Andrew G. Ewing, David Joffe, Svetlana Blitshteyn, et. al., Annals of Clinical Microbiology and Antimicrobials volume 24, Article number: 27 (2025)
Abstract
Background
Long COVID is a complex, heterogeneous syndrome affecting over four hundred million people globally. There are few recommendations, and no formal training exists for medical professionals to assist with clinical evaluation and management of patients with Long COVID. More research into the pathology, cellular, and molecular mechanisms of Long COVID, and treatments is needed. The goal of this work is to disseminate essential information about Long COVID and recommendations about definition, diagnosis, treatment, research and social issues to physicians, researchers, and policy makers to address this escalating global health crisis.
Methods
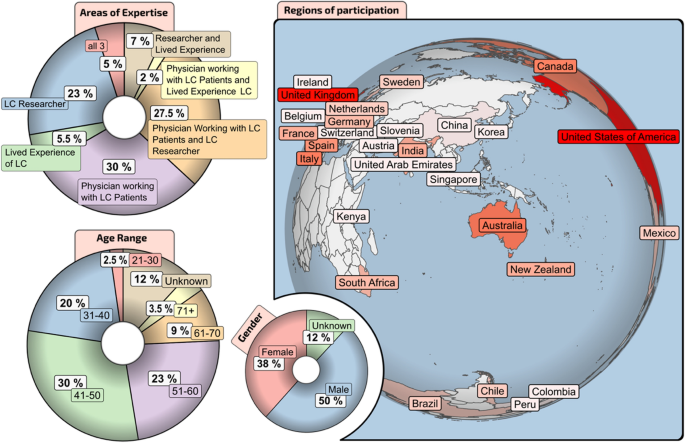
A 3-round modified Delphi consensus methodology was distributed internationally to 179 healthcare professionals, researchers, and persons with lived experience of Long COVID in 28 countries. Statements were combined into specific areas: definition, diagnosis, treatment, research, and society.
Results
The survey resulted in 187 comprehensive statements reaching consensus with the strongest areas being diagnosis and clinical assessment, and general research. We establish conditions for diagnosis of different subgroups within the Long COVID umbrella. Clear consensus was reached that the impacts of COVID-19 infection on children should be a research priority, and additionally on the need to determine the effects of Long COVID on societies and economies. The consensus on COVID and Long COVID is that it affects the nervous system and other organs and is not likely to be observed with initial symptoms. We note, biomarkers are critically needed to address these issues.
Conclusions
This work forms initial guidance to address the spectrum of Long COVID as a disease and reinforces the need for translational research and large-scale treatment trials for treatment protocols.
Introduction
The World Health Organization (WHO) lists ‘confirmed’ cases of COVID-19 at 775 million [1]. This number is likely much greater due to the limitations of testing and very limited surveillance [2]. Following acute COVID-19, the risk of developing symptoms that last beyond the initial illness, is estimated to be 15% per individual per infection [2]. This ailment is often termed Long COVID, but has several names including post-COVID conditions (PCC), post-acute COVID-19 or post-acute sequelae of SARS-CoV-2 infection (PASC).
Defining, diagnosing, treating, and understanding Long COVID and its impact on society pose some of the most significant scientific and medical questions of our time. The true global prevalence of Long COVID is likely much higher than 100 million as risk is amplified by reinfection [3] similarly affecting all ethnicities, with most cases in 18- to 64-year-olds. Women are affected approximately twice as often as men [4]. SARS-CoV-2 can also cause organ damage in individuals both with and without symptoms [5, 6].
From July 2023 to February 2024, a global panel of experts of more than half physicians diagnosing and treating Long COVID, as well as researchers and those with lived experience, engaged in a modified Delphi consensus process [7, 8]. Topics included definition, diagnosis and clinical assessment, treatment, research, and socioeconomic factors related to Long COVID. The overarching goal was to provide recommendations to physicians, researchers and policy makers.
