There is no cure or approved treatment for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). However, some symptoms can be treated or managed. Treating these symptoms might provide relief for some patients with ME/CFS but not others. Other strategies, like learning new ways to manage activity, can also be helpful.
Patients, their families, and healthcare providers need to work together to decide which symptom causes the most problems. This should be treated first. Patients, families, and healthcare providers should discuss the possible benefits and harms of any treatment plans, including medicines and other therapies.
Healthcare providers need to support their patients’ families as they come to understand how to live with this illness. Providers and families should remember that this process might be hard on people with ME/CFS.
Symptoms that healthcare providers might try to address are:
PATIENTS CAN USE THIS FILLABLE FORM TO KEEP TRACK OF THEIR MEDICATIONS AND CAN BRING IT TO DOCTOR APPOINTMENTS.
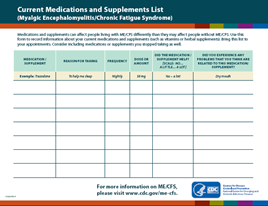
Handout: Current Medications and Supplements List pdf icon[PDF – 1 page]
Post-exertional Malaise (PEM)
Post-exertional malaise (PEM) is the worsening of symptoms after even minor physical, mental or emotional exertion. For some patients, sensory overload (light and sound) can induce PEM. The symptoms typically get worse 12 to 48 hours after the activity or exposure and can last for days or even weeks.
PEM can be addressed by activity management, also called pacing. The goal of pacing is to learn to balance rest and activity to avoid PEM flare-ups, which can be caused by exertion that patients with ME/CFS cannot tolerate. To do this, patients need to find their individual limits for mental and physical activity. Then they need to plan activity and rest to stay within these limits. Some patients and doctors refer to staying within these limits as staying within the “energy envelope.” The limits may be different for each patient. Keeping activity and symptom diaries may help patients find their personal limits, especially early on in the illness.
Being mindful of personal limits could prove to be a helpful coping skill for people living with ME/CFS. This enables them the ability to find balance between activities and rest, giving them a sense of managing the illness rather than the illness controlling them. People living with ME/CFS may find that everyday activities such as buying groceries, brushing their teeth, or interacting with others may be enough to cause a relapse or “crash”. It may not be possible to entirely avoid these situations, but people living with ME/CFS need to be aware of monitoring their own activity limits. When having a good day, it is tempting to try and “push” (increasing activity beyond what would normally attempt) to make up for lost time. However, this can then lead to a “crash” (worsening of ME/CFS symptoms); the cycle can then repeat itself after people start recovering from the crash.
Rehabilitation specialists or exercise physiologists who understand ME/CFS may help patients with adjusting to life with ME/CFS. Finding ways to make activities easier may be helpful, like sitting while doing the laundry or showering, taking frequent breaks, and dividing large tasks into smaller steps. Some patients find heart rate monitors useful in keeping track of how hard their body is working, as a way to prevent PEM. Patients who have learned to listen to their bodies might be able to increase their activity level. However, ME/CFS is unpredictable. PEM symptoms may not start right after exercise, making it important for each treatment plan to be tailored for each case. Exercise is not a cure for ME/CFS.
Any activity or exercise plan for people with ME/CFS needs to be carefully designed with input from each patient. While vigorous aerobic exercise can be beneficial for many chronic illnesses, patients with ME/CFS do not tolerate such exercise routines. Standard exercise recommendations for healthy people can be harmful for patients with ME/CFS. However, it is important that patients with ME/CFS undertake activities that they can tolerate, as described above.
Sleep
Patients with ME/CFS often feel less refreshed and restored after sleep than they did before they became ill. Common sleep complaints include difficulty falling or staying asleep, extreme sleepiness, intense and vivid dreaming, restless legs, and nighttime muscle spasms. Good sleep habits are important for all people, including those with ME/CFS. When people try these tips but are still unable to sleep, their doctor might recommend taking medicine to help with sleep. First, people should try over-the-counter sleep products. If this does not help, doctors can offer a prescription sleep medicine, starting at the smallest dose and using for the shortest possible time.
