- Authors: Min Gao, MSc *, Carmen Piernas, PhD , Nerys M Astbury, PhD, Prof Julia Hippisley-Cox, FRCPProf Stephen O’Rahilly, FRS, Prof Paul Aveyard, FRCGP †
Summary
Background
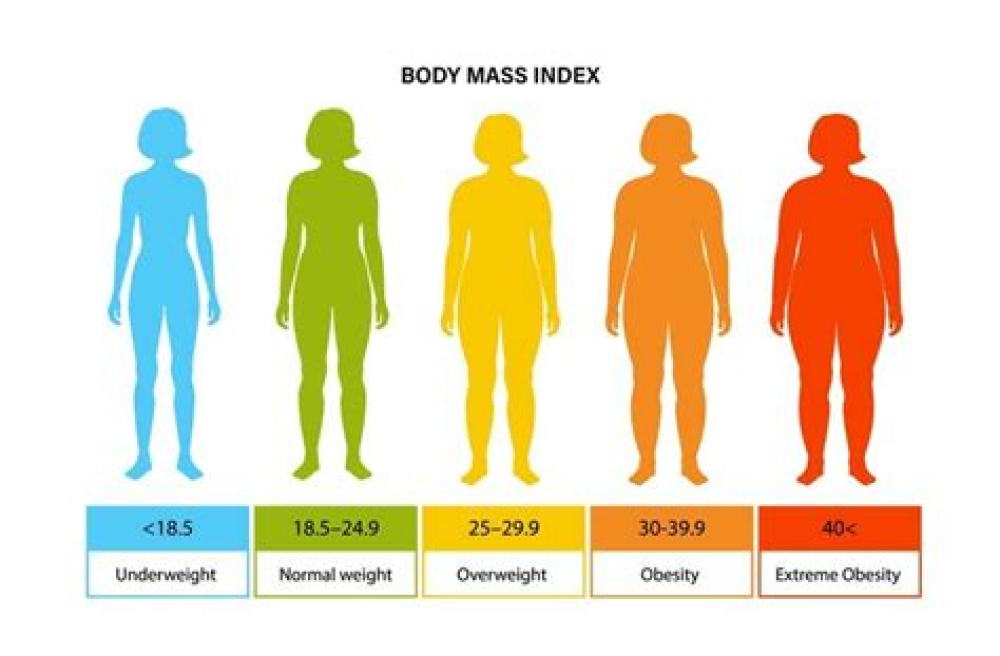
Obesity is a major risk factor for adverse outcomes after infection with SARS-CoV-2. We aimed to examine this association, including interactions with demographic and behavioural characteristics, type 2 diabetes, and other health conditions.
Methods
In this prospective, community-based, cohort study, we used de-identified patient-level data from the QResearch database of general practices in England, UK. We extracted data for patients aged 20 years and older who were registered at a practice eligible for inclusion in the QResearch database between Jan 24, 2020 (date of the first recorded infection in the UK) and April 30, 2020, and with available data on BMI. Data extracted included demographic, clinical, clinical values linked with Public Health England’s database of positive SARS-CoV-2 test results, and death certificates from the Office of National Statistics. Outcomes, as a proxy measure of severe COVID-19, were admission to hospital, admission to an intensive care unit (ICU), and death due to COVID-19. We used Cox proportional hazard models to estimate the risk of severe COVID-19, sequentially adjusting for demographic characteristics, behavioral factors, and comorbidities.
Findings
Among 6 910 695 eligible individuals (mean BMI 26·78 kg/m2 [SD 5·59]), 13 503 (0·20%) were admitted to hospital, 1601 (0·02%) to an ICU, and 5479 (0·08%) died after a positive test for SARS-CoV-2. We found J-shaped associations between BMI and admission to hospital due to COVID-19 (adjusted hazard ratio [HR] per kg/m2 from the nadir at BMI of 23 kg/m2 of 1·05 [95% CI 1·05–1·05]) and death (1·04 [1·04–1·05]), and a linear association across the whole BMI range with ICU admission (1·10 [1·09–1·10]). We found a significant interaction between BMI and age and ethnicity, with higher HR per kg/m2 above BMI 23 kg/m2 for younger people (adjusted HR per kg/m2 above BMI 23 kg/m2 for hospital admission 1·09 [95% CI 1·08–1·10] in 20–39 years age group vs 80–100 years group 1·01 [1·00–1·02]) and Black people than White people (1·07 [1·06–1·08] vs 1·04 [1·04–1·05]). The risk of admission to hospital and ICU due to COVID-19 associated with unit increase in BMI was slightly lower in people with type 2 diabetes, hypertension, and cardiovascular disease than in those without these morbidities.
For More Information: https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00089-9/fulltext