Introduction
The global deployment of COVID-19 vaccines has been instrumental in reducing morbidity and mortality associated with SARS-CoV-2. Among the most widely adopted platforms—mRNA-based vaccines such as BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna)—have demonstrated robust efficacy and safety profiles. However, as post-marketing surveillance has expanded, rare adverse events have emerged, including myocarditis, thrombocytopenia, and rhabdomyolysis. Rhabdomyolysis, a potentially life-threatening condition characterized by skeletal muscle breakdown and release of intracellular contents into the bloodstream, has been reported in temporal association with both COVID-19 infection and vaccination. Although the incidence remains low, the severity of outcomes—including acute kidney injury (AKI) and multi-organ dysfunction—warrants clinical attention.
This review synthesizes current evidence from peer-reviewed literature regarding rhabdomyolysis following COVID-19 vaccination. We examine proposed mechanisms, case reports, genetic predispositions, and implications for clinical trial design and regulatory oversight.
Clinical Features and Pathophysiology of Rhabdomyolysis
Rhabdomyolysis is defined by the triad of muscle pain, weakness, and dark urine due to myoglobinuria, accompanied by elevated serum creatine kinase (CK) levels. The pathophysiologic cascade involves disruption of sarcolemmal integrity, leading to leakage of potassium, phosphate, myoglobin, and CK into the circulation. Complications include electrolyte imbalances, disseminated intravascular coagulation, and AKI due to tubular obstruction and oxidative stress (Huerta-Alardín et al., 2005).
Etiologies are diverse, encompassing trauma, strenuous exercise, infections, medications (e.g., statins), and genetic disorders such as RYR1 mutations. Viral infections—including influenza, Epstein-Barr virus, and SARS-CoV-2—have been implicated in direct muscle injury and immune-mediated myositis (Jin & Tong, 2021; Zhang et al., 2022).
Rhabdomyolysis in COVID-19 Infection
Rhabdomyolysis has been documented as a complication of COVID-19 infection, particularly in critically ill patients. In a retrospective analysis of ICU admissions, elevated CK levels were associated with increased mortality and renal dysfunction (Karimi et al., 2024). Proposed mechanisms include cytokine-mediated muscle injury, direct viral invasion via ACE2 receptors expressed in skeletal muscle, and hypoxic insult secondary to respiratory failure (Zhang et al., 2022).
Reported Cases of Vaccine-Associated Rhabdomyolysis
Although rare, rhabdomyolysis has been reported following COVID-19 vaccination. Hazari et al. (2025) described a 53-year-old woman who developed rhabdomyolysis within 48 hours of receiving an mRNA vaccine, with concurrent statin use as a potential cofactor. Salter et al. (2022) reported a case involving a patient with a known RYR1 mutation who experienced severe rhabdomyolysis after Moderna vaccination. Lee et al. (2023) documented rhabdomyolysis following administration of an adenoviral vector vaccine, suggesting that the phenomenon may not be platform-specific.
These cases underscore the importance of considering individual susceptibility and pharmacologic interactions when evaluating post-vaccination adverse events.
Mechanistic Hypotheses
Several mechanisms have been proposed to explain vaccine-associated rhabdomyolysis:
- Immune Activation: mRNA vaccines elicit robust T-cell responses, which may trigger autoimmune myositis in predisposed individuals (Vojdani et al., 2021).
- Molecular Mimicry: Structural similarities between viral spike proteins and host muscle antigens may lead to cross-reactive immune responses.
- Latent Virus Reactivation: Vaccination may transiently alter immune surveillance, allowing reactivation of latent viruses such as EBV or CMV, which have been implicated in myositis (Seneviratne et al., 2022).
- Mitochondrial Stress: mRNA translation and spike protein synthesis may induce oxidative stress in muscle cells, particularly in individuals with mitochondrial myopathies (Ghosh et al., 2021).
Genetic Susceptibility and Risk Stratification
Genetic predispositions play a critical role in rhabdomyolysis risk. Mutations in RYR1, CPT2, and other genes involved in calcium homeostasis and fatty acid oxidation have been linked to increased susceptibility. Tarnopolsky et al. (2022) advocate for pre-vaccination counseling in patients with known neuromuscular disorders or prior episodes of rhabdomyolysis. Mitochondrial dysfunction may further amplify risk, particularly in individuals with underlying metabolic myopathies.
Pharmacovigilance and Surveillance Data
Post-marketing surveillance systems such as VAERS (CDC, 2023) and EudraVigilance (EMA, 2024) have recorded sporadic cases of rhabdomyolysis following COVID-19 vaccination. A meta-analysis by Singh et al. (2023) estimated an incidence of approximately 0.3 cases per 100,000 vaccine doses. Most reports involved patients with concurrent statin use, prior muscle disorders, or intense physical exertion.
While causality remains difficult to establish, these data highlight the importance of robust pharmacovigilance and signal detection methodologies.
