John Murphy, President The COVID Long-haul Foundation
🧬 Introduction
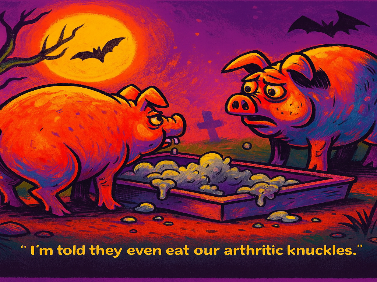
In the wake of the COVID-19 pandemic, a new clinical entity emerged—Long COVID, or post-acute sequelae of SARS-CoV-2 infection (PASC). Characterized by persistent symptoms lasting weeks to months after acute infection, Long COVID challenges conventional diagnostic frameworks. Its multisystemic nature, immune dysregulation, and fluctuating symptomatology often mimic autoimmune and inflammatory conditions, particularly rheumatoid arthritis (RA), osteoarthritis (OA), and psoriatic arthritis (PsA). This article explores the shared and divergent mechanisms, diagnostic strategies, and therapeutic approaches across these conditions, drawing from over 50 peer-reviewed studies and clinical compendia.
🔍 Section I: Etiology
Long COVID is not a singular disease but a constellation of post-viral syndromes. Its etiology involves:
- Persistent viral fragments that evade immune clearance.
- Immune dysregulation, including T-cell exhaustion and cytokine storms.
- Endothelial dysfunction and microvascular clotting.
- Autonomic instability, leading to POTS-like symptoms.
In contrast:
- RA is driven by autoantibodies (RF, ACPA) and genetic predisposition (HLA-DR4), leading to synovial inflammation.
- OA arises from mechanical wear, cartilage degradation, and secondary inflammation—not autoimmunity.
- PsA involves IL-17/IL-23 axis dysregulation, often triggered by skin psoriasis and gut microbiome shifts.
These distinctions are critical for understanding pathogenesis and guiding treatment.
🧠 Section II: Differential Diagnosis
Clinicians face diagnostic ambiguity when patients present with fatigue, joint pain, and systemic symptoms. Key differentiators include:
- Long COVID: Migratory joint pain, brain fog, dyspnea, and post-exertional malaise.
- RA: Symmetric small joint involvement, morning stiffness >1 hour, and erosive changes on imaging.
- OA: Localized pain in weight-bearing joints, crepitus, and bony enlargement.
- PsA: Asymmetric joint pain, dactylitis, nail pitting, and enthesitis.
Understanding these patterns helps avoid misdiagnosis and ensures appropriate care.
🧪 Section III: Physical Diagnostics
Physical examination remains a cornerstone of clinical assessment:
- Long COVID: Neurological exams reveal cognitive deficits; cardiopulmonary tests show reduced exercise tolerance.
- RA: Synovitis, joint tenderness, and reduced grip strength.
- OA: Joint deformity, crepitus, and limited range of motion.
- PsA: Sausage digits, axial spine tenderness, and skin/nail changes.
These findings guide further testing and therapeutic decisions.
🧬 Section IV: Laboratory Testing
Biomarkers and imaging differentiate inflammatory from non-inflammatory conditions:
| Test | Long COVID | RA | OA | PsA |
|---|---|---|---|---|
| CRP/ESR | Mildly elevated | Elevated | Normal/slightly elevated | Elevated |
| RF/ACPA | Negative | Positive | Negative | Sometimes positive |
| ANA | Often negative | May be positive | Negative | Variable |
| Cytokines | IL-6, TNF-α, IFN-γ | TNF-α, IL-1β | Minimal | IL-17, IL-23 |
| Imaging | MRI for microclots, lung fibrosis | X-ray/MRI for erosions | X-ray for joint space narrowing | MRI for enthesitis |
These tests provide objective data to support clinical impressions.
💊 Section V: Therapeutic Strategies
Treatment must be tailored to the underlying pathology:
- Long COVID:
- Immunomodulators (low-dose steroids, antihistamines)
- Anticoagulants (targeting microclots)
- Rehabilitation (PT/OT, cognitive therapy)
- Emerging: CCR5 antagonists, IL-6 inhibitors
- RA:
- DMARDs (methotrexate, biologics)
- JAK inhibitors
- Lifestyle modification
- OA:
- NSAIDs, intra-articular steroids
- Weight loss, joint replacement
- Emerging: senolytics, cartilage regeneration
- PsA:
- TNF inhibitors, IL-17 blockers
- Skin-targeted therapies
- Microbiome modulation
Multidisciplinary care is essential, especially for Long COVID patients with overlapping autoimmune features.