People might continue to feel unrefreshed even after the medications help them to get a full night of sleep.If so, they should consider seeing a sleep specialist. Most people with sleep disorders, like sleep apnea (symptoms include brief pausing in breathing during sleep) and narcolepsy (symptoms include excessive daytime sleepiness), respond to therapy. However, for people with ME/CFS, not all symptoms may go away.
Pain
People with ME/CFS often have deep pain in their muscles and joints. They might also have headaches (typically pressure-like) and soreness of their skin when touched.
Patients should always talk to their healthcare provider before trying any medication. Doctors may first recommend trying over-the-counter pain-relievers, like acetaminophen, aspirin, or ibuprofen. If these do not provide enough pain relief, patients may need to see a pain specialist. People with chronic pain, including those with ME/CFS, can benefit from counseling to learn new ways to deal with pain.
Other pain management methods include stretching and movement therapies, gentle massage, heat, toning exercises, and water therapy for healing. Acupuncture, when done by a licensed practitioner, might help with pain for some patients.
Depression, Stress, and Anxiety
Adjusting to a chronic, debilitating illness sometimes leads to other problems, including depression, stress, and anxiety. Many patients with ME/CFS develop depression during their illness. When present, depression or anxiety should be treated. Although treating depression or anxiety can be helpful, it is not a cure for ME/CFS.
Some people with ME/CFS might benefit from antidepressants and anti-anxiety medications. However, doctors should use caution in prescribing these medications. Some drugs used to treat depression have other effects that might worsen other ME/CFS symptoms and cause side effects. When healthcare providers are concerned about patient’s psychological condition, they may recommend seeing a mental health professional.
Some people with ME/CFS might benefit from trying techniques like deep breathing and muscle relaxation, massage, and movement therapies (such as stretching, yoga, and tai chi). These can reduce stress and anxiety, and promote a sense of well-being.
Dizziness and Lightheadedness (Orthostatic Intolerance)
Some people with ME/CFS might also have symptoms of orthostatic intolerance that are triggered when-or made worse by-standing or sitting upright. These symptoms can include:
- Frequent dizziness and lightheadedness
- Changes in vision (blurred vision, seeing white or black spots)
- Weakness
- Feeling like your heart is beating too fast or too hard, fluttering, or skipping a beat
For patients with these symptoms, their doctor will check their heart rate and blood pressure, and may recommend they see a specialist, like a cardiologist or neurologist.
For people with ME/CFS who do not have heart or blood vessel disease, doctor might suggest patients increase daily fluid and salt intake and use support stockings. If symptoms do not improve, prescription medication can be considered.
Memory and Concentration Problems
Memory aids, like organizers and calendars, can help with memory problems. For people with ME/CFS who have concentration problems, some doctors have prescribed stimulant medications, like those typically used to treat Attention-Deficit / Hyperactivity Disorder (ADHD). While stimulants might help improve concentration for some patients with ME/CFS, they might lead to the ‘push-and-crash’ cycle and worsen symptoms. “Push-and-crash” cycles are when someone with ME/CFS is having a good day and tries to push to do more than they would normally attempt (do too much, crash, rest, start to feel a little better, do too much once again).
Living with ME/CFS
Strategies that do not involve use of medications and might be helpful to some patients are:
- Professional counseling: Talking with a therapist to help find strategies to cope with the illness and its impact on daily life and relationships.
- Balanced diet. A balanced diet is important for everyone’s good health and would benefit a person with or without any chronic illness.
- Nutritional supplements. Doctors might run tests to see if patients lack any important nutrients and might suggest supplements to try. Doctors and patients should talk about any risks and benefits of supplements, and consider any possible interactions that may occur with prescription medications. Follow-up tests to see if nutrient levels improve can help with treatment planning.
- Complementary therapies. Therapies, like meditation, gentle massage, deep breathing, or relaxation therapy, might be helpful.
Important note: Patients should talk with their doctors about all potential therapies because many treatments that are promoted as cures for ME/CFS are unproven, often costly, and could be dangerous.
Disclaimer: This website is for informational purposes only. The information provided on this website is not intended to be a substitute for professional medical advice, diagnosis, or treatment.