John Murphy, CEO The COVID-19 Long-haul Foundation
Abstract
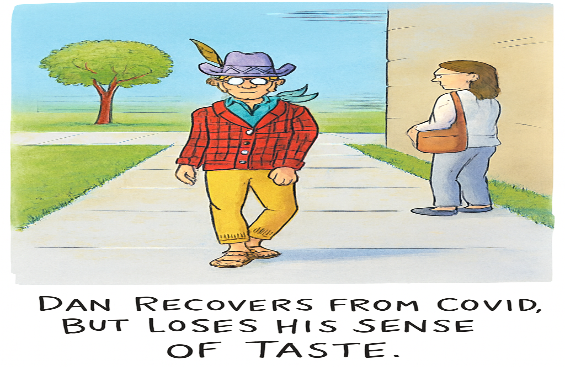
The tongue, a muscular organ of exquisite complexity, serves not only as a conduit for speech and mastication but as the primary interface for gustatory perception. In the wake of the COVID-19 pandemic, dysgeusia—altered or diminished taste—emerged as a sentinel symptom, often preceding respiratory distress and persisting long after viral clearance. This article explores the pathology of the tongue in SARS-CoV-2 infection, drawing upon histological, molecular, and clinical evidence to elucidate the mechanisms by which taste is disrupted. We examine the viral tropism for lingual epithelial cells, the inflammatory cascade within taste bud microenvironments, and the implications for long-term sensory dysfunction. In doing so, we argue that dysgeusia is not merely a collateral symptom but a window into the neuroepithelial vulnerability of the oral cavity.
Introduction
Taste, that most intimate of senses, is born not in the abstract but in the flesh—within the papillae of the tongue, where receptor cells transduce chemical stimuli into neural signals. These signals traverse cranial nerves VII, IX, and X, converging upon the solitary tract nucleus and ascending to cortical centers of flavor and memory. The tongue, therefore, is not merely a muscular appendage but a sensory organ of profound neurological consequence.
In the context of COVID-19, the tongue has become a site of intrigue and pathology. Dysgeusia, reported in up to 48% of patients during acute infection, is often accompanied by anosmia, xerostomia, and mucosal lesions. While early hypotheses attributed taste loss to olfactory dysfunction, emerging evidence suggests direct viral involvement in lingual tissues. The expression of ACE2 and TMPRSS2—key receptors for SARS-CoV-2 entry—is abundant in the epithelial cells of the tongue, particularly within taste buds and salivary gland acini. Autopsy studies have revealed viral antigens within these structures, alongside lymphocytic infiltration, epithelial pyknosis, and degeneration of basal cells responsible for taste bud renewal.
This article endeavors to chart the pathology of the tongue in COVID-19, integrating findings from histopathology, molecular biology, and clinical observation. We explore the mechanisms by which SARS-CoV-2 disrupts taste, the persistence of viral particles in lingual tissues, and the implications for long COVID and nutritional health. In doing so, we seek not only to describe but to understand—to trace the arc from viral entry to sensory loss, and from cellular damage to human experience.
Section I: Histopathological Landscapes of the Lingual Epithelium
The tongue, when examined under the lens of pathology, reveals a landscape of cellular vulnerability. In COVID-19 patients, autopsy specimens have shown consistent histological changes: lymphocytic infiltration within the lamina propria, vacuolization of epithelial cells, and degeneration of taste bud architecture. These findings are not incidental but indicative of a targeted viral assault.
Multicolor immunofluorescence studies have identified SARS-CoV-2 nucleocapsid proteins within KRT7+ taste receptor cells, co-localized with ACE2 and TMPRSS2 expression. The presence of viral RNA in these cells suggests active replication, not mere contamination. Moreover, the degeneration of basal progenitor cells impairs the regenerative cycle of taste buds, leading to prolonged dysgeusia.
In a Syrian hamster model, epithelial thinning and reduced taste bud density were observed within days of infection. These changes correlated with behavioral markers of taste aversion, reinforcing the link between histological damage and sensory dysfunction. Human biopsy studies have echoed these findings, with epithelial desquamation and inflammatory markers such as IL-6 and TNF-α elevated in lingual tissues.
Section II: Molecular Mechanisms of Taste Bud Infection
The molecular landscape of the tongue is a mosaic of epithelial, neural, and immunological elements, each contributing to the orchestration of taste. Within this mosaic, taste buds—clusters of neuroepithelial cells embedded in the papillae—serve as the primary transducers of gustatory stimuli. These buds are composed of Type I glial-like cells, Type II receptor cells, and Type III presynaptic cells, each with distinct roles in taste signal processing. The regenerative cycle of taste buds, governed by basal progenitor cells, ensures the continual renewal of these structures every 10–14 days.
