- Ana Flávia Avelar Maia Seixas, Milena Soriano Marcolino, Felipe Souza Guimarães, et. al.,, BMC Infectious Diseases volume 25, Article number: 509 (2025)
Abstract
Introduction
Long COVID is a condition that occurs in patients with a previous history of COVID-19, and symptoms that cannot be explained by another diagnosis persist.
Objective
To evaluate the prevalence of long COVID and associated factors in patients treated with a public telehealth service during acute COVID-19.
Method
This was a cross-sectional study involving users of a COVID-19 telehealth service offered during the critical phase of the pandemic, called TeleCOVID-MG. Individuals older than 18 years of age who tested positive for SARS-CoV-2 and were monitored during social isolation were eligible. Prevalence was calculated, and descriptive analysis and group comparisons (patients with and without long COVID symptoms) were performed in addition to logistic regression with odds ratios and 95% confidence intervals.
Results
Among the 699 patients included in the study, 60.8% were women aged between 30 and 49 years (44.6%) and had a high school education (46.5%). The main comorbidities were hypertension (20.9%), diabetes (8.3%), and heart disease (3.9%). The incidence of long COVID was 26.8% (95% CI: 23.5; 30.1). Cognitive symptoms (49.7%), chronic diarrhea (49.2%), and cough (40.6%) were the most persistent symptoms. Female sex (OR: 2.51), secondary education (OR: 2.13), elementary education (OR: 2.81), monthly income between 600 and 1,000 USD (OR: 5.85), supplementary health assistance (OR: 1.98), anosmia during acute COVID-19 (OR: 4.52) and need for in-person care (OR: 2.44) were factors associated with a higher incidence of long COVID.
Conclusion
Long COVID affected almost one-third of the study population. Although the COVID-19 pandemic is under control, the virus continues to infect individuals, raising doubts about the long-term complications of the disease.
Introduction
COVID-19 (coronavirus disease 2019) has presented major challenges to the global health system [1]. Considering the rapid spread of COVID-19 to several countries around the world, there was a need to seek alternatives that can treat symptomatic patients in a timely manner due to the overload of the global health system [2]. In this context, telehealth strategies have emerged as a valuable tool to provide remote care, reduce the burden on healthcare facilities, and ensure timely access to medical assistance for symptomatic patients [3].
COVID-19 can no longer be considered a public health emergency; however, post-COVID-19 complications, also known as long COVID continue to generate many uncertainties [4]. According to the World Health Organization (WHO), long COVID is a condition that occurs in patients with a history of probable or confirmed SARS-CoV-2 infection three months after the acute phase of the disease; these symptoms persist for at least two months and cannot be explained by another diagnosis [5, 6]. This condition can develop in patients who have a mild, moderate, or severe form of the disease and can also manifest itself in asymptomatic individuals [7, 8].
Long COVID consequences are being seen as a second pandemic, as they have affected a large number of people [9], which prevalence to 10 to 20% [5, 6]. The most prevalent signs and symptoms of long COVID include changes in memory and concentration; fatigue; dyspnea; myalgia; arthralgia; headache; cough; chest pain; anosmia; ageusia; diarrhea; and alopecia [5, 10,11,12]. Advanced age, female sex, and the number of symptoms related to the disease in the acute phase seem to contribute to a higher prevalence [12], as does smoking, being overweight, and the need for prior hospital admission due to COVID-19. The use of oxygen therapy in the acute phase [10] and the presence of comorbidities, such as heart disease, systemic arterial hypertension, diabetes, and cancer [11], are also associated with a higher incidence of this morbidity.
In the face of the rapid increase in COVID-19 cases and the looming collapse of the public health system, telehealth emerged as a cost-effective tool with significant potential to address the substantial demands posed by the acute phase of the disease [13,14,15]. In the post-pandemic period, a new challenge has arisen, understanding the long-term consequences of COVID-19. However, there remains a scarcity of studies on this topic in Brazil, particularly those focusing on telecare. Thus, this study aimed to evaluate the prevalence of long COVID and identify the factors associated with its occurrence in patients managed through telehealth services.