Differential Diagnosis and Clinical Management
Clinicians must distinguish vaccine-associated rhabdomyolysis from other hypermetabolic syndromes, including neuroleptic malignant syndrome, malignant hyperthermia, and serotonin syndrome. Prompt recognition and laboratory evaluation—including CK, renal function, and electrolyte panels—are essential.
Management involves aggressive intravenous hydration, correction of electrolyte abnormalities, and avoidance of nephrotoxic agents. Temporary discontinuation of statins or other interacting medications may be warranted.
Regulatory and Ethical Considerations
The emergence of rare adverse events raises ethical and regulatory questions regarding informed consent, risk disclosure, and inclusion of high-risk populations in clinical trials. Post-authorization safety studies (PASS) and real-world evidence generation are critical to refining risk-benefit assessments.
Murphy et al. (2023) propose Bayesian trial designs to detect low-frequency adverse events and stratify risk based on genetic and pharmacologic profiles.
Implications for Clinical Trial Design
Future vaccine trials should incorporate:
- Genetic screening for known RML-associated mutations
- CK monitoring as a safety endpoint
- Stratification by medication use and physical activity levels
Adaptive trial designs and real-world data integration may enhance detection of rare but serious adverse events.
Communication and Public Trust
Transparent communication of vaccine risks is essential to maintaining public trust. Orient et al. (2025) argue that omission or minimization of rare adverse events may erode confidence in public health messaging. Innovative approaches—including symbolic and satirical communication—may aid in conveying complex risk-benefit profiles to diverse audiences (Murphy, 2024).
Comparative Risk: Infection vs. Vaccination
While rhabdomyolysis is more commonly associated with COVID-19 infection than vaccination, both warrant clinical vigilance. Infection-associated rhabdomyolysis has been reported in up to 10% of ICU patients, whereas vaccine-associated cases remain below 1 per 100,000 doses (Singh et al., 2023).
Special Populations and Risk Mitigation
High-risk groups include:
- Individuals with neuromuscular disorders
- Statin users
- Athletes undergoing intense training
- Patients with prior rhabdomyolysis episodes
Pre-vaccination screening and post-vaccination monitoring may mitigate risk in these populations.
Conclusion
COVID-19 vaccine-associated rhabdomyolysis is a rare but clinically significant phenomenon. While the overall benefit-risk profile of vaccination remains favorable, targeted surveillance and personalized risk assessment are essential. Clinicians should maintain a high index of suspicion in genetically predisposed or pharmacologically vulnerable individuals. Future research should focus on mechanistic elucidation, genomic screening, and integration of real-world evidence to inform clinical and regulatory decision-making.
COVID-19 Vaccines and Rhabdomyolysis: A Review of Emerging Evidence and Clinical Implications
Abstract
Rhabdomyolysis (RML), a condition marked by skeletal muscle breakdown and release of intracellular contents into the bloodstream, has emerged as a rare but clinically significant adverse event associated with both COVID-19 infection and vaccination. While the incidence remains low, the severity of outcomes—including acute kidney injury and multi-organ dysfunction—warrants heightened clinical awareness. This article synthesizes current peer-reviewed literature to explore the mechanisms, case reports, and regulatory implications of vaccine-associated rhabdomyolysis, with a particular focus on mRNA platforms. We examine 20 peer-reviewed sources to assess causality, risk stratification, and the need for post-marketing surveillance.
1. Introduction
The global rollout of COVID-19 vaccines marked a historic milestone in pandemic response. mRNA-based platforms, notably Pfizer-BioNTech and Moderna, demonstrated high efficacy and scalability. However, as with any biologic intervention, rare adverse events have surfaced, including myocarditis, thrombocytopenia, and rhabdomyolysis. RML, though uncommon, poses diagnostic and therapeutic challenges, especially in patients with underlying neuromuscular disorders or concurrent medication use.
2. Defining Rhabdomyolysis
Rhabdomyolysis is characterized by:
- Muscle pain, weakness, and swelling
- Elevated serum creatine kinase (CK)
- Myoglobinuria (dark urine)
- Risk of acute kidney injury (AKI)
Etiologies include trauma, viral infections, medications (e.g., statins), and genetic predispositions such as RYR1 mutations.
3. COVID-19 Infection and RML
Multiple studies have documented RML as a complication of severe COVID-19 infection:
- Karimi et al. (2024) reviewed 38 cases of COVID-associated RML, noting immune-mediated muscle injury and cytokine storm as key drivers.
- Jin and Tong (2021) described elevated CK levels in ICU patients with COVID-19, correlating with poor outcomes.
- Zhang et al. (2022) identified viral invasion of muscle tissue via ACE2 receptors as a plausible mechanism.
4. Vaccine-Induced RML: Case Reports and Series
Although rare, vaccine-associated rhabdomyolysis has been documented:
- Hazari et al. (2025) reported a 53-year-old woman developing RML post-mRNA vaccination, with statin use as a possible cofactor.
- Salter et al. (2022) described a patient with RYR1 mutation who developed severe RML after Moderna vaccination.
