Uwe Wollina 1,✉, Jean Kanitakis 2, Robert Baran 3, PMCID: PMC8420555 PMID: 34398500
Abstract
The SARS‐CoV‐2 infection, responsible for COVID‐19, has raised the interest for infection‐associated muco‐cutaneous symptoms. While dermatologic symptoms in general gained an increasing awareness, affection of the nail organ has been mentioned only recently. We provide a narrative review on COVID‐19 manifestation on the nail organ and add symptoms induced by personal protective measures and SARS‐CoV‐2 vaccination. Available treatment options are discussed.
Keywords: COVID‐19, COVID‐vaccination, nail diseases, nail organ, protective measures, SARS‐CoV‐2, treatment
1. INTRODUCTION
In 2019, a new highly contagious viral disease emerged in China. Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) was identified as the responsible pathogen and the disease was termed coronavirus disease‐19 (COVID‐19). On March 11, 2020, the WHO declared COVID‐19 as a pandemic disease. 1 Cardiovascular and pulmonary symptoms were major clinical symptoms, but soon it was observed that the systemic nature of this infection could affect all organs and tissues of the human body. Although cutaneous manifestations have only rarely been mentioned in the early reports from Wuhan, China, they gained increasing attention later when the pandemic affected Europe and America. 2 The dermatological signs of this systemic infection have been now categorized and have obtained a much better awareness. 3 , 4 , 5 , 6
In contrast to this, nail changes have only recently been identified as possible consequences of SARS‐CoV‐2‐infection. 7 We here review the current knowledge on this topic compared with that of 2020 and added treatment options for the various nail pathologies.
2. NAIL CHANGES INDUCED BY SARS‐COV‐2 INFECTION
2.1. Microvascular disturbances
Microvascular disturbances caused by SARS‐CoV‐2 can be observed by nailfold capillaroscopy. In an open trial with 82 COVID‐19 patients from Italy, pericapillary edema (80.5%), enlarged capillaries (61.0%), and sludge flow (53.7%) was reported. In addition, meandering capillaries and reduced capillary density has been observed in every second patient. Acute COVID‐19 infection was associated with a higher prevalence of hemosiderin deposits resulting from micro‐hemorrhages and micro‐thrombosis. Patients who recovered from COVID‐19 had a higher prevalence of capillary pathologies such as enlarged capillaries, meandering capillaries, loss of capillaries, and empty dermal papillae. 8
2.2. COVID‐toe or ‐finger
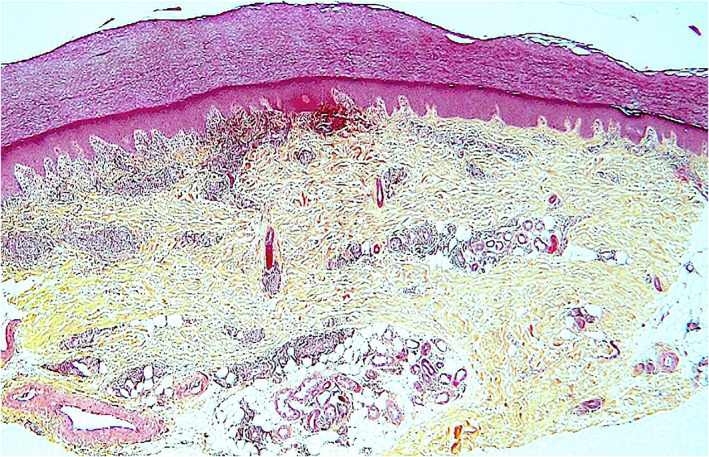
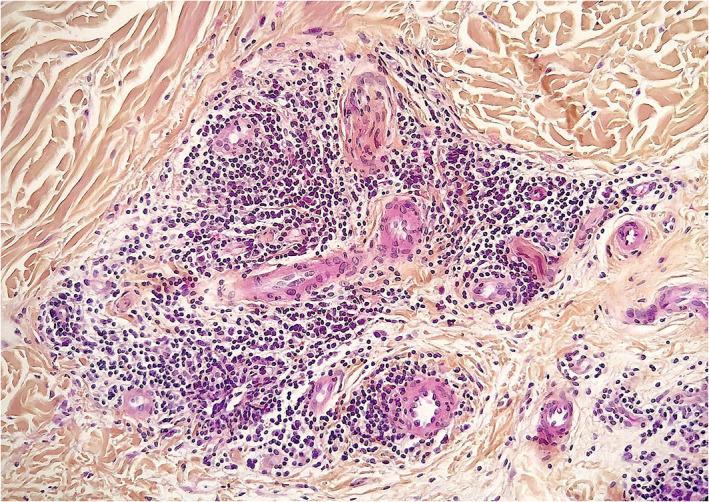
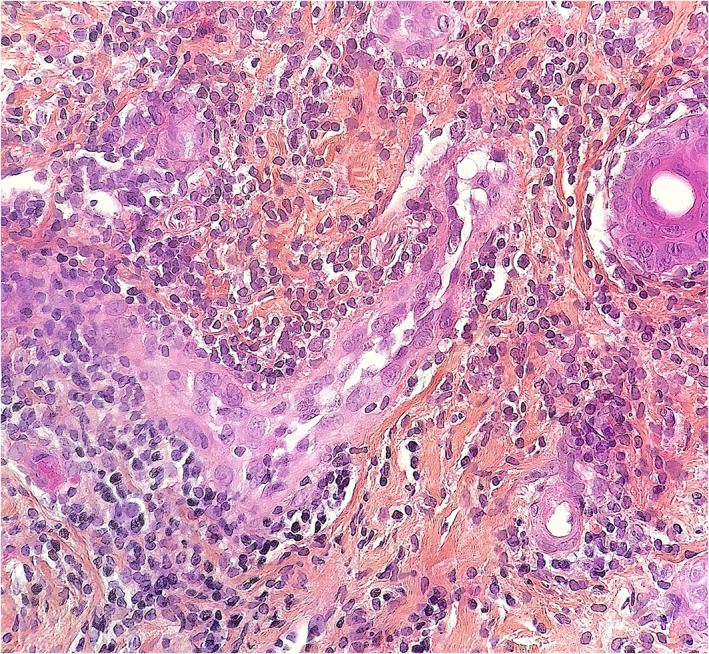
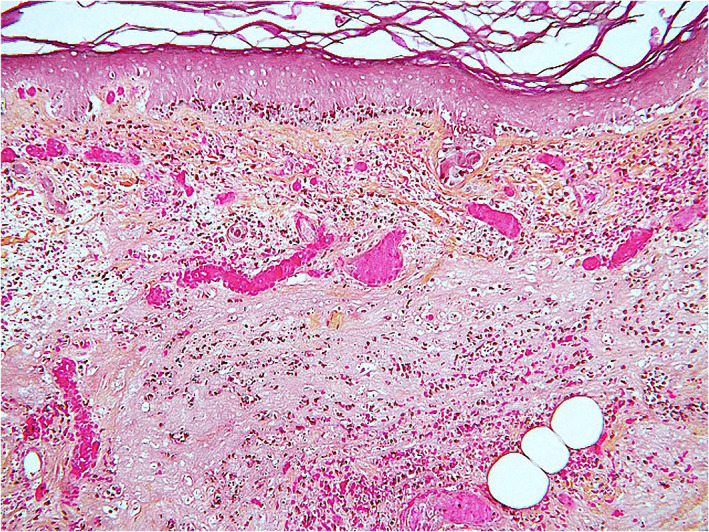