Method
Study design
This was a cross-sectional study involving users of a telecare and telemonitoring service, which attended individuals with clinical manifestations of COVID-19, named TeleCOVID-MG [15]. Faced with the context of progressive growth in the number of COVID-19 cases and the imminent collapse of the public health system in Minas Gerais state, Brazil, the Telehealth Network of Minas Gerais (Rede de Telessaúde de Minas Gerais—RTMG), which is a large-scale public telehealth service [16, 17] created the TeleCOVID-MG project for remote assistance to patients with symptomatic COVID-19. Briefly, TELECOVID-MG was an on-demand telecare service delivered by a multidisciplinary team, providing consultations during the acute phase of the disease and telemonitoring during the social isolation period, typically spanned 6 to 14 days [15].
Study locations
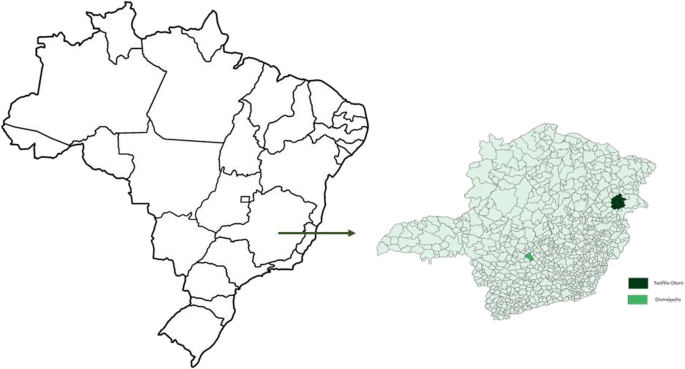
This investigation was carried out with patients from the municipalities of Divinopolis and Teófilo Otoni in the state of Minas Gerais (MG), located in the southeastern region of Brazil, treated with TeleCOVID-MG during the critical phase of the COVID-19 pandemic from June 2020 to February 2021. During the data collection period, none of the participants had received any vaccination for the COVID-19. At the time of the study, Divinópolis had a resident population of 231,091 inhabitants and a human development index (HDI) of 0.764 (ranking 21st in Minas Gerais). Teófilo Otoni, in contrast, had a resident population of 137,418 inhabitants and an HDI of 0.701 (with 223 placed in Minas Gerais) [18] (Fig. 1).
Study population, sample, and data collection
All users in the aforementioned TeleCOVID-MG municipalities who met the following criteria were considered eligible for the study: were aged 18 years or over, had a positive result in diagnostic tests for SARS-CoV-2, had been monitored by a team of TeleCOVID-MG for > 06 days, and had clinical information recorded by the health team in remote care during the acute phase of the disease.
For the sample calculation, the following indicators were used: a finite eligible population of 2,260 individuals served in two cities by the TeleCOVID-MG project with a confirmed diagnosis of COVID-19 from June 2020 to February 2021; an estimated prevalence of 10% of the event in the population [6] a margin of error of 3%; a design effect of 1.0; and a confidence limit of 95%. The sample size necessary to meet these parameters was 626 individuals.
For the data collection, a structured questionnaire was used to collect information confirming the diagnosis of COVID-19, the evolution of the clinical picture, the persistence of signs and symptoms, the type and duration of symptoms, the impact of the persistence of symptoms on activities of daily living and the need for treatment for the patient in the present study.
The conditions possibly related to long COVID included in the interview questionnaire were cough, dyspnea, fatigue, chest pain, thrombosis, systemic arterial hypertension, coronary heart disease, headache, stroke, seizure, neuropathy, weight loss/malnutrition, depression or sadness or hopelessness, anxiety, stress, insomnia, delirium or mental confusion, cognitive symptoms, stabbing pain in the upper or lower limbs, chronic diarrhea, odynophagia, anosmia, ageusia, intermittent low fever, skin rashes, hearing loss problems, alopecia or telogen effluvium, and diabetes mellitus. All complaints were investigated regarding the presence and duration of signs and symptoms. The criterion used for defining long COVID was symptoms persisting for more than 60 days after the acute phase.
The questionnaire used for data collection was tested in a pretest and pilot study. Patients who were monitored by TeleCOVID-MG in the acute phase of the disease were contacted via telephone by a previously trained team consisting of undergraduate medical students supervised by postgraduate students and faculty advisors, reaching the number of patients indicated by the sample calculation. The data were collected in the first half of 2021. There was a maximum of three attempts to contact each patient, varying between weekdays and weekends and at different times (morning, afternoon and night).
Sociodemographic and clinical information, such as sex, age, body mass index (BMI), education, individual income, supplementary health care, smoking status, and the presence of comorbidities, was also collected during acute care. The dollar (USD) rate used to convert the Brazilian minimum wage on the date of collection was that of March 2021 (5.5 USD).
