Authors: Yuyang Lei,1,2,*Jiao Zhang,1,2,5,*Cara R. Schiavon,8,9Ming He,5Lili Chen,2Hui Shen,5,10Yichi Zhang,5Qian Yin,2Yoshitake Cho,5Leonardo Andrade,8Gerald S. Shadel,9Mark Hepokoski,6Ting Lei,3Hongliang Wang,4Jin Zhang,7Jason X.-J. Yuan,6Atul Malhotra,6Uri Manor,8,†Shengpeng Wang,2,†Zu-Yi Yuan,1,† and John Y-J. Shyy5,†
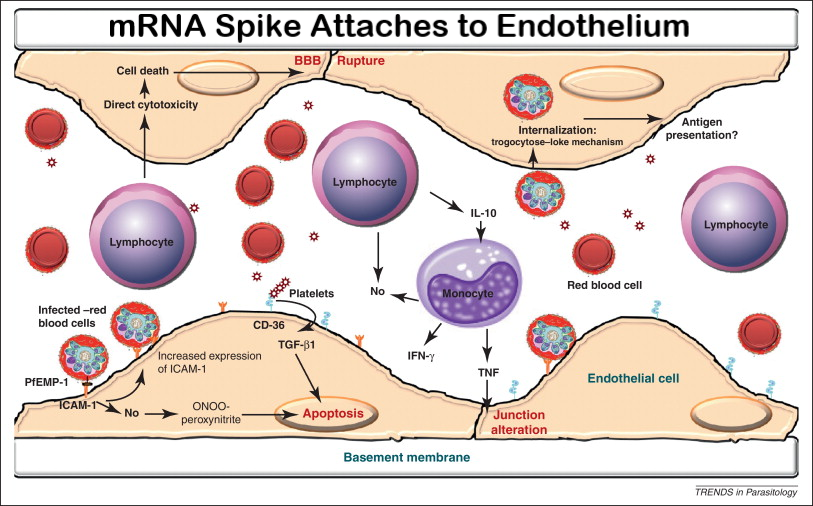
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) infection relies on the binding of S protein (Spike glycoprotein) to ACE (angiotensin-converting enzyme) 2 in the host cells. Vascular endothelium can be infected by SARS-CoV-2,1 which triggers mitochondrial reactive oxygen species production and glycolytic shift.2 Paradoxically, ACE2 is protective in the cardiovascular system, and SARS-CoV-1 S protein promotes lung injury by decreasing the level of ACE2 in the infected lungs.3 In the current study, we show that S protein alone can damage vascular endothelial cells (ECs) by downregulating ACE2 and consequently inhibiting mitochondrial function.
We administered a pseudovirus expressing S protein (Pseu-Spike) to Syrian hamsters intratracheally. Lung damage was apparent in animals receiving Pseu-Spike, revealed by thickening of the alveolar septa and increased infiltration of mononuclear cells (Figure [A]). AMPK (AMP-activated protein kinase) phosphorylates ACE2 Ser-680, MDM2 (murine double minute 2) ubiquitinates ACE2 Lys-788, and crosstalk between AMPK and MDM2 determines the ACE2 level.4 In the damaged lungs, levels of pAMPK (phospho-AMPK), pACE2 (phospho-ACE2), and ACE2 decreased but those of MDM2 increased (Figure [B], i). Furthermore, complementary increased and decreased phosphorylation of eNOS (endothelial NO synthase) Thr-494 and Ser-1176 indicated impaired eNOS activity. These changes of pACE2, ACE2, MDM2 expression, and AMPK activity in endothelium were recapitulated by in vitro experiments using pulmonary arterial ECs infected with Pseu-Spike which was rescued by treatment with N-acetyl-L-cysteine, a reactive oxygen species inhibitor (Figure [B], ii).Open in a separate windowFigure.
SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Spike protein exacerbates endothelial cell (EC) function via ACE (angiotensin-converting enzyme) 2 downregulation and mitochondrial impairment. A, Representative H&E histopathology of lung specimens from 8- to 12 wk-old male Syrian hamsters 5-day post administration of pseudovirus overexpressing Spike protein (Pseu-Spike) or mock virus in control group (n=3 mice per group, 1×108 PFU). Thickened alveolar septa (red arrowhead) and mononuclear cell (red arrow). Scale bar=20 μm. B, Pseu-Spike (n=4) or mock virus (n=4)–infected hamster lungs were subjected to Western blot analysis for pAMPK (phospho-AMPK) T172, AMPK, pACE2 (phospho angiotensin-converting enzyme) S680, ACE 2, MDM2, peNOS S1176, peNOS T494, eNOS (endothelial NO synthase), and β-actin (B, i). Human pulmonary arterial EC (PAECs) were infected with Pseu-Spike or mock virus for 24 h with or without N-acetyl-L-cysteine (NAC; 5 mmol/L) pretreatment for 2 h. The protein extracts were analyzed by Western blot using antibodies against proteins as indicated (n=4; B, ii). C, Representative confocal images of mitochondrial morphology of ECs treated with human recombinant S1 protein or IgG (4 μg/mL) for 24 h (C, i) or infected with human adenovirus ACE2 S680D (ACE2-D) or ACE2 S680L (ACE2-L; 10 MOI) for 48 h (C, ii). Mitochondria were visualized using TOM20 antibody (n=4, 50 cells counted for each replicate). Scale bar=2.5 μm. Tubular: the majority of mitochondria in ECs was >10 μm in length; Intermediate: the mitochondria were <≈10 μm; Fragment: the majority of mitochondria were spherical (no clear length or width). D, Measurement of oxygen consumption rate (OCR, D, i and iii) and extracellular acidification rate (ECAR, D, ii and iv) in ECs infected with ACE2-D vs ACE2-L (10 MOI) for 48 h (n=3) or treated with IgG vs S1 protein (4 μg/mL) for 24 h (n=3). E, Real-time quantitative polymerase chain reaction analysis of the indicated mRNA levels in lung ECs from ACE2-D (n=4) and ACE2-L (n=4) knock-in mice. Eight-week-old ACE2-D and ACE2-L male mice with C57BL/6 background were used. F, Dose-response curves of acetylcholine (ACh, left)- and sodium nitroprusside (SNP, right)–mediated relaxation on the tension of phenylephrine (1 μmol/L) precontracted intrapulmonary artery stripes from Pseu-Spike-(ACh n=8, SNP n=5) or mock (ACh n=6, SNP n=5) virus–infected Syrian hamsters (1×108 PFU; F, i) and ACE2-D (n=6) or ACE2-L (n=5) mice (F, ii). The animal experiments were approved by the ethical committee of Xi’an Jiaotong University. 