John Murphy, The COVID 19 Long-haul Foundation
Abstract
Long COVID, or post-acute sequelae of SARS-CoV-2 infection (PASC), presents a complex clinical landscape marked by persistent inflammation, fatigue, and multisystem dysfunction. Corticosteroids—particularly prednisone and dexamethasone—have been employed to mitigate inflammatory cascades in select long COVID phenotypes. However, prolonged steroid exposure carries risks, including the development of lipomatosis: a pathological proliferation of adipose tissue in ectopic or symmetric distributions. This article explores the intersection of steroid therapy and lipomatosis in long COVID patients, drawing on emerging evidence and established endocrinological mechanisms.
Introduction
Lipomatosis refers to the abnormal accumulation of adipose tissue, often in symmetric or infiltrative patterns, and is distinct from isolated lipomas. While rare, steroid-induced lipomatosis has been documented in chronic inflammatory conditions such as lupus, HIV, and sarcoidosis. In the context of long COVID, where corticosteroids are sometimes prescribed to manage persistent inflammation, the potential for lipomatosis warrants scrutiny.
Corticosteroids in Long COVID: Therapeutic Use and Risks
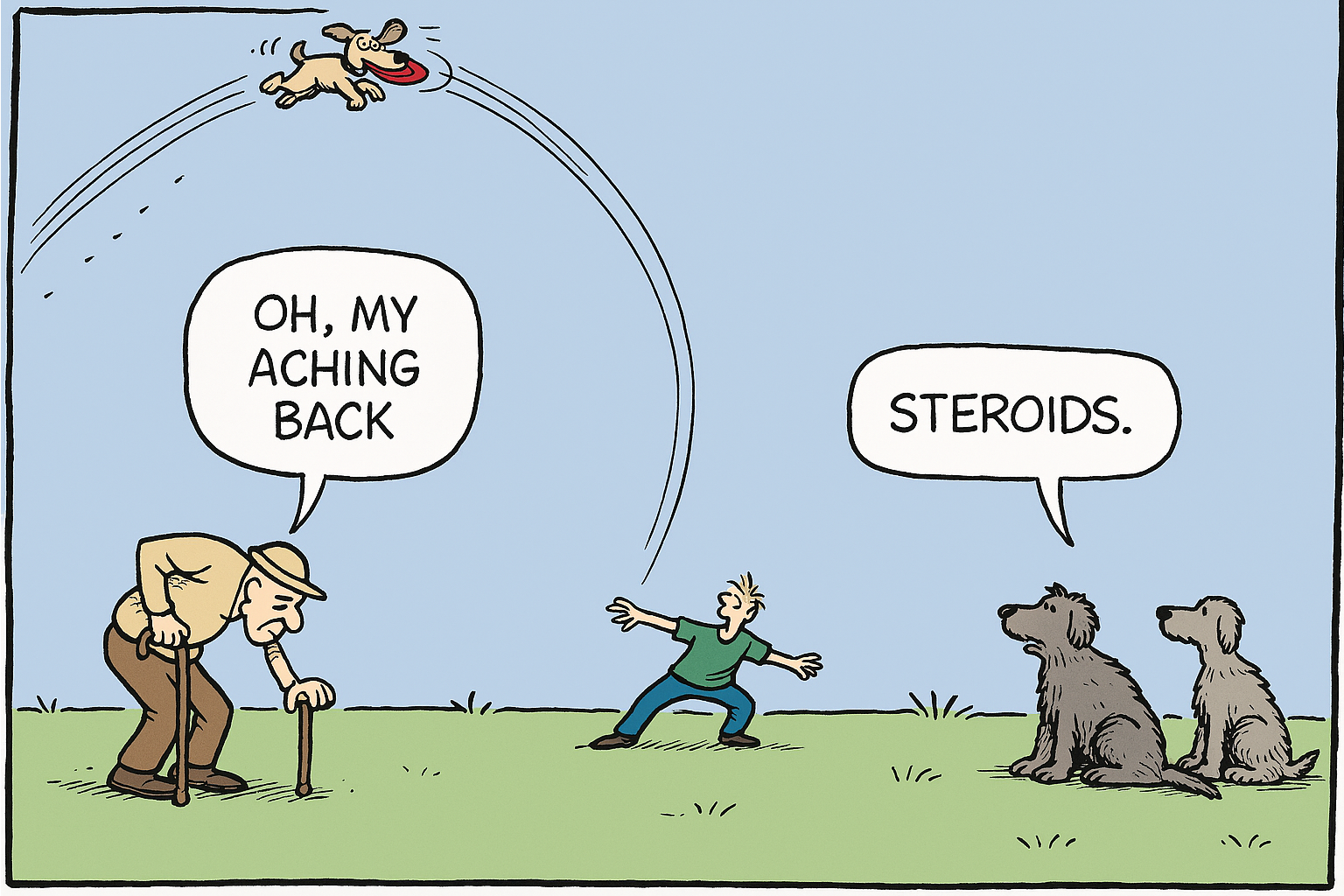
Steroids remain a cornerstone of acute COVID-19 management, with dexamethasone reducing mortality in hypoxic patients as demonstrated in the RECOVERY trial. In long COVID, low-dose prednisone has been used off-label to address lingering inflammation, particularly in patients with autoimmune-like symptoms or post-viral fatigue syndromes. A living systematic review in The BMJ identified corticosteroids among several pharmacologic interventions trialed for long COVID, though evidence remains limited and heterogeneous.
Mechanisms of Steroid-Induced Lipomatosis
Chronic corticosteroid exposure alters lipid metabolism, redistributes fat, and promotes adipocyte hypertrophy. This is mediated by:
- Glucocorticoid receptor activation, which upregulates lipogenic enzymes and downregulates lipolysis.
- Insulin resistance, a common side effect of steroids, which enhances adipose deposition.
- Suppression of growth hormone and sex steroids, contributing to altered body composition.