Statistical analysis
The descriptive analysis included frequency distributions as well as measures of central tendency and dispersion, based on the valid number of observations for each variable. The incidence of long COVID was calculated with a 95% confidence interval (CI). Based on the prevalence, two groups of individuals, those with and without long COVID, were formed and compared based on socioeconomic, demographic, and clinical characteristics collected in the acute phase.
To evaluate variables capable of predicting long COVID, logistic regression was used with odds ratios (ORs) and 95% confidence intervals (CIs). The variables that presented a p value lower than 0.20 in the bivariate analysis were selected to construct the initial multiple model, as well as variables with clinical relevance highlighted in the literature, such as age, body mass index (BMI), i.e., the individual’s weight in kilograms divided by height in squared meters (kg/m2), and systemic arterial hypertension [12]. Subsequently, the presence of multicollinearity between the variables was tested. Significant variables remained in the final model at a level of 5%. To evaluate the quality of adjustment and prediction ability of the logistic regression model, the Hosmer–Lemeshow [19] and Nagelkerke’s pseudo R2 [20] tests were used. Listwise deletion was applied to handle missing data collected during the acute phase of COVID-19. The assumption of missing at random (MAR) was evaluated. The software used in the analyses was R (version 4.1.2).
Ethical aspects
This study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of the Federal University of São João del-Rei, Divinopolis, number 4,614,603. All participants signed an informed consent form before the interview.
Results
A total of 699 individuals were interviewed. At the time of the interview, 91.5% of the patients had surpassed 120 days since the acute phase of the disease (4 months), while 8,5% were between 60 and 90 days. Of these, 187 met the criteria for long COVID, for a prevalence of 26.8% (95% CI: 23.5; 30.1). Table 1 presents the characterization of the signs and symptoms reported by patients with long COVID. The most reported changes were cognitive symptoms (49.7%), chronic diarrhea (49.2%) and cough (40.6%). The average number of complaints or persistent symptoms reported was 3.92 (SD = 2.82).Table 1 Characterization of self-reported complaints by patients with long COVID (n = 187)
Tables 2 and 3 show the results of the descriptive analysis of the global population and the comparisons between the two groups of individuals, those with (n = 187) and those without long COVID (n = 512). The largest proportion of respondents were women, aged between 30 and 49 years, high school education and lacked supplementary assistance. The most prevalent comorbidities were systemic arterial hypertension. The main complaints of patients in the acute phase of the disease were cough (23.2%), anosmia (21.8%), and headache (14.6%). With regard to the municipality of origin, 80.1% of the patients came from Teófilo Otoni.Table 2 Bivariate analysis of the sociodemographic data of patients with and without long COVID (N = 699)
Full size tableTable 3 Bivariate analysis of the clinical data of patients with and without long COVID (n = 699)
Table 4 shows the variables that made up the initial and final models. A greater chance of long COVID was detected in females (OR: 2.51; 95% CI 1.36; 4.63), in those with secondary education (OR: 2.13; 95% CI 1.07; 4.22) or elementary education (OR: 2.81; 95% CI 1.12; 7.04) than in those with higher education and postgraduate education; in those with a monthly income of 600 to 1,000 USD compared to the lowest income (OR; 5.85; 95% CI 1.20; 28.49); in those with supplementary health care (OR: 1.98; 95% CI 1.05; 3.73); in those who manifested anosmia in the acute phase (OR: 4.52; 95% CI 2.05; 9.98); and in those with the need for in-person care (OR: 2.44; 95% CI 1.02; 5.86). The Hosmer–Lemeshow test showed good model fit (p value = 0.363), with Negelkerke’s R2 at 40%.Table 4 Sociodemographic and clinical characteristics of the initial and final models for the association with long COVID (n = 699)
Discussion
In this investigation, the prevalence of long COVID was 26.8%. Female individuals with less education, higher income, supplementary health assistance, anosmia and who required face-to-face care in the acute phase of COVID-19 had a greater chance of long COVID. The main persistent complaints were difficulty concentrating, memory lapses, chronic diarrhea, coughing, and skin rashes.