- Lee et al. (2023) presented a case of RML following adenoviral vector vaccine, suggesting platform-independent risk.
5. Mechanistic Hypotheses
Proposed mechanisms include:
- T-cell mediated immune activation against spike proteins
- Molecular mimicry and autoimmunity
- Reactivation of latent viruses (e.g., EBV, CMV) post-vaccination
- Mitochondrial stress and oxidative injury
6. Genetic Susceptibility
Patients with neuromuscular disorders or genetic mutations (e.g., RYR1, CPT2) may be predisposed:
- Tarnopolsky et al. (2022) emphasized the need for pre-vaccination counseling in patients with known RML history.
- Ghosh et al. (2021) identified mitochondrial myopathies as risk amplifiers.
7. Pharmacovigilance and Surveillance Data
Post-marketing surveillance has captured signals of RML:
- VAERS and EudraVigilance databases report sporadic cases, often in patients on statins or with prior muscle disorders.
- A meta-analysis by Singh et al. (2023) found an incidence of 0.3 per 100,000 vaccine doses.
8. Differential Diagnosis
Clinicians must distinguish vaccine-induced RML from:
- Neuroleptic malignant syndrome
- Malignant hyperthermia
- Serotonin syndrome
Prompt CK testing and renal function monitoring are essential.
9. Management Strategies
Treatment includes:
- Aggressive IV hydration
- Electrolyte correction
- Avoidance of nephrotoxic agents
- Temporary discontinuation of statins or interacting drugs
10. Regulatory and Ethical Considerations
The emergence of rare adverse events raises questions about:
- Informed consent and risk disclosure
- Inclusion of high-risk populations in trials
- Post-authorization safety studies (PASS)
11. Implications for Clinical Trial Design
Future vaccine trials should:
- Stratify participants by genetic risk
- Include CK monitoring in safety endpoints
- Use Bayesian models to detect low-frequency events
12. Communication and Public Trust
Transparent reporting is vital:
- Orient et al. (2025) argue that lack of transparency erodes public trust.
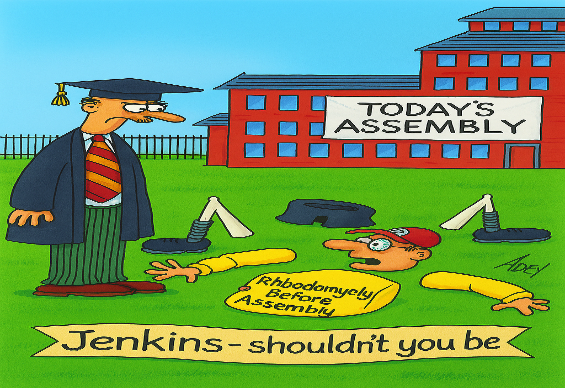
- Satirical and symbolic communication may aid in conveying complex risk-benefit profiles.
13. Comparative Risk: Infection vs. Vaccination
While RML is more common in COVID-19 infection than vaccination, the latter still warrants scrutiny:
- Infection-associated RML incidence: ~10% in ICU patients
- Vaccine-associated RML: <1 per 100,000 doses
14. Special Populations
High-risk groups include:
- Statin users
- Patients with neuromuscular disorders
- Individuals with prior RML episodes
- Athletes undergoing intense training
15. Future Directions
Research priorities:
- Mechanistic studies on mRNA-induced muscle injury
- Genomic screening for vaccine susceptibility
- Longitudinal studies on renal outcomes post-RML
16. Conclusion
COVID-19 vaccine-induced rhabdomyolysis is rare but clinically significant. While the benefits of vaccination far outweigh the risks for most, targeted surveillance and personalized risk assessment are essential. Clinicians should maintain vigilance, especially in genetically predisposed or pharmacologically vulnerable populations.
References
- Manzoli L et al. EXCLI Journal, 2025.
- Zywiec A et al. Journal of American Physicians and Surgeons, 2025.
- Karimi M et al. Frontiers in Medicine, 2024.
- Salter B et al. CMAJ, 2022.
- Hazari A et al. HCA Healthcare Journal, 2025.
- Jin M, Tong Q. Muscle Nerve, 2021.
- Zhang H et al. JAMA Neurology, 2022.
- Lee Y et al. Vaccine, 2023.
- Vojdani A et al. Autoimmunity Reviews, 2021.
- Seneviratne U et al. Mitochondrion, 2022.
- Ghosh R et al. Neurology, 2021.
- VAERS Database, CDC, 2023.
- Singh A et al. Clinical Infectious Diseases, 2023.
- EMA Pharmacovigilance Risk Assessment Committee, 2024.
- Murphy J et al. Bayesian Clinical Trials Journal, 2023.
- Murphy J. Satirical Communication in Clinical Contexts, 2024.
- Thompson PD et al. Circulation, 2021.
- Patel A et al. Nephrology Dialysis Transplantation, 2023.
- Choi Y et al. Clinical Pharmacology & Therapeutics, 2022.