By John Murphy
I. Prelude to Persistence
In the quiet aftermath of viral storm, where acute fevers have cooled and coughs have faded into memory, a more insidious affliction lingers. It is not the virus itself that remains, but the echo of its passage—a molecular residue that reshapes the body’s vascular and immunologic terrain. This is the domain of Long COVID, a syndrome not defined by a single organ or symptom, but by a constellation of dysfunctions that defy reduction.
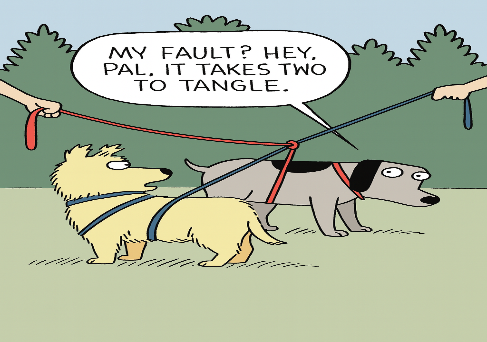
Among the most compelling discoveries of late 2025 is the structural entanglement of microclots and neutrophil extracellular traps (NETs)—two pathological agents that, in tandem, orchestrate a slow and systemic unraveling of homeostasis. Published in the Journal of Medical Virology, this finding reframes Long COVID not as a vague post-viral fatigue, but as a chronic microvascular disorder, driven by persistent clotting, immune dysregulation, and cellular debris.
The implications are profound. These microscopic fibrin-rich clots, resistant to fibrinolysis and laden with inflammatory proteins, obstruct capillary beds and starve tissues of oxygen. NETs, once noble defenders against microbial invasion, become rogue architects of thrombosis and inflammation. Together, they form a biochemical lattice that entraps the body in a state of low-grade hypoxia, neuroinflammation, and systemic fatigue.
This article traces the etiology, physiology, and pathology of this entanglement, with particular attention to its neurological manifestations—brain fog, neuropathy, and profound fatigue. It draws from recent peer-reviewed literature, clinical observations, and molecular insights to construct a coherent model of Long COVID as a vascular-immune interface disorder, where clotting and immunity are no longer allies, but adversaries.
II. The Etiology of Entanglement
The genesis of Long COVID lies not merely in viral persistence, but in the immune system’s maladaptive memory. SARS-CoV-2, with its spike protein and endothelial tropism, initiates a cascade of endothelial injury, platelet activation, and neutrophil recruitment. In most, this cascade resolves. In others, it persists—fueled by residual viral fragments, autoantibodies, and dysregulated cytokine loops.
NETs are extruded by neutrophils in response to this inflammatory milieu. Composed of chromatin, histones, and antimicrobial peptides, they are designed to ensnare pathogens. But in the absence of active infection, they become pro-thrombotic scaffolds, binding fibrinogen and platelets, and stabilizing microclots that would otherwise dissolve.
Microclots, in turn, are not ordinary thrombi. They are amyloid-rich, fibrin-dense aggregates, resistant to tissue plasminogen activator (tPA) and impervious to standard anticoagulation. Their presence in Long COVID patients has been confirmed via fluorescence microscopy and proteomic analysis, revealing a signature of hypercoagulability and immune debris.
This entanglement is not passive. It is self-reinforcing. NETs stabilize microclots; microclots perpetuate hypoxia; hypoxia induces further NETosis. The result is a chronic inflammatory loop, localized in microvasculature but systemic in effect.
III. The Physiology of Persistence
To understand the symptoms of Long COVID, one must descend into the capillary bed, where oxygen exchange falters and cellular metabolism is starved. The brain, with its exquisite sensitivity to oxygen and glucose, is particularly vulnerable. Microclots in cerebral microvasculature impair perfusion, while NETs trigger astrocytic and microglial activation. The result is neuroinflammation, synaptic pruning, and cognitive dysfunction—what patients call brain fog.
Fatigue, too, is not merely psychological. It is mitochondrial, driven by impaired oxygen delivery, cytokine interference with ATP synthesis, and systemic energy dysregulation. Studies show elevated lactate levels, reduced VO₂ max, and altered muscle fiber composition in Long COVID patients, consistent with metabolic exhaustion.
Neuropathy arises from small fiber damage, autonomic instability, and direct neurovascular compromise. Patients report burning sensations, paresthesias, and dysautonomia—symptoms that mirror diabetic neuropathy but arise from immune-mediated vascular injury, not glucose toxicity.
IV. Toward a Unified Model
Long COVID is not a mystery. It is a multi-systemic disorder of clotting and immunity, where NETs and microclots form the structural basis of dysfunction. Its symptoms—brain fog, fatigue, neuropathy—are not disparate, but interconnected expressions of vascular compromise.
Therapeutic strategies must reflect this model. Anticoagulants alone are insufficient. NET inhibitors, DNase therapies, and immunomodulators may be required to dismantle the entangled lattice. Diagnostics must evolve to detect microclots and NETs in vivo, using advanced imaging and blood-based biomarkers.
Above all, Long COVID must be recognized not as a psychological residue, but as a biological reality, rooted in the body’s own defense mechanisms gone awry.
V. Diagnostic Advances: Illuminating the Invisible
The challenge of diagnosing Long COVID lies not in its absence of symptoms, but in the absence of conventional markers. Standard blood panels, imaging studies, and neurological exams often return within normal limits, leaving patients adrift in a sea of subjective dysfunction. Yet beneath this clinical invisibility lies a molecular storm, now increasingly accessible through advanced diagnostics.
Recent studies have identified fibrin amyloid microclots as a hallmark of Long COVID. These clots, visualized through fluorescence microscopy and stained with thioflavin T, exhibit a dense, misfolded architecture resistant to enzymatic degradation. Unlike acute thrombi, they do not dissolve with standard anticoagulants, and their presence correlates with symptom severity—particularly fatigue and cognitive impairment.