The prevalence of long COVID found in this study is close to that described by the WHO (2022), which was 10 to 20% [5, 6], diverging from the findings of Miranda [11] and O’Mahoney [21], which indicate a prevalence of 50.2% and 45%, respectively. The greater prevalence of COVID-19 in those investigations can be explained by the fact that they followed patients for longer periods — 14 months [11] and 126 days [21] — when compared to our investigation, as the patients evaluated here may have presented symptoms related to long COVID after participating in the interview, which occurred 120 days after the acute illness. Another explanation for the higher prevalence in the studies mentioned above could be the origin of the population that was recruited from hospitals, a place where individuals generally arrive with a more serious case of COVID-19 and with a greater risk of developing persistent symptoms or new complaints arising from the disease [1, 21].
In this study, long COVID was associated with female sex, aligning with findings from a retrospective cohort (OR 1.52, 95% CI 1.48–1.56) [10] and a longitudinal cohort, where women had higher odds of persistent fatigue or weakness (OR 1.43, 95% CI 1.04–1.96) and anxiety or depression (OR 2.00, 95% CI 1.48–2.69) [22]. Women under 50 are also five times more likely than men to develop prolonged symptoms [23]. While women typically exhibit stronger acute immune responses, they may experience more significant late reactions due to X chromosome-linked genes and female hormones, which could perpetuate a hyperinflammatory state post-acute phase [24]. Higher IgG antibody production in women may contribute to better acute outcomes but potentially exacerbate long-term manifestations. Additionally, women’s heightened attentiveness to bodily changes may enhance their perception and reporting of symptoms [25].
In our investigation, patients with lower education levels were more likely to develop long COVID compared to those with higher education or postgraduate degrees. In contrast, the meta-analysis by O’Mahoney [21] found no association between education level and long COVID, potentially due to the geographic homogeneity of included studies, with 55% originating from Europe. We suggest that higher education may reduce the risk of long COVID through improved health literacy, which enhances access to information about immune-boosting practices such as regular physical activity and a nutritious diet. Supporting this, Gil et al. observed that physically inactive patients had a 57% higher risk of post-COVID-19 complications [26].
TeleCOVID-MG users with monthly incomes between USD 600 and 1,000 (3–5 times the minimum wage in Brazil) had a higher likelihood of persistent COVID-19 symptoms compared to those with lower incomes. Notably, 90% of the Brazilian population earns less than USD 625 per month, with the national average income being USD 501 in late 2022 [18]. This suggests that the USD 600–1,000 income bracket represents a relatively higher socioeconomic group. Contrary to our findings, Subramanian’s retrospective cohort study associated long COVID with socioeconomic deprivation [10]. While additional research is needed to clarify the long-term effects of low income on this condition, it is known that vulnerable populations often face greater health challenges due to inequitable access to public resources [4]. Our findings may be explained by higher-income individuals’ greater health awareness, enabling them to identify and report symptoms earlier and seek timely medical care. The presence of supplementary health insurance in this group further supports the association between long COVID and higher income, facilitating diagnosis and treatment.
In this study, long COVID was not associated with advanced age, a finding that contrasts with other studies [10, 27, 28]. However, this lack of association may be explained by the relatively young age of the participants in our sample, with a mean age of 42.7 years. Young age individuals can have better health conditions and lower prevalence of comorbidities.
Assessing long COVID outcomes often requires laboratory and imaging techniques that may be unavailable in resource-limited settings, as was the case in Brazil’s public health system during the pandemic time [29]. Those with higher incomes and health insurance likely had greater access to consultations, diagnostic exams, and clinical evaluations, leading to improved self-perception of health and understanding of long COVID consequences. In Brazil, only 2.2% of individuals earning less than USD 46 per month have health insurance, compared to 86.8% of those earning more than USD 925 [18], reinforcing the association observed in this study.
In our study, individuals with anosmia during the acute phase were more likely to develop long COVID. Anosmia or hyposmia was present in 29.9% of long COVID patients compared to 18.8% of those without it, consistent with findings by Lopez-Leon (21%) and higher than those reported by O’Mahoney (14.3%) and Chen (7%) [1, 12, 21]. Persistent anosmia may result from olfactory pathway degeneration, neuroinflammation, or sensory information loss, potentially leading to brain atrophy. COVID-19-related signaling pathways and viral entry into central nervous system cells may disrupt brain homeostasis, contributing to long-term neurocognitive effects. Anosmia could therefore be an early indicator of neurocognitive changes in long COVID [30].
