By Marty Makary, MD, and Vinay Prasad, MD, MPH (Rewritten for journal publication), edited: John Murphy, The COVID 19 Long-haul Foundation
Abstract
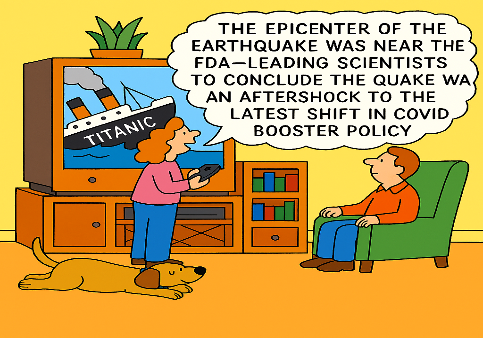
The U.S. Food and Drug Administration (FDA) has revised its COVID-19 vaccination policy, signaling a significant shift in its approach to booster recommendations. This article explores the rationale behind the FDA’s decision to limit booster approvals to high-risk populations, the scientific and ethical considerations driving this change, and the implications for public health, vaccine confidence, and regulatory integrity.
Introduction
Since the onset of the COVID-19 pandemic, the FDA has played a central role in evaluating and authorizing vaccines to mitigate the spread and severity of SARS-CoV-2. The initial rollout of mRNA vaccines in late 2020 marked a historic achievement in biomedical science, with rapid development, deployment, and widespread uptake. However, as the pandemic evolved, so did the virus—and with it, the public’s response to ongoing vaccination efforts.
In 2025, the FDA announced a pivotal change: it would no longer recommend annual COVID-19 boosters for healthy individuals under the age of 65. Instead, the agency would prioritize vulnerable populations—those over 65 and individuals with comorbidities or immunocompromised conditions. This decision reflects a broader reassessment of the clinical utility, public trust, and scientific rigor surrounding booster policies.
The Scientific Rationale: Immunogenicity vs. Clinical Benefit
Central to the FDA’s revised framework is the distinction between immunogenicity and clinical efficacy. While early vaccine trials demonstrated robust antibody responses, the correlation between these responses and meaningful clinical outcomes—such as reduced hospitalization or death—has become less clear over time, particularly in low-risk populations.
Dr. Marty Makary, FDA Commissioner, and Dr. Vinay Prasad, Director of the Center for Biologics Evaluation and Research, emphasized that future approvals for boosters in healthy individuals will require randomized controlled trials (RCTs) demonstrating tangible clinical benefits. “We can’t just extrapolate from a clinical trial from four or five years ago,” Makary stated at the American Hospital Association’s annual meeting. The FDA’s new policy mandates that Biologics License Applications for boosters in healthy individuals must be supported by outcome-driven data—not merely antibody titers.
This shift aligns the U.S. with peer nations such as Canada, the UK, and Australia, which have already limited booster recommendations to high-risk groups.
Public Trust and Vaccine Uptake
One of the most pressing concerns driving the FDA’s decision is the erosion of public trust in vaccines. Despite the initial success of COVID-19 vaccination campaigns, booster uptake has plummeted. Less than 25% of Americans received the most recent annual booster, and uptake among children under 12 is below 10%. Even among healthcare workers—once the most vaccinated demographic—booster rates have declined to roughly one-third.
Makary and Prasad argue that overextending booster recommendations to low-risk populations has contributed to skepticism not only about COVID vaccines but about vaccination more broadly. “The American people were skeptical, and some of them took that skepticism to every single vaccine, which has led to some big problems,” Prasad noted.
By narrowing the scope of recommendations, the FDA aims to restore credibility and reinforce the principle of evidence-based medicine. This recalibration is not a retreat from science—it is a recommitment to it.
Ethical Considerations: Risk, Benefit, and Autonomy
The ethical calculus of recommending medical interventions hinges on a balance of risks and benefits. For high-risk individuals, the benefits of COVID-19 boosters remain compelling. However, for healthy individuals—particularly children and young adults—the risk-benefit ratio is less favorable.
Makary posed a provocative question: “Should we really be putting the full weight of the government to urge vaccination against COVID for a healthy, thin 12-year-old girl with her seventh COVID booster right now today in America? I don’t think so”.
This sentiment underscores a broader ethical concern: the medicalization of low-risk populations without clear evidence of benefit. The FDA’s new policy respects individual autonomy while ensuring that public health recommendations are grounded in rigorous science.
Regulatory Integrity and the Role of Evidence
The FDA’s credibility depends on its commitment to transparent, evidence-based decision-making. In recent years, critics have accused the agency of succumbing to political pressure and pharmaceutical lobbying. Makary and Prasad’s policy seeks to reverse this trend by demanding “gold standard science” from vaccine manufacturers.
Future booster approvals will require RCTs that evaluate not just antibody levels but real-world outcomes. This approach reflects a maturation of the regulatory process—one that prioritizes long-term safety, efficacy, and public trust over expediency.
International Context and Comparative Policy
Globally, the trend toward targeted booster recommendations is well established. In the UK, boosters have been limited to vulnerable groups for several seasons. European regulators have similarly adopted risk-based frameworks, citing limited evidence for annual boosters in healthy populations.
The FDA’s new policy brings the U.S. into alignment with these international standards. It also reflects a growing consensus among immunologists that repeated boosting in low-risk individuals may offer diminishing returns—and could even pose risks, such as immune fatigue or adverse reactions.
Implications for Future Vaccine Development
The FDA’s revised stance has significant implications for pharmaceutical companies, clinical researchers, and public health officials. Vaccine developers will need to design trials that measure clinical endpoints, not just immunogenicity. Researchers must explore alternative strategies for long-term immunity, such as mucosal vaccines or pan-coronavirus platforms.
Public health officials will need to recalibrate messaging to emphasize targeted protection rather than universal boosting. This shift may also open the door to more personalized vaccination strategies, guided by individual risk profiles and emerging biomarkers.
Conclusion
The FDA’s decision to limit COVID-19 booster recommendations marks a watershed moment in the pandemic response. It reflects a nuanced understanding of risk, benefit, and evidence—and a commitment to restoring public trust in the regulatory process.
Makary and Prasad’s policy is not an indictment of vaccines. Rather, it is a call for precision, integrity, and accountability. As the pandemic enters a new phase, the FDA’s role must evolve from crisis management to thoughtful stewardship. That means asking hard questions, demanding rigorous data, and putting science—not politics—at the center of public health.