Determining the duration of protective immunity to infection by SARS-CoV-2 is crucial for understanding and predicting the course of the COVID-19 pandemic. Clinical studies now indicate that immunity will be long-lasting.
Authors: Andreas Radbruch & Hyun-Dong Chang
Generating immunity against the SARS-CoV-2 coronavirus is of the utmost importance for bringing the COVID-19 pandemic under control, protecting vulnerable individuals from severe disease and limiting viral spread. Our immune systems protect against SARS-CoV-2 either through a sophisticated reaction to infection or in response to vaccination. A key question is, how long does this immunity last? Writing in Nature, Turner et al.1 and Wang et al.2 characterize human immune responses to SARS-CoV-2 infection over the course of a year.
There is ongoing discussion about which aspects of the immune response to SARS-CoV-2 provide hallmarks of immunity (in other words, correlates of immunological protection). However, there is probably a consensus that the two main pillars of an antiviral response are immune cells called cytotoxic T cells, which can selectively eliminate infected cells, and neutralizing antibodies, a type of antibody that prevents a virus from infecting cells, and that is secreted by immune cells called plasma cells. A third pillar of an effective immune response would be the generation of T helper cells, which are specific for the virus and coordinate the immune reaction. Crucially, these latter cells are required for generating immunological memory — in particular, for orchestrating the emergence of long-lived plasma cells3, which continue to secrete antiviral antibodies even when the virus has gone.
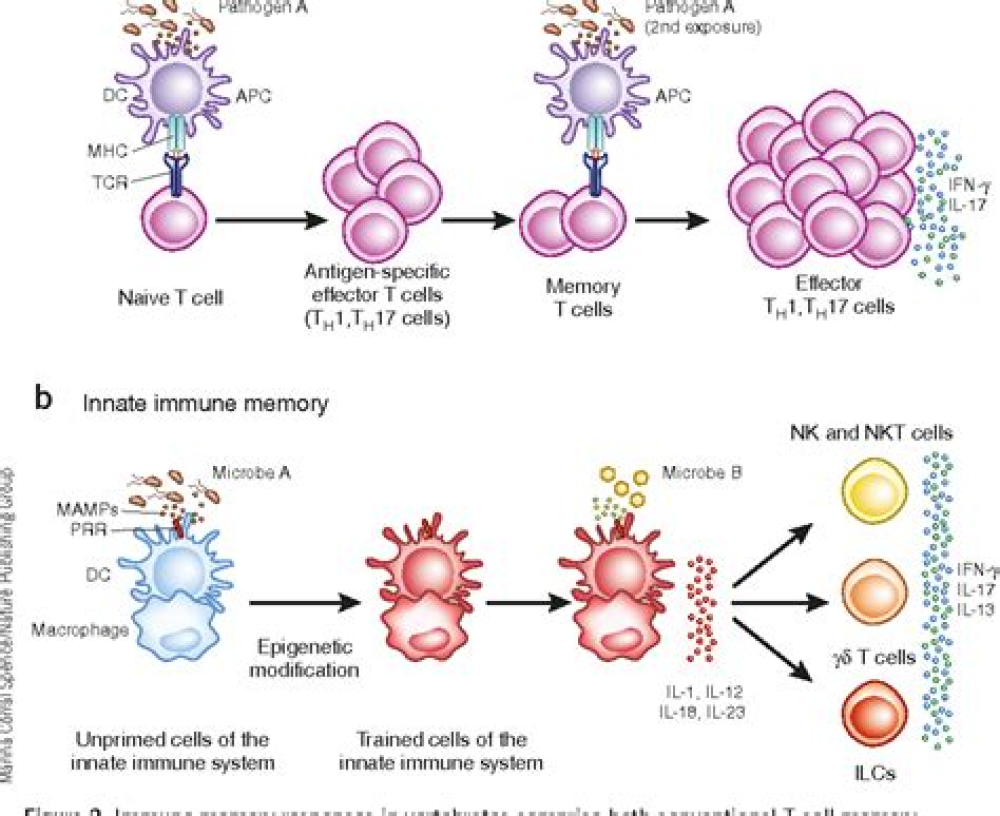
Immunological memory is not a long-lasting version of the immediate immune reaction to a particular virus; rather, it is a distinct aspect of the immune system. In the memory phase of an immune response, B and T cells that are specific for a virus are maintained in a state of dormancy, but are poised to spring into action if they encounter the virus again or a vaccine that represents it. These memory B and T cells arise from cells activated in the initial immune reaction. The cells undergo changes to their chromosomal DNA, termed epigenetic modifications, that enable them to react rapidly to subsequent signs of infection and drive responses geared to eliminating the disease-causing agent4. B cells have a dual role in immunity: they produce antibodies that can recognize viral proteins, and they can present parts of these proteins to specific T cells or develop into plasma cells that secrete antibodies in large quantities. About 25 years ago5, it became evident that plasma cells can become memory cells themselves, and can secrete antibodies for long-lasting protection. Memory plasma cells can be maintained for decades, if not a lifetime, in the bone marrow6.
The presence in the bone marrow of long-lived, antibody-secreting memory plasma cells is probably the best available predictor of long-lasting immunity. For SARS-CoV-2, most studies so far have analyzed the acute phase of the immune response, which spans a few months after infection, and have monitored T cells, B cells and secreted antibodies7. It has remained unclear whether the response generates long-lived memory plasma cells that secrete antibodies against SARS-CoV-2.
For More Information: https://www.nature.com/articles/d41586-021-01557-z