Kanitakis et al. (2020) studied 17 patients with suspected but unconfirmed SARS‐CoV‐2 infection and pernio‐like acral lesions. Histopathological findings of skin biopsies included deep horizontal parakeratosis (71%), necrosis of epidermal keratinocytes (41.5%), dispersed or confluents basal cell vacuolation (18%), spongiosis (12%), lymphocytic exocytosis (12%), dermal edema (76.5%), perivascular dermal lymphocytic infiltrate (100%), perivascular eosinophils (23.5%), endothelial cell swelling (65%), dermal mucin deposits (41.5%), microthrombi in superficial capillaries (12%) or venules (6%), dermal fibrin deposits (12%), and fibrin deposits in venule walls (18%). The dermal infiltrate consisted mainly of CD3+ lymphocytes, but rare B‐lymphocytes or plasma cells and rare activated CD30+ cells were intermingled. Direct immunofluorescence was positive in 82% of samples with vascular deposits of IgM (53%), IgA, and/ or C3 (29% each) (Figures 2, 3, 4). 10
In another study of 17 adolescents (median age 13.2 years), 16 (94.1%) had bilaterally localized distal erythematous or cyanotic lesions. Dermatoscopy discovered red dots (100%), white rosettes (68.8%), and white streaks (62.5%). Histology demonstrated a remodeling of dermal blood vessels with a lobular arrangement, vascular wall thickening, and a mild perivascular lymphocytic infiltrate. In these patients, a SARS‐CoV‐2 infection was excluded by in situ hybridization and serologic testing. 11
Thirty‐three patients (mean age 23.4 years) with chilblains during the COVD‐19 pandemic presented with erythematous and purpuric papules on the toes or fingers with edema and pruritus or burning sensation. Histology (n = 5) revealed superficial dermal lymphocytic infiltrates around vessels and eccrine sweat glands. None of these patients tested positive with two different antibody assays for SARS‐CoV‐2. 12
These findings question a causative relationship to SARS‐CoV‐2 infection, while other studies claimed the presence of SARS‐CoV‐2 spike proteins within blood endothelial cells and eccrine sweat glands. About 50% of patients with COVID‐toes or ‐fingers were positive for SARS‐CoV‐2. Most patients were young. 13 , 14
The serologic negativity in patients with COVID‐toes or ‐fingers might be due to a later seroconversion in milder cases, limited antibody production, or induction of an early robust innate immune response to SARS‐CoV‐2. 15 The presence of microthrombi in COVID‐toes and ‐fingers suggests an association with the observed coagulopathy in COVID‐19. 10 , 16
The most important differential diagnoses include frostbites (perniones) and chilblain lupus erythematosus. In familial chilblain lupus, loss‐of‐function mutations in the nucleases TREX1 or SAMHD1 have been identified characteristic of a type I interferonopathy. 17
2.3. Acral gangrene
A rare but severe symptom is acral gangrene (Figure 5). It is a red flag sign of acute severe infection with multisystemic inflammation and cardiovascular malfunction. 18
2.3.1. Treatment of microvascular symptoms