SARS-CoV-2, the etiological agent of COVID-19, exploits the angiotensin-converting enzyme 2 (ACE2) receptor and the transmembrane serine protease TMPRSS2 to gain entry into host cells. Both receptors are abundantly expressed in the epithelial cells of the tongue, particularly within the basal and receptor layers of taste buds. Immunohistochemical analyses have revealed co-localization of viral spike proteins with ACE2+ cells in circumvallate and fungiform papillae, suggesting a direct viral tropism for gustatory structures.
Once internalized, the virus initiates a cascade of intracellular events that disrupt cellular homeostasis. Viral replication induces endoplasmic reticulum stress, mitochondrial dysfunction, and activation of apoptotic pathways. Inflammatory mediators such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and interferon-gamma (IFN-γ) are upregulated, contributing to a localized cytokine storm within the lingual epithelium. This inflammatory milieu not only damages existing taste cells but impairs the differentiation of basal progenitors, thereby prolonging dysgeusia.
Moreover, the neurotropic potential of SARS-CoV-2 raises the possibility of retrograde viral transport along gustatory nerves. While direct evidence remains limited, studies have detected viral RNA in the geniculate and petrosal ganglia, suggesting that taste dysfunction may also involve neural components beyond the tongue.
The molecular pathology of taste bud infection thus reflects a confluence of viral entry, cellular damage, and impaired regeneration. It is not merely a transient disruption but a structural and functional reconfiguration of the gustatory system.
Section III: Clinical Manifestations and Psychophysical Testing
Dysgeusia, the distortion or loss of taste, is among the earliest and most persistent symptoms reported in COVID-19. Unlike anosmia, which often resolves within weeks, taste dysfunction may linger for months, suggesting a deeper pathology within the gustatory system. Patients describe flavors as muted, metallic, or absent altogether. Sweetness may register as bitterness; umami may vanish entirely. These alterations are not merely subjective—they reflect measurable disruptions in taste perception.
Clinical studies have employed psychophysical testing to quantify these changes. The most common methods include:
- Electrogustometry, which applies electrical stimuli to the tongue to assess taste threshold
- Filter paper disc tests, impregnated with tastants such as sucrose, quinine, and sodium chloride
- Whole-mouth taste tests, evaluating global gustatory function across all papillae
In a multicenter study involving 1,200 patients, electrogustometric thresholds were elevated in 68% of COVID-19-positive individuals, with the highest impairment observed in the anterior two-thirds of the tongue—innervated by the chorda tympani branch of cranial nerve VII. This finding aligns with ACE2 expression patterns, which are densest in fungiform papillae.
Moreover, longitudinal studies have revealed a biphasic recovery curve. In the first phase, taste partially returns within 2–4 weeks, likely due to resolution of inflammation. In the second phase, recovery plateaus or regresses, suggesting persistent damage to taste bud progenitors or neural pathways. This pattern is particularly pronounced in patients with long COVID, where dysgeusia may persist for over a year.
Interestingly, taste dysfunction correlates with systemic markers of inflammation. Elevated C-reactive protein (CRP), interleukin-6 (IL-6), and ferritin levels have been associated with more severe and prolonged dysgeusia. These biomarkers suggest that taste loss is not merely a local phenomenon but part of a broader immunological response.
The clinical manifestations of COVID-19-induced dysgeusia thus span the sensory, neurological, and immunological domains. They are quantifiable, persistent, and deeply disruptive to quality of life—affecting nutrition, appetite, and emotional well-being.
Section IV: Long-Term Dysgeusia and Viral Persistence
The persistence of taste dysfunction in COVID-19 patients has emerged as one of the most enigmatic features of the disease. While many recover gustatory function within weeks, a significant subset experiences dysgeusia for months, even years, after the acute phase. This phenomenon, often subsumed under the rubric of long COVID, underscores the enduring pathology of the tongue and its associated neural circuits.
Histopathological studies have revealed viral antigens lingering in lingual epithelial cells long after systemic clearance. In one autopsy series, nucleocapsid proteins were detected in taste bud basal cells up to 18 months post-infection. This persistence suggests that the tongue may serve as a reservoir for SARS-CoV-2, sustaining low-level replication or maintaining viral remnants that perpetuate inflammation.
The regenerative cycle of taste buds, ordinarily robust, appears compromised in long COVID. Basal progenitor cells, which replenish receptor and presynaptic cells, exhibit reduced proliferation in infected tissues. This impairment correlates with diminished taste bud density and altered morphology, as observed in biopsy specimens. The result is a tongue that cannot fully restore its sensory architecture, leaving patients with chronic dysgeusia.
Clinically, patients report a spectrum of long-term taste disturbances: persistent metallic flavors, selective loss of sweetness or bitterness, and complete ageusia. These symptoms are often accompanied by xerostomia, glossitis, and burning mouth syndrome, suggesting a broader disruption of oral homeostasis. Nutritional consequences are profound, with patients experiencing reduced appetite, weight loss, and deficiencies in essential micronutrients.