Another variable identified in this study as associated with long COVID was the need for in-person care in the acute phase of the disease. This variable is believed to be related to greater severity of the clinical condition. Remote care was essential during the COVID-19 pandemic, whether to alleviate the burden on the healthcare system or to offer care to patients at an opportune time [13] however, some patients still need in-person care. In the present investigation, 30% of patients classified as having long COVID needed to be referred by the remote team for in-person care at primary health care units or hospital emergency departments in the acute phase of the disease due to complications and/or worsening of the clinical condition, and in the remaining patients, only 14% presented this need. Although long COVID may be present in individuals with mild symptoms and even in asymptomatic individuals [11], there is a consensus in the literature that it tends to be more prevalent in those with more severe manifestations and who require hospitalization in the acute setting [1, 11, 21].
In patients with long COVID, the most common symptoms were cognitive issues, chronic diarrhea, cough, anosmia, and dyspnea, with an average of four symptoms per patient. Lopez-Leon’s meta-analysis (2021) [12] identified the five most common symptoms as fatigue, headache, cognitive symptoms, alopecia and dyspnea. Similarly, Miranda (2022) [11] reported fatigue, cough, dyspnea anosmia/ageusia, and headache. Cheetham’s prospective cohort study (2023) [31] found that cognitive deficits; commonly referred to as brain fog; persisted for up to two years after infection, were more pronounced in long COVID patients and those with severe infections and were less frequent in vaccinated individuals. These deficits significantly impact daily activities, including work, home tasks, and childcare [31].
As long COVID is a recent condition, a lack of standardized data collection methods may contribute to heterogeneity in findings. While many articles referenced in this study were meta-analyses and systematic reviews, divergences between results were observed. Munblit et al. [29] highlighted that the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) developed protocols to monitor and study long COVID in adults and children, assessing prevalence and risk factors. Similarly, the WHO introduced a standardized form to evaluate medium and long-term consequences of this disease. Despite these efforts, the rapid proliferation of research tools, often implemented without adequate testing or validation, has likely exacerbated inconsistencies in results [29].
This study provides important insights into long COVID in patients treated via telecare during the pandemic, but some limitations must be considered. First, the cross-sectional design assessed long COVID at a single point in time, making it impossible to track symptom progression or new symptom emergence. Second, the short interval between the acute phase and the assessment (60 days) may have been insufficient to capture the development of chronic conditions. Third, at the time of the interviews, there was still no vaccination in Brazil, so all selected patients did not receive immunization, which may have worsened the symptoms. Additionally, information bias may have influenced the results. Telecare, during the acute phase, was conducted during isolation, when patients were more available and engaged, while long COVID interviews occurred later, potentially excluding healthier individuals who had returned to their routines and contributing to an overestimation of prevalence. We also did not investigate whether participants received specific treatment for long COVID, which could affect symptom prevalence. Finally, the results may lack generalizability, as 80.1% of participants were from Teófilo Otoni.
Although it has some limitations, this study is essential for helping individuals understand Long COVID, as it contributes to the visibility of this new morbidity, which has such an impact on the population. The results shown here and the associations found are of great importance and can contribute to planning care aimed at this population. The strengths of this investigation are reinforced by the fact that it is an analytical study conducted with a robust database that contributes to revealing this new morbidity, long COVID.
This study underscores the vital role of telehealth in primary care, particularly during the COVID-19 pandemic. Already widely utilized in Brazil [16], telehealth proved to be an essential, cost-effective, and accessible tool for managing isolated patients lacking support for a novel and poorly understood disease [3, 17]. In this project, only 15% of patients receiving remote care required face-to-face consultation. This finding serves as an indicator of effectiveness and resolution, in addition to demonstrating patient satisfaction with the care received [32]. Beyond its effectiveness during the pandemic, telehealth demonstrates significant potential for addressing future healthcare needs, including providing specialist support for persistent symptoms associated with long COVID. Prior to the COVID-19 pandemic, teleconsultations in Brazil had been restricted to interactions between healthcare professionals. However, following the pandemic, direct patient care through teleconsultation was authorized.
Conclusion
COVID-19 affected nearly one-third of the patients in this study, particularly impairing concentration and memory. Although the pandemic is under control, the virus continues leaving unanswered questions about its long-term complications. To advance understanding of long COVID, future research should prioritize prospective cohort studies to track patients over time, systematic reviews to synthesize emerging evidence, and investigations into specific factors such as the biological mechanisms underlying persistent symptoms, effective interventions for cognitive and neurological impairments, and disparities in long COVID outcomes across diverse populations.
