By Patricia Weiser, PharmD
COVID vaccine access may be more limited for some groups, after federal health officials changed recommendations. Here’s what to know about the latest COVID vaccine schedule.
Key Takeaways
- In May 2025, U.S. Health and Human Services Secretary Robert F. Kennedy, Jr. removed COVID-19 vaccines from the list of routine immunizations for healthy pregnant women and children. This decision has sparked concern among public health experts who warn that it may reduce protection for vulnerable populations and hinder vaccine access through insurance.
- Although the pandemic phase has passed, COVID continues to evolve. Updated vaccines offer protection against severe illness, hospitalization and long COVID.
- Health experts and organizations like the American College of Obstetricians and Gynecologists (ACOG) still recommend getting the COVID vaccine during pregnancy, citing the heightened risk of complications and the protective benefits for infants. Some fear the guideline changes could reduce vaccine uptake and insurance coverage, putting more people at risk.
- Personal health factors – including age, underlying health conditions, pregnancy status and previous vaccine history – which vaccine and how many doses you may need. People at high risk – including older adults, people with chronic conditions and those with weakened immune systems – benefit the most and may require additional doses to maintain protection.
- Talk to your health care provider to better understand what’s best for you and your loved ones.
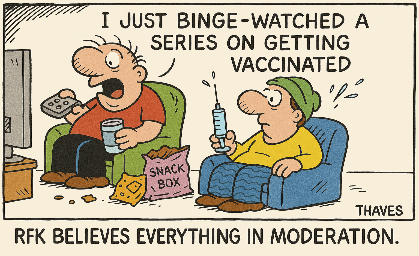
After years of updates on COVID-19 vaccines and boosters, it can be confusing to know who should get a shot and when. While a lot of that confusion has to do with the new COVID strains that have emerged, recent changes to federal vaccination guidelines by U.S. Health and Human Services Secretary Robert F. Kennedy, Jr. have made it more complicated.
On May 27, 2025, Kennedy announced that COVID-19 vaccines have been removed from the list of routine immunizations recommended for healthy pregnant women and children.
However, many health experts are concerned about the changing vaccination guidelines and what it means for public health.
“Recent changes to COVID-19 vaccine guidance are worrisome,” says Dr. Naima Joseph, assistant professor of medicine at Boston University and vice chair of the Society for Maternal-Fetal Medicine’s committee on infectious disease and emerging threats.
Although we’re no longer in the midst of a global pandemic, it’s important not to let our guards down. The COVID virus continues to evolve into new variants that evade our immune systems, but staying up-to-date with current vaccines can help you fight off infection from circulating strains.
Here’s what you need to know about the latest vaccine recommendations and how they may apply to you or your loved ones.
Overview of COVID Vaccines and Boosters
COVID vaccines help your immune system develop active immunity to recognize and fight the virus. Regardless of which vaccine you receive, it typically takes about two weeks after vaccination to build full protection.
There are two types of COVID vaccines available:
Why It’s Still Important to Be Current on COVID Vaccines
Like all viruses, the virus that causes COVID continues to change – mutating into new variants that evade our immune systems.
COVID vaccines help your body build stronger, more reliable immunity to protect against the virus – even as new variants continue to emerge. Vaccines remain safe and are carefully monitored for side effects.
Here are a few benefits of getting the COVID vaccine, according to the Centers for Disease Control and Prevention:
- Lower risk of severe illness. The COVID vaccine helps shorten the length and severity of illness if you do get infected. It reduced the risk of severe illness by about 70% in adults within two months of vaccination, with protection around 50% after 10 months.
- Reduced hospitalizations. Vaccinated adults had a 50% lower risk of needing hospitalization within two months of getting the vaccine. After 10 months, the risk was reduced to around 30%.
- Fewer emergency visits. The COVID vaccine lowered the risk of needing urgent care or emergency care among vaccinated adults by 50% within the first two months.
- Reduced risk of long COVID. Vaccinated people who later get COVID were less likely to develop long COVID than unvaccinated people or those who hadn’t received their latest boosters.
Who’s at risk?
COVID vaccines are especially important for people at higher risk of serious illness. That includes:
- Unvaccinated individuals
- Adults 65 and older (who make up most COVID-related deaths)
- People living in long-term care facilities, such as nursing homes
- People with certain health conditions, such as kidney disease, diabetes, heart conditions or obesity
- People with weakened immune systems
In people with weaker immune systems, vaccines can lower the risk of hospitalization by 36% in the first two months, though protection fades over time, which is why some may need another dose after six months.