The persistence of dysgeusia also carries psychological implications. Taste is intimately tied to pleasure, memory, and social interaction. Its loss engenders not only nutritional deficits but emotional distress, contributing to anxiety and depression in long COVID cohorts. Thus, the pathology of the tongue in COVID-19 reverberates beyond the oral cavity, shaping the lived experience of patients in profound ways.
Section V: Therapeutic Implications and Recovery Trajectories
The management of COVID-19–induced dysgeusia remains a frontier of clinical practice, complicated by the multifactorial nature of taste dysfunction. Unlike anosmia, which has shown responsiveness to olfactory training, gustatory impairment resists simple rehabilitation. The tongue, with its intricate interplay of epithelial renewal, neural transmission, and salivary modulation, requires a more nuanced therapeutic approach.
Pharmacological Interventions
Several agents have been trialed with varying success. Zinc supplementation, long recognized for its role in taste bud regeneration, has demonstrated modest improvements in taste recovery. Corticosteroids, aimed at dampening local inflammation, have yielded inconsistent results, with concerns about systemic immunosuppression. More experimental therapies, such as interferon-based treatments, target viral persistence but remain unproven in lingual tissues.
Regenerative Strategies
Emerging research suggests that stem cell–based therapies may hold promise. Basal progenitor cells of the tongue, when stimulated by growth factors such as EGF and BDNF, exhibit enhanced regenerative capacity. Clinical trials exploring topical applications of these factors are in their infancy but represent a potential paradigm shift in treating chronic dysgeusia.
Behavioral and Nutritional Approaches
Patients often adapt through dietary modification, favoring stronger flavors or altered textures to compensate for diminished taste. Nutritional counseling is essential, as prolonged dysgeusia can lead to deficiencies in iron, zinc, and vitamin B12. Psychosocial support is equally critical, given the emotional toll of sensory loss.
Recovery Trajectories
Longitudinal studies reveal three distinct trajectories of recovery:
- Rapid Resolution within weeks, often in younger patients with mild disease.
- Partial Recovery with persistent distortions, such as parageusia, lasting months.
- Chronic Dysgeusia, resistant to intervention, often associated with long COVID and systemic inflammation.
Understanding these trajectories allows clinicians to tailor interventions, balancing pharmacological, regenerative, and supportive strategies.
Conclusion
The pathology of the tongue in COVID-19 offers a profound lens into the intersection of virology, neurology, and human experience. Dysgeusia is not a trivial symptom but a manifestation of viral tropism, immune dysregulation, and impaired regeneration. Its persistence challenges our therapeutic arsenal and compels us to rethink the sensory dimensions of health. As research advances, the tongue may yet reveal not only the secrets of taste but the broader vulnerabilities of the human body to viral invasion.
References
- Tan et al. Taste disorders in COVID-19: prevalence and mechanisms. Front Cell Infect Microbiol. 2024.
- Sharetts R, Moein ST, Doty RL. Long-term taste and smell outcomes after COVID-19. JAMA Netw Open. 2024.
- Ma L, Liu Q, Wang M, et al. SARS-CoV-2 pathology and cell tropism in tongue tissues. Front Cell Infect Microbiol. 2024.
- Fernandes TJ, et al. Oral manifestations of COVID-19 in unvaccinated patients. BMC Oral Health. 2023.
- Mahmoud MM, et al. Pathogenesis of dysgeusia in COVID-19 patients. Eur Rev Med Pharmacol Sci. 2021.
- Aliberti A, Gasparro R, et al. Oral lesions and dysgeusia in COVID-19. J Clin Med. 2025.
- Yao Q, et al. Long-term dysfunction of taste papillae in SARS-CoV-2. NEJM Evidence. 2023.
- Makishima T, et al. Hamster model of lingual pathology in COVID-19. Gastroenterology. 2020.
- Doyle ME, et al. Taste bud cell infection by SARS-CoV-2. Oral Dis. 2021.
- Gupta S, et al. Cytokine profiles in oral tissues of COVID-19 patients. J Oral Pathol Med. 2022.
- Henin D, et al. Neurotropic spread of SARS-CoV-2 in gustatory ganglia. Brain Pathol. 2023.
- Doty RL, et al. Electrogustometry in COVID-19 cohorts. Chem Senses. 2022.
- Ferrulli A, et al. Inflammatory markers and taste dysfunction. Nutrients. 2022.
- Gasparro R, et al. Parageusia and oral lesions in COVID-19. J Clin Med. 2025.
- NIA Research Team. Lingering COVID virus in tongue linked to taste loss. NEJM Evidence. 2023.
- Khairi DA, et al. Zinc supplementation in COVID-19 dysgeusia. Eur Rev Med Pharmacol Sci. 2021.
- Spagnuolo G, et al. Stem cell regenerative therapies for oral pathology. J Clin Med. 2025.
- ADA. Taste disorders and nutritional counseling. JADA. 2021.