2-DG indicates 2-Deoxy-D-glucose; ACE2-D, a phospho-mimetic ACE2 with increased stability; ACE2-L, a dephospho-mimetic ACE2 with decreased stability; AMPK, AMP-activated protein kinase; AA/R, antimycin A&Rotenone; ENO2, enolase 2; FCCP, carbonyl cyanide-p-(trifluoromethoxy)phenylhydrazone; H&E, Hematoxylin and Eosin; HK2, hexokinase 2; HO1, heme oxygenase-1; MDM2, murine double minute 2; MOI, multiplicity of infection; NRF1, nuclear respiratory factor 1; peNOS, phospho-eNOS; PFKFB3, 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3; Resp, respiration; and TFAM, transcription factor A, mitochondrial.
We next studied the impact of S protein on mitochondrial function. Confocal images of ECs treated with S1 protein revealed increased mitochondrial fragmentation, indicating altered mitochondrial dynamics (Figure [C], i). To examine whether these mitochondrial changes were due, in part, to the decreased amount of ACE2, we overexpressed ACE2 S680D (ACE2-D, a phospho-mimetic ACE2 with increased stability) or S680L (ACE2-L, a dephospho-mimetic with decreased stability)4 in ECs. As shown in Figure [C], ii, ECs with ACE2-L had a higher number of fragmented mitochondria when compared to those with ACE2-D. Performing oxygen consumption rate and extracellular acidification rate assays, we found that ECs overexpressing ACE2-L had reduced basal mitochondrial respiration, ATP production, and maximal respiration compared to ECs overexpressing ACE2-D (Figure [D], i). Moreover, ACE2-L overexpression caused increased basal acidification rate, glucose-induced glycolysis, maximal glycolytic capacity, and glycolytic reserve (Figure [D], ii). Also, ECs incubated with S1 protein had attenuated mitochondrial function but increased glycolysis, when compared with control cells treated with IgG (Figure [D], iii and iv). We also compared the expressions of mitochondria- and glycolysis-related genes in lung ECs isolated from ACE2-D or ACE2-L knock-in mice.4 Shown in Figure [E], the mRNA levels of NRF1, HO1, and TFAM (mitochondria biogenesis-related genes) were increased, whereas those of HK2, PFKFB3, and ENO2 (glycolysis-related genes) were decreased in lung ECs in ACE2-D mice, as compared to those in ACE2-L mice.
SARS-CoV-2 infection induces EC inflammation, leading to endotheliitis.1,5 Because S protein decreased ACE2 level and impaired NO bioavailability, we examined whether S protein entry is indispensable for dysfunctional endothelium. As shown in Figure [F], i, the endothelium-dependent vasodilation induced by acetylcholine was impaired in pulmonary arteries isolated from Pseu-Spike-administered hamsters, whereas the endothelium-independent vasodilation induced by sodium nitroprusside was not affected. We also compared the acetylcholine- and sodium nitroprusside–induced vasodilation of pulmonary vessels from ACE2-D or ACE2-L mice. As anticipated, acetylcholine-induced vasodilation was hindered in pulmonary arteries isolated from ACE2-L mice in comparison to ACE2-D mice (Figure [F], ii). There was, however, little difference in sodium nitroprusside–induced vasodilation between ACE2-D and ACE-L animals.
Although the use of a noninfectious pseudovirus is a limitation to this study, our data reveals that S protein alone can damage endothelium, manifested by impaired mitochondrial function and eNOS activity but increased glycolysis. It appears that S protein in ECs increases redox stress which may lead to AMPK deactivation, MDM2 upregulation, and ultimately ACE2 destabilization.4 Although these findings need to be confirmed with the SARS-CoV-2 virus in the future study, it seems paradoxical that ACE2 reduction by S protein would decrease the virus infectivity, thereby protecting endothelium. However, a dysregulated renin-angiotensin system due to ACE2 reduction may exacerbate endothelial dysfunction, leading to endotheliitis. Collectively, our results suggest that the S protein-exerted EC damage overrides the decreased virus infectivity. This conclusion suggests that vaccination-generated antibody and/or exogenous antibody against S protein not only protects the host from SARS-CoV-2 infectivity but also inhibits S protein-imposed endothelial injury.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8091897/