Authors: Hasan K. Siddiqi,a,bPeter Libby,a,⁎ and Paul M Ridkera,b
Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) leads to multi-system dysfunction with emerging evidence suggesting that SARS-CoV-2-mediated endothelial injury is an important effector of the virus. Potential therapies that address vascular system dysfunction and its sequelae may have an important role in treating SARS-CoV-2 infection and its long-lasting effects.
SARS-CoV-2 infection and vascular dysfunction
In health, the vascular endothelium maintains homeostasis through regulation of immune competence, inflammatory equilibrium, tight junctional barriers, hemodynamic stability as well as optimally balanced thrombotic and fibrinolytic pathways. In the novel coronavirus disease of 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), dysregulation of many of these pathways has emerged as a mediator of severe disease. The constellation of clinical and biomarker derangements seen in COVID-19 can be classified into disruption of the immune, renin-angiotensin-aldosterone (RAA), and thrombotic balance, all of which converge on the vascular endothelium as a common pathway. Accumulating evidence from basic science, imaging and clinical observations, has clarified the picture of COVID-19 as a vascular disease. Understanding the disease in this context may provide novel avenues of understanding COVID-19 and lead to critically needed improvements in therapeutic strategies.
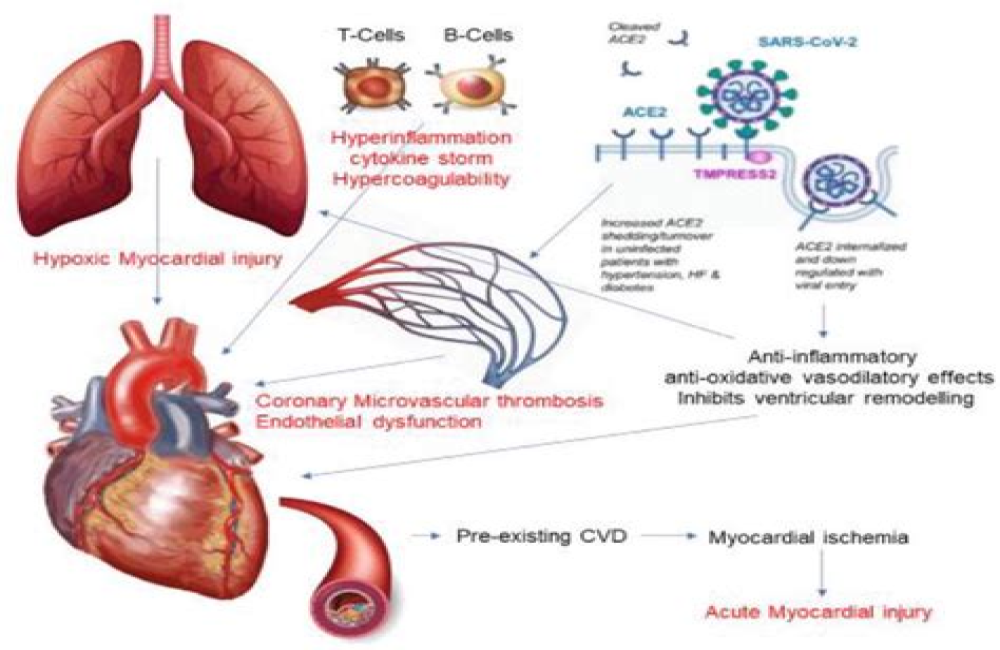
SARS-CoV-2 uses the angiotensin converting enzyme 2 (ACE2) to facilitate entry into target cells and initiate infection. This viral entry into the cell is further mediated by transmembrane serine protease 2 (TMPRSS2) and cathepsin L which cleave the S protein on the viral particle to permit engagement with ACE2 [1]. Endothelial cells (ECs) in general and cardiac pericytes in particular express abundant ACE2, making them a direct target of SARS-CoV-2 infection (Fig. 1 ) [2]. Examination of the pulmonary vascular bed shows severe derangements in COVID-19, compared to control and influenza patients, particularly with widespread thrombosis and microangiopathy, endothelial activation and extensive angiogenesis [3]. These studies and pervasive findings establish the role of viral injury to the vascular system with resulting vascular dysfunction in COVID-19 patients [4].

Open in a separate windowFig. 1
SARS-CoV-2 Induced Endothelial Injury
Legend: A schematic of SARS-CoV-2 infection and proposed resulting endothelial injury, involving immune activation, pro-thrombotic milieu, and RAAS dysregulation. These insults interact with each other to cause end-organ dysfunction that is manifest in many COVID-19 patients.
TMPRSS2 = Transmembrane protease serine 2; ADAM17 = A disintegrin and metalloproteinase 17; TNF = Tumor necrosis factor; TNFr = Tumor necrosis factor receptor; TLR = toll-like receptor; DAMPs = Damage-associated molecular patterns; PAMPs = Pathogen-associated molecular patterns; PAI-1 = plasminogen activator inhibitor-1; vWF = von Willebrand factor; eNOS = endothelial nitric oxide; tPA = tissue plasminogen activator; AT1R = angiotensin 1 receptor; ARDS = acute respiratory distress syndrome.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7556303/