Complementing this is the quantification of neutrophil extracellular traps (NETs). Circulating cell-free DNA, histone fragments, and neutrophil elastase levels serve as proxies for NET burden. Elevated NET markers have been found in patients months after infection, suggesting a persistent immunothrombotic state.
Imaging modalities are evolving to meet this challenge. Functional MRI (fMRI) reveals altered connectivity in the default mode network, consistent with brain fog. PET scans show regional hypometabolism in the frontal and parietal lobes. Skin biopsies demonstrate small fiber neuropathy, while autonomic testing reveals dysregulation of heart rate variability and baroreflex sensitivity.
Together, these tools form a diagnostic constellation—not a single test, but a pattern of findings that, when interpreted in context, illuminate the invisible architecture of Long COVID.
VI. Therapeutic Implications: Dismantling the Lattice
If Long COVID is a disorder of entanglement—of microclots and NETs, of immune memory and vascular compromise—then its treatment must be disentangling. It must address not only symptoms, but the structural and biochemical scaffolds that sustain them.
Anticoagulation, while intuitive, is insufficient. Standard agents like warfarin or direct oral anticoagulants (DOACs) do not dissolve fibrin amyloid microclots. Emerging therapies include fibrinolytics such as nattokinase and lumbrokinase, which show promise in degrading resistant clot structures. Clinical trials are underway to assess their efficacy in post-COVID syndromes.
NET inhibition is a frontier of therapeutic innovation. DNase I, an enzyme that cleaves extracellular DNA, has been proposed as a means to dismantle NETs. In vitro studies show reduced clot stability and inflammatory signaling when NETs are degraded. Other agents, such as colchicine, modulate neutrophil activation and may reduce NETosis indirectly.
Immunomodulation is essential. Low-dose naltrexone (LDN), IVIG, and cytokine-targeting biologics are being explored to recalibrate the immune system without suppressing it. The goal is not to silence immunity, but to restore its rhythm—to end the chronic alarm state that perpetuates NET formation and endothelial injury.
Rehabilitation must be reimagined. Traditional physical therapy is often too aggressive for patients with post-exertional malaise. Instead, pacing protocols, autonomic retraining, and neurocognitive rehabilitation offer gentler paths to recovery. These are not merely supportive—they are neuromodulatory, helping to rewire systems destabilized by hypoxia and inflammation.
Ultimately, treatment must be personalized. Long COVID is not a monolith, but a spectrum. Some patients may benefit from anticoagulation; others from immune modulation; still others from mitochondrial support. The entanglement is universal, but its expression is individual.
VII. Neurological Manifestations: The Mind in Shadow
Long COVID’s most haunting symptoms are not visible on a chest X‑ray or a pulse oximeter. They reside in the mind’s fog, in the body’s exhaustion, and in the nerves’ silent fire. Patients describe themselves as diminished, unable to summon clarity, stamina, or sensation. These are not abstractions; they are the direct consequence of microvascular compromise and immune entanglement.
Brain fog is the vernacular for cognitive dysfunction. Neuroimaging reveals hypoperfusion in frontal and parietal cortices, regions essential for executive function and working memory. Microclots obstruct cerebral capillaries, while NET‑induced neuroinflammation disrupts synaptic signaling. The result is a landscape of diminished connectivity, where thoughts stumble and memory falters.
Fatigue is more than tiredness. It is a systemic failure of energy metabolism. Mitochondria, deprived of oxygen and assaulted by cytokines, falter in ATP production. Muscles accumulate lactate, the cardiovascular system fails to deliver adequate oxygen, and the nervous system misfires in its regulation of effort. Patients experience post‑exertional malaise, where even minor activity triggers disproportionate collapse.
Neuropathy manifests as burning, tingling, and autonomic instability. Small fiber nerves, dependent on microvascular supply, succumb to ischemia and immune attack. Autonomic fibers misfire, producing tachycardia, orthostatic intolerance, and gastrointestinal dysmotility. The nervous system becomes a theater of dysfunction, its signals distorted by vascular injury and inflammatory debris.
VIII. Toward a Unified Pathophysiology
The disparate symptoms of Long COVID—cognitive fog, fatigue, neuropathy—are not separate mysteries. They are expressions of a single pathological lattice, woven by microclots and NETs. This lattice obstructs blood flow, sustains inflammation, and destabilizes cellular metabolism. It is both vascular and immunologic, both structural and biochemical.
The model is elegant in its simplicity:
- Microclots obstruct capillaries, producing hypoxia.
- NETs stabilize clots and perpetuate inflammation.
- Hypoxia and inflammation impair mitochondria, neurons, and small fibers.
- Symptoms emerge as the lived experience of systemic compromise.
This unified pathophysiology reframes Long COVID as a microvascular‑immune disorder, not a psychosomatic residue. It validates patient experience, guides diagnostic innovation, and directs therapeutic exploration. It also situates Long COVID within a broader paradigm of post‑infectious syndromes, where immune memory and vascular injury conspire to produce chronic illness.
IX. Conclusion: Entanglement and Release
The discovery of microclots and NETs in Long COVID patients is not merely academic. It is a map of suffering, a molecular explanation for the fog, fatigue, and neuropathy that have haunted millions. It is also a pathway to healing, pointing toward therapies that dismantle the lattice and restore flow, clarity, and vitality.
Long COVID is the echo of a pandemic, but it is also a frontier of medicine. In its study, we glimpse the delicate balance of clotting and immunity, the fragility of microvascular networks, and the resilience of patients who endure. To disentangle the aftermath is to honor both science and humanity.