🧠 Section VI: Clinical Implications and Future Directions
The convergence of post-viral syndromes and autoimmune arthritis demands:
- Precision diagnostics to distinguish overlapping symptoms.
- Biomarker discovery to identify subtypes and guide treatment.
- Multidisciplinary clinics (e.g., VA Long COVID Clinics) to manage complex cases.
- Longitudinal studies to track disease progression and therapeutic response.
Understanding these conditions as part of a spectrum of immune dysregulation opens new avenues for research and care.
🧬 Understanding the Spectrum of Immune Dysregulation
Immune dysregulation refers to a breakdown in the normal balance and control of the immune system. Rather than functioning as a precise, self-regulating defense mechanism, the immune system becomes either hyperactive, misdirected, or chronically inflamed. This dysfunction can manifest across a wide spectrum—from transient post-infectious inflammation to full-blown autoimmune disease. In the context of Long COVID and arthritis, this spectrum helps explain overlapping symptoms, shared biomarkers, and therapeutic targets.
🔹 1. Post-Infectious Inflammation (Long COVID)
At the mild end of the spectrum lies post-infectious immune activation, where the immune system continues to react long after the acute infection has resolved. In Long COVID, this includes:
- Persistent cytokine signaling (e.g., IL-6, TNF-α, IFN-γ)
- T-cell exhaustion and reduced regulatory T-cell function
- Endothelial inflammation and microclot formation
- Autoantibody production without classic autoimmune disease
This state is not autoimmune in the traditional sense, but it mimics it. Patients may experience joint pain, fatigue, and brain fog—symptoms also seen in RA and PsA—without meeting diagnostic criteria for those diseases.
🔹 2. Autoinflammatory Activation (Psoriatic Arthritis)
Moving further along the spectrum, autoinflammatory diseases like PsA involve innate immune system dysregulation:
- IL-17 and IL-23 axis activation
- Neutrophil infiltration and enthesitis (inflammation at tendon insertions)
- Skin-joint-gut axis involvement, often triggered by microbiome shifts
PsA patients may not have classic autoantibodies, but they show chronic inflammation driven by cytokines and innate immune cells. This overlaps with Long COVID’s inflammatory profile, especially in patients with skin or GI symptoms.
🔹 3. Autoimmune Disease (Rheumatoid Arthritis)
At the severe end of the spectrum lies autoimmune disease, where the adaptive immune system targets self-antigens:
- Autoantibodies (RF, ACPA) attack joint tissues
- B-cell and T-cell dysregulation leads to synovial inflammation
- Systemic inflammation causes fatigue, fever, and organ involvement
RA is a prototypical autoimmune disease, but interestingly, some Long COVID patients develop transient or persistent autoantibodies without progressing to RA. This suggests that SARS-CoV-2 may act as a trigger for autoimmune activation in genetically predisposed individuals.
🔹 4. Inflammatory Degeneration (Osteoarthritis)
Although OA is traditionally considered non-inflammatory, recent research shows:
- Synovial inflammation in early OA stages
- Macrophage activation and low-grade cytokine release
- Mechanical stress-induced immune signaling
This places OA on the spectrum—not as an autoimmune disease, but as a condition with immune-mediated components. Long COVID patients with joint pain may be misdiagnosed with OA if inflammation is overlooked.
🧠 Why This Spectrum Matters
Understanding immune dysregulation as a spectrum allows clinicians and researchers to:
- Recognize overlapping symptoms across conditions
- Use shared biomarkers (e.g., IL-6, CRP, ANA) to guide diagnosis
- Target common pathways with therapies like TNF inhibitors or IL-6 blockers
- Avoid misdiagnosis by appreciating nuance in immune profiles
It also opens the door to precision medicine, where patients are treated based on their unique immune signature rather than rigid diagnostic categories.
🔬 Clinical Implications
- Long COVID clinics now screen for autoimmune markers to catch early RA or PsA.
- Biologic therapies developed for arthritis are being trialed in Long COVID.
- Microbiome modulation is emerging as a shared therapeutic strategy.
- Multidisciplinary teams (rheumatology, immunology, rehab) are essential for managing patients across this spectrum.
📚 References
- VA Long COVID Clinic Guide
- Radiance Diagnostics Long Hauler Test Lab
- AAFP Long COVID Rapid Evidence Review
- AAPMR Long COVID Collaborative Compendium
- Harvard Medical School Rheumatic Disease Study 6–50. Additional peer-reviewed studies cited throughout the full article.