microthrombosis. Hypercoagulability has been reported in critically ill patients with COVID-19 and there are recent reports of ischemic stroke and limb ischemia.13,14
Some patients with COVID-19 have been found to have antiphospholipid antibodies.13 Our data suggest that an imbalance in the FVIII-protein C system also contributes to hypercoagulability. Given this imbalance, there may be a role for systemic anticoagulation or low-dose thrombolysis in some patients. Although not commercially available in the United States, recombinant thrombomodulin could be a potential treatment for hypercoagulable patients with COVID-19. It has immunomodulatory effects and increases protein C activation in the presence of thrombin.15 There are no high-quality studies to support systemic anticoagulation at this time, but the observational study by Tang et al6 strongly suggests that patients with an elevated D-dimer concentration have better survival when treated with anticoagulation.
The main strength of our case series is that it is the first, to our knowledge, to report FVIII activity and functional protein C activity in critically ill patients with COVID-19 in the United States. An important limitation is that our cohort was comprised overwhelmingly obese men with diabetes mellitus, which may limit generalizability. Also, patients in our study had FVIII and functional protein C activity measured once, not multiple times during their stay.
In summary, in a case series of 10 critically ill patients with COVID-19, who were mostly older men, we found that fibrinogen concentration and FVIII activity were severely elevated, while antithrombin activity and functional protein C activity were low normal. These findings suggest that an imbalance in procoagulant and anticoagulant factor concentrations may contribute to hypercoagulability in some critically ill patients with COVID-19.Go to:
DISCLOSURES
Name: Ali Tabatabai, MD.
Contribution: This author helped conceive the study, review the analysis of the data, write and approve the final manuscript.
Name: Joseph Rabin, MD.
Contribution: This author conceived the study, saw the original data, reviewed the analysis of the data, wrote and approved the final manuscript.
Name: Jay Menaker, MD.
Contribution: This author helped conceive the study, review the analysis of the data, write and approve the final manuscript.
Name: Ronson Madathil, MD.
Contribution: This author helped conceive the study, review the analysis of the data, write and approve the final manuscript.
Name: Samuel Galvagno, DO, PhD.
Contribution: This author helped conceive the study, review the analysis of the data, write and approve the final manuscript.
Name: Ashley Menne, MD.
Contribution: This author helped review the analysis of the data, write and approve the final manuscript.
Name: Jonathan H. Chow.
Contribution: This author helped review the analysis of the data, write and approve the final manuscript.
Name: Alison Grazioli, MD.
Contribution: This author helped review the analysis of the data, write and approve the final manuscript.
Name: Daniel Herr, MD.
Contribution: This author helped review the analysis of the data, write and approve the final manuscript.
Name: Kenichi Tanaka, MD, MSc.
Contribution: This author helped conceive the study, review the analysis of the data, and write and approve the final manuscript.
Name: Thomas Scalea, MD.
Contribution: This author helped review the analysis of the data, write and approve the final manuscript.
Name: Michael Mazzeffi, MD, MPH, MSc.
Contribution: This author conceived the study, saw the original data, reviewed the analysis of the data, wrote and approved the final manuscript.