In case of young asymptomatic patients or patients without confirmation of SARS‐CoV‐2 infection COVID‐toe or finger is self‐limited and spontaneous resolution has been observed within 2–3 weeks. The basic treatment in early COVID‐19 stages consists of a combination of antiviral therapies (e.g., favipiravir, remdesivir, hydroxychloroquine, lopinavir plus ritonavir) with antithrombotic treatment, while in later advanced stages of the disease antithrombotic therapy should be combined with a treatment of the cytokine storm (e.g., tocilizumab, dexamethasone, interleukin‐1 or tumor necrosis factor‐beta antagonists). Antithrombotic treatment is using low‐molecular weight heparinoids or heparin. Heparin is capable of limiting endothelial damage such as glycocalyx shedding. These compounds have anticoagulant, antiviral, and anti‐inflammatory effects. 19 Oral corticosteroids in combination with low‐dose acetylsalicylic acid are the treatment of choice for cryofibrinogenemia. 20
2.4. Periungual desquamation
Periungual desquamation has been reported in children with severe Kawasaki‐like multisystemic inflammatory syndrome (MIS‐C) and adults recovering from severe COVID‐19. 21 , 22 Since coronary artery lesions have been observed in MIS‐C, it has been recommended to assess patients with severe COVID‐19 for such vascular symptoms. 23
2.4.1. Treatment
Moisturizers can be used to limit the symptoms.
2.5. Beau’s lines and onychomadesis
Beau’s lines are transverse grooves of the nails resulting from suppressed growth of the nail matrix by drugs or systemic infectious diseases. Beau’s lines have been observed among children and adults with COVID‐19. 24 , 25 , 26 Single or multiple nails may be affected–mostly fingernails. Beau’s lines can be accompanied by leukonychia. 24
Beau’s lines may precede onychomadesis, characterized by separation of the nail plate from the nail matrix, with persistent attachment to the nail bed. Onychomadesis is a possible consequence of COVID‐19. 27 , 28
Another late manifestation of COVID‐19 disease is a heterogeneous red–white discoloration of the nail bed with distal onycholysis. 29
2.5.1. Treatment
Onychomadesis and Beau’s lines are usually mild and self‐limited. In chemotherapy‐induced onychomadesis, high‐energy 633 nm red light (126 J/cm2 for 20 min every day) has been successful for fingernails but not toenails. 30
2.6. Discolorations of the lunula and the nail plate
A red‐violet band surrounding the distal margin of the nail lunula, is known as red half‐moon sign and has been observed in acute SARS‐CoV‐2 infection in adult patients. 31 , 32
Distal orange discolorations of the nail plates have been reported as a delayed response several weeks after COVID‐19 disease in elderly patients who developed later sarcopenia and anemia. 33
Nonblanchable transverse leukonychia (transverse white lines) was observed in a 47‐year‐old man with COVID‐19. These lines are due to abnormal keratinization of the nail plate. 34
2.6.1. Treatment of discolorations
There is no specific treatment of nail plate discolorations. It is most important to exclude infections (onychomycosis or bacterial infections). Colored nail lacquers can cover the symptoms. Transverse white lines may be persistent after severe damage of nail matrix.