These mechanisms underlie conditions like Cushingoid appearance and steroid-induced lipomatosis, particularly in the cervical, dorsocervical (“buffalo hump”), and supraclavicular regions.
Lipomatosis in Long COVID: Emerging Observations
While direct studies on lipomatosis in long COVID are sparse, case reports and retrospective analyses suggest a pattern. Aiyegbusi et al. (2021) noted that long COVID patients treated with extended steroid courses reported new-onset fat redistribution and subcutaneous nodularity, raising concern for lipomatosis. Additionally, Wang et al. (2022) found that patients receiving steroids for more than three days had reduced mortality but higher rates of metabolic complications, including weight gain and dyslipidemia1.
In clinical practice, lipomatosis may be underdiagnosed due to its slow progression and overlap with general steroid-induced weight gain. However, its presence can impair mobility, exacerbate fatigue, and contribute to psychosocial distress—compounding the burden of long COVID.
Differential Diagnosis and Imaging
Lipomatosis must be distinguished from lipomas, liposarcomas, and steroid-induced myopathy. MRI and ultrasound can aid in identifying diffuse adipose infiltration versus encapsulated masses. Biopsy is rarely required unless malignancy is suspected.
Long-Term Management and Mitigation
For patients with steroid-associated lipomatosis, management includes:
- Steroid tapering, when clinically feasible, to reduce further adipose proliferation.
- Metabolic monitoring, including glucose, lipid panels, and body composition analysis.
- Physical rehabilitation, to counteract mobility limitations and muscle deconditioning.
- Surgical excision, in rare cases where lipomatosis causes functional impairment or disfigurement.
Alternatives to systemic steroids—such as localized injections, biologics, or non-steroidal immunomodulators—may reduce risk in susceptible individuals.
Conclusion
Lipomatosis represents a subtle but significant complication of corticosteroid therapy in long COVID. As clinicians navigate the balance between inflammation control and long-term safety, awareness of adipose dysregulation is essential. Future studies should quantify lipomatosis prevalence in steroid-treated long COVID cohorts and explore targeted interventions to mitigate its impact.