Five years into the COVID-19 pandemic, the global vaccination campaign has saved lives and reduced hospitalizations—but it has also sparked intense debate. Critics argue that the medical profession’s rapid and widespread administration of mRNA vaccines occurred without sufficient long-term safety data, raising ethical concerns about informed consent, risk transparency, and the durability of immunity.
⚖️ Ethical Concerns in Vaccine Administration
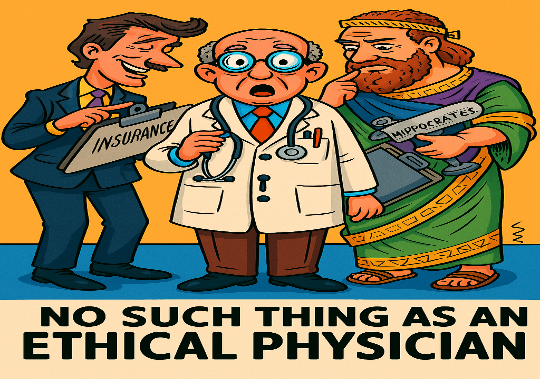
Some medical ethicists and patient advocates have raised alarms about what they call “vaccine overreach”—the practice of administering vaccines without fully disclosing uncertainties about long-term effects. Key concerns include:
- Lack of longitudinal safety data: Most studies tracked outcomes for weeks or months, not years
- Pressure to vaccinate: Social, professional, and governmental mandates often left little room for personal medical discretion
- Informed consent gaps: Patients may not have been told about rare but serious adverse events or the evolving nature of immunity
This has led some to describe the rollout as a form of medical overconfidence, where urgency eclipsed caution.
🧬 Do COVID Vaccines Confer Long-Term Immunity?
Contrary to early hopes, COVID-19 vaccines do not appear to confer durable sterilizing immunity. A 2024 NIH study found that mRNA vaccines failed to generate long-lived plasma cells in the bone marrow—cells responsible for sustained antibody production. Instead, protection wanes within months, requiring repeated boosters.
| Immune Feature | Observation |
|---|---|
| Long-lived plasma cells | Scarce after mRNA vaccination |
| Antibody levels | Decline within 3–6 months |
| Breakthrough infections | Common, even after multiple doses |
While boosters can temporarily restore antibody levels, critics argue this reflects short-term immune stimulation, not lasting protection. And, Boosters come with significant risks which become more pronounced with each shot.
🧠 Impact on Cellular Function and Immune Regulation
Emerging research has explored how mRNA vaccines affect cellular and immune dynamics:
- A 2025 study from the University of Cologne found persistent epigenetic changes in innate immune cells after mRNA vaccination3
- These changes may enhance immune readiness—but some researchers caution they could also alter inflammatory pathways or disrupt immune balance over time
- Concerns have been raised about spike protein persistence, which may interfere with cellular signaling in rare cases
While these findings are preliminary, they underscore the need for long-term surveillance and mechanistic studies.
🧪 Are We Missing the Bigger Picture?
Critics argue that public health messaging has leaned heavily on speculative modeling—such as counterfactual estimates of lives saved—without acknowledging the uncertainty behind these projections. Many models assume:
- Static behavior in unvaccinated populations
- Uniform vaccine efficacy across variants
- Minimal contribution from natural immunity
This has led some to question whether vaccine benefit claims are overstated, especially in younger, healthier populations.
🧭 Moving Forward: Transparency and Accountability
To restore trust and ensure ethical medical practice, experts recommend:
- Expanded long-term studies on fertility, cancer risk, and autoimmune conditions
- Clearer informed consent protocols for future vaccine campaigns
- Independent review of public health modeling and assumptions
- Open access to raw safety data for independent analysis
🧠 Final Thought
COVID-19 vaccines were a scientific triumph—but science also demands humility. As we learn more about their long-term effects, the medical profession must balance urgency with caution, and innovation with accountability. Scrutiny isn’t sabotage—it’s how medicine earns trust.