Abstract
The COVID-19 pandemic has unveiled a spectrum of long-haul symptoms, including persistent fatigue, cognitive dysfunction, and sleep disturbances. Recent case reports and longitudinal studies suggest a potential link between SARS-CoV-2 infection and the onset or exacerbation of narcolepsy—a chronic neurological disorder characterized by excessive daytime sleepiness and disrupted sleep architecture. This article reviews emerging evidence on the immunological and neurobiological mechanisms that may connect COVID-19 with narcoleptic syndromes.
🦠 Introduction
Narcolepsy affects approximately 44.3 per 100,000 individuals and is categorized into two types: Type 1 (NT1), associated with cataplexy and hypocretin deficiency, and Type 2 (NT2), which lacks cataplexy and typically retains normal hypocretin levels. The disorder is believed to have autoimmune underpinnings, particularly in NT1, where T-cell mediated destruction of hypocretin-producing neurons in the lateral hypothalamus is implicated.
COVID-19, caused by SARS-CoV-2, has been associated with a wide range of neurological sequelae. Among long-haul patients, sleep disturbances—including hypersomnia and fragmented sleep—are frequently reported. The overlap between these symptoms and narcolepsy has prompted investigations into whether COVID-19 may trigger or unmask narcoleptic syndromes.
🧬 Etiology: How COVID-19 May Trigger Narcolepsy
- Autoimmune Hypothesis: SARS-CoV-2 may trigger an autoimmune response that damages hypocretin (orexin)-producing neurons in the lateral hypothalamus—key regulators of wakefulness2.
- Post-Infectious Mechanism: Similar to the H1N1 pandemic, viral infections may activate T-cells that cross-react with sleep-regulating neurons, especially in genetically predisposed individuals (e.g., those with HLA DQB1*0602).
- Inflammatory Cascade: Neuroinflammation and cytokine storms during COVID-19 may disrupt sleep architecture and circadian regulation.
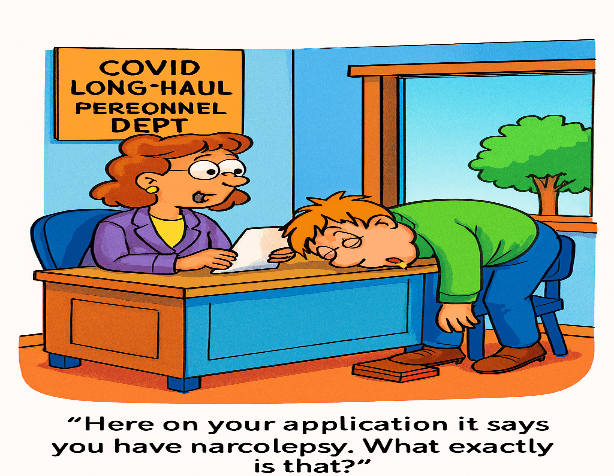
😴 Symptoms of COVID-Induced Narcolepsy
- Excessive Daytime Sleepiness (EDS): Involuntary naps, inability to stay awake during the day
- Sleep-Onset Insomnia: Difficulty falling asleep
- Sleep-Maintenance Insomnia: Frequent awakenings during the night
- Sleep-Onset REM Periods (SOREMs): Rapid transition into REM sleep
- Possible Symptoms:
- Cataplexy (sudden muscle weakness triggered by emotion) — more common in Type 1
- Hypnagogic hallucinations
- Sleep paralysis
🧪 Diagnosis & Tests
Clinical Evaluation
- Detailed sleep history and symptom tracking
- Rule out other causes of hypersomnia (e.g., depression, sleep apnea)
Sleep Studies
- Polysomnography (PSG): Overnight sleep study to assess sleep architecture
- Multiple Sleep Latency Test (MSLT): Measures how quickly a person falls asleep in quiet situations during the day; presence of ≥2 SOREMs is diagnostic for narcolepsy2
Biomarkers
- CSF Hypocretin Levels: Often low in Type 1 narcolepsy; borderline or normal in Type 2
- HLA Typing: DQB1*0602 variant may support autoimmune etiology
💊 Potential Therapies
Standard Treatments
- Wakefulness-Promoting Agents:
- Modafinil or armodafinil
- Solriamfetol or pitolisant
- Sodium oxybate: For cataplexy and disrupted nighttime sleep
Post-COVID-Specific Therapies
- Corticosteroid Pulse Therapy: High-dose methylprednisolone showed remission in a COVID-induced narcolepsy case, suggesting an autoimmune mechanism
- Immunomodulatory Approaches: Still experimental but may be considered in early onset cases with inflammatory markers
🧠 Summary
COVID-induced narcolepsy is rare but increasingly recognized. It may present as Type 1 or Type 2 narcolepsy, often without prior sleep disorder history. Diagnosis hinges on sleep studies and clinical correlation, and in some cases, immunosuppressive therapy may lead to remission.
Would you like help drafting a clinical summary or patient education sheet for this condition? I can also help visualize the hypothesized autoimmune pathway.
🧬 Pathophysiological Mechanisms
A case report published in Clinical Case Reports describes a 33-year-old woman who developed full-spectrum narcolepsy symptoms within two weeks of recovering from COVID-19. Sleep studies confirmed increased sleep latency and multiple sleep-onset REM periods, consistent with NT1 diagnosis.
Key proposed mechanisms include:
- Immune Activation: SARS-CoV-2 may provoke autoimmune responses targeting hypocretin neurons, similar to mechanisms observed during the H1N1 pandemic.
- Genetic Susceptibility: The HLA DQB1*0602 allele, prevalent in NT1 patients, may predispose individuals to post-viral narcolepsy.
- Neuroinflammation: COVID-19-related cytokine storms and blood-brain barrier disruption may facilitate central nervous system autoimmunity.
📊 Longitudinal Outcomes
A 4-year follow-up study published in Sleep and Biological Rhythms tracked 100 narcolepsy patients through the pandemic. Findings revealed:
- Increased daytime sleepiness and altered sleep efficiency during lockdown periods.
- NT1 patients experienced worsened physical role functioning post-pandemic.
- Medication adherence and flexible sleep schedules were critical to symptom management.
These results underscore the pandemic’s lasting impact on narcoleptic patients and suggest that COVID-19 may exacerbate pre-existing sleep disorders or contribute to new-onset cases.
🩺 Clinical Implications
Clinicians should maintain a high index of suspicion for narcolepsy in patients presenting with post-COVID fatigue, hypersomnia, or sleep fragmentation. Diagnostic sleep studies and HLA typing may aid in early identification. Given the chronic nature of narcolepsy, timely intervention can significantly improve quality of life.
🔍 Conclusion
While narcolepsy remains a rare condition, its potential emergence in the context of COVID-19 long-haul syndrome warrants further investigation. The intersection of viral immunology and sleep neurobiology presents a unique opportunity to deepen our understanding of post-infectious neurological disorders.
References
- Narcolepsy following COVID-19: A case report and review of potential mechanisms
- Long-term follow-up of symptom and quality of life changes in patients with narcolepsy during and after the COVID-19 pandemic