New COVID Variant NB.1.8.1: What to Know
A new variant, NB.1.8.1, also known as Nimbus, has recently been detected in the United States after contributing to a surge of cases in Asia. Experts believe it could lead to a summer wave of infections in the U.S. as well.
NB.1.8.1 is part of the Omicron family and may spread more easily than earlier variants like LP.8.1. COVID symptoms for NB.1.8.1 remain similar to those seen with prior variants, including fever, chills, fatigue, cough, shortness of breath and loss of taste or smell. However, reports of “razor blade throat,” a new symptom characterized by a severely painful sore throat, have emerged.
“Elderly patients may experience more atypical symptoms, such as weakness, decreased appetite, falls and dehydration,” says Dr. Maher Madhoun, director of clinical operations and infectious disease specialist at Stamford Health.
So far, testing and treatments remain the same for NB.1.8.1. Treatment for mild illness continues to focus on supportive care, such as rest and fluids. For patients at higher risk, including older adults and those with underlying conditions, the antiviral pill Paxlovid may be used. For hospitalized patients with low oxygen levels, the IV steroid dexamethasone remains a key therapy.
Updated COVID Vaccine Schedule Recommendations
In general, health experts recommend an updated COVID vaccine or booster for most adults annually. The CDC’s vaccine recommendations vary depending on your age, health status and previous vaccination history, as follows.
Adults (ages 19 and 64)
If you haven’t been vaccinated yet, you should receive either one dose of an mRNA vaccine or two doses of Novavax spaced several weeks apart.
If you’ve already been vaccinated before the 2024-2025 season, you can get one updated mRNA dose at least eight weeks after your last dose.
Those who previously received Novavax may receive either one additional Novavax dose or one mRNA dose, depending on timing. People who received the Janssen vaccine in the past can receive one mRNA dose to update their protection.
Older adults (ages 65 and up)
The recommendations for this population are similar, but they also include a second dose after six months to help maintain protection, as aging affects immunity.
If unvaccinated, you can receive either one dose of an mRNA vaccine or two doses of Novavax, followed by an additional dose six months later.
Those who were vaccinated before the 2024-2025 season follow the same schedule as younger adults, with an extra dose at the six-month mark.
Pregnant and breastfeeding people
The COVID-19 vaccine will now only be recommended for pregnant women who are immunocompromised, regardless of previous vaccination status.
Although COVID-19 vaccines have been removed from the HHS’s list of routine immunizations for healthy pregnant women, the American College of Obstetricians and Gynecologists continues to strongly recommend the COVID vaccine. Pregnant and breastfeeding people can safely receive either vaccine type at any time during pregnancy or while breastfeeding.
It’s a good idea to speak with your health care provider to discuss the best approach based on your individual circumstances.
Children (ages 6 months to 17 years)
The COVID vaccines were originally on the list of recommended vaccines for children ages 6 months to 17 years, but as of May 2025, the shots are only recommended after consulting with the child’s health care provider. Parents should talk with their child’s pediatrician about their vaccination options.
Currently, the Pfizer and Moderna (Spikevax) vaccines are approved for children as young as 6 months old, while Novavax is approved for those 12 and older.
Growing Public Health Concerns
Many health experts have raised serious concerns about the decision to remove COVID vaccines from the list of recommended shots for healthy pregnant women and children.
While COVID in kids tends to be milder, some children can get very sick, especially babies. Pregnant people face higher risks too, and vaccination helps protect both them and their newborns.
The new vaccine guidelines “ignore strong evidence showing that pregnant people with COVID-19 have a higher risk of being hospitalized and that the vaccine is safe and helps protect against severe illness during pregnancy,” Joseph says. “Babies under 6 months old are also at high risk for hospitalization but are too young to get the vaccine, so the only way to protect them is through vaccination during pregnancy.”
This change could make it more difficult for some people to access the vaccines. Because insurers often rely on CDC guidelines when deciding which vaccines to cover, many insurance companies may stop paying for COVID-19 vaccines for these groups.
The COVID vaccine recommendations will likely shift again before the 2025-2026 season.
Bottom Line
COVID-19 vaccine recommendations continue to evolve as the virus changes and policies shift. Updated vaccines remain important for protecting adults, especially those who are at higher risk for severe illness. The recent removal of routine COVID vaccine recommendations for healthy pregnant people and children has sparked debate among experts who emphasize the ongoing safety and benefits of vaccination for these groups.
If you’re unsure whether you or your child should receive an updated COVID vaccine, speak with your health care provider. They can help you navigate the latest guidance and make the best decision for your personal situation.