2.7. Nail changes induced by COVID‐19 treatments
Favipiravir is a purine nucleoside precursor and competitive inhibitor of RNA‐dependent RNA polymerase. It is used in COVID‐19 off‐label with variable results. A yellow‐white fluorescence on the nails has been reported as an adverse event of favipiravir used for COVID‐19 disease. 35
Some patients on favipiravir developed a greenish fluorescence in the lunula and nail plate portion near the proximal nail fold. Green fluorescence has also been observed on the scalp hair made visible by Wood’s lamp illumination. It is not yet clear, whether the fluorescence is mainly caused by drug metabolites or by additives of the tablets, such as yellow ferric oxide. 36
Hydroxychloroquine is an antimalarial drug with anti‐viral activity in vitro that may cause hyperpigmentation of tissues. Hydroxychloroquine has been widely used in prevention and treatment of SARS‐CoV‐2 infection but sound evidence for a clinical benefit is lacking. Hydroxychloroquine‐induced longitudinal melanonychia is a possible adverse event. 37
The most important differential diagnosis of drug‐induced melanonychia is subungual melanoma, which warrants a nail biopsy. 38
2.7.1. Treatment
Drug‐induced nail changes will most often spontaneously disappear after withdrawal of the responsible drug. No specific treatment exists.
2.8. Nail changes induced by vaccination
Recently, some cases of pernio‐like lesions were reported that developed on the hands and/ or feet a few days after vaccination against COVID‐19 with RNA‐based vaccines (BionTec/ Pfizer, Moderna). 39 , 40 , 41 , 42 Histologic examination revealed findings indistinguishable from idiopathic and COVID‐19‐related perniones. 40 , 42
2.8.1. Treatment
Low‐dose acetylsalicylic acid with oral corticosteroids can be used in symptomatic and painful lesions. Due to temporary character of the vaccine‐induced perniones, often treatment is unnecessary.
2.9. Nail changes by protective measures
The green nail syndrome or Goldman‐Fox syndrome is caused by nail infection or colonization with P. aeruginosa. It is known as an occupational disease in health care workers, especially in intensive care units. Green nail syndrome has recently been reported in health care workers during the COVID‐19 pandemic (Figure 6). 43 , 44
2.9.1. Treatment
Treatment consists of oral ciprofloxacin. Topical treatment includes removal of the onycholytic part of the nail and brushing of the nail bed with 2% sodium hypochlorite solution twice daily for at least 6 weeks, and topical nadifloxacin, tobramycin, or gentamycin. 43 , 45
Irritant hand dermatitis has been observed more frequently during the COVID‐19 pandemic especially on health care workers on COVID‐19 departments. One study reported adverse cutaneous reactions to frequent hand washing and frequent use of disinfectants in up to 80.2%. 46 Nails can be affected due to wet work leading to brittle nails. Loss of cuticle is often seen together with a chronic irritant proximal nail fold dermatitis (Figure 5). 47
Recommendations of skin care have been developed by various medical bodies including the European academy of dermatology and venereology task force on contact dermatitis to avoid adverse effects of sanitary procedures on hands and nails. 46 Limitation of wet work, use of protective gloves, and regular use of moisturizers during the day and emollients overnight are helpful.
3. CONCLUSIONS
Affection of the nail by COVID‐19 has only recently been reported. The nail organ can be affected by SARS‐CoV‐2 infection in a number of ways. Some of these symptoms are indicators of a mild course like COVID‐toe or‐finger, while others are a red flag for a serious course like acro‐ulcerative lesions. The medical treatment of COVID‐19 may also interfere with the nail organ often with color changes of the nail plate. Vaccination with RNA‐based vaccines can induce pernio‐like acral lesions of digits. Prolonged use of protective gloves and wet work bear a risk for bacterial infection of the nail plate with Pseudomonas leading to chloronychia. Health care staff with chloronychia is a potential source of transmissible infections, especially in intensive care units, transplant centers, and hemato‐oncology departments.