Methods
Delphi expert panel member selection
This modified Delphi electronic survey (using the Survey Monkey platform) on Long COVID was conducted under the governance and oversight of the World Health Network (WHN). We used an open sampling approach to generate the panel for this Delphi study. The WHN Long COVID working group, with a membership of 12 members, initiated the study. During the progression of the study the group enlarged to 20 members and an additional 14 members were recruited to form an extended evaluation committee. The working group met bi-weekly and the extended committee on invitation. The target panel for the survey was chosen to include clinicians (e.g., general practitioners, pulmonologists, cardiologists, neurologists) and researchers with expertise in Long COVID. A comprehensive literature search was carried out to identify physicians and researchers working and publishing on Long COVID and an email inquiry was sent to them (n = 1574) to ascertain their willingness to participate. As new literature was published, new members were invited at each new round in the survey.
Areas of expertise, 28 countries of participation, and panel genders and age groups are shown in Fig. 1. Selection of the expert panel involved semi-purposeful sampling [9], which had the criterion that panellists had expertise in COVID-19/Long COVID and/or rehabilitation.
Delphi method data collection
The Delphi method was modified to ensure the methodology was suitable for the study aims instead of configuring the study aims to fit the methodology [10, 11]. The first round of a traditional Delphi typically uses open questioning to identify the focus. However, in the present study, this was modified to include 34 health care professionals as well as patients and public involvement and engagement (PPIE), reviewing the existing literature until July 2023, and generating structured questions using a roundtable approach.
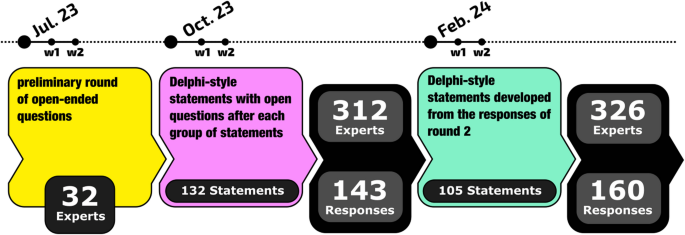
Figure 2 shows a breakdown of the survey process and numbers of responses. The international surveys included a preliminary round of open-ended questions (SI Table S4) to generate a broad range of opinions and perspectives. This provided 32 responses that were then used by the working group to generate Delphi-style statements in the areas of Long COVID definition, diagnosis, treatment, evaluation of treatment, research, and social issues (SI Table S5), with open questions after each group of statements for round 2 of the survey. Open-text responses were not analyzed using a formal process but were considered by the trial steering group using a roundtable approach with individual members adding potential new statements for discussion and refinement by the group. The third round of the survey (SI Table S6) was developed from the responses from round 2. These statements were developed by the extended committee to A) modify statements not receiving consensus in the earlier round and B) to address the open-ended comments. Respondents were given ∼3 weeks to complete the surveys.
Delphi data analysis
A 5-point Likert Scale was used (Tables S5 and S6) and for some statements ‘do not have the expertise to answer’ was considered necessary based on the diversity of the expert panel. Anonymized results were summarized into excel tables and a sum for agree and strongly agree was determined for consensus. The proportion who chose ‘I do not have the expertise to answer’ was removed from the denominator to calculate levels of agreement/disagreement. A supermajority (that is, ≥ 67% combined agreement – strongly agree and agree) was used as a minimum cut-off for consensus. This more demanding cut-off (versus a simple majority of greater than 50%) was decided to ensure clear consensus.
Results
A list of 187 statements reaching consensus by topic across survey rounds two and three is given in Table 1. A pictorial summary of consensus statement numbers by topic is given in Fig. 3. Statements are arranged with the following levels of agreement: ‘U’ denotes unanimous (100%) agreement; ‘A’ denotes 90–99% agreement; ‘B’ denotes 78–89% agreement; ‘C’ denotes 67–77% agreement. Table 1 Statements reaching consensus by topic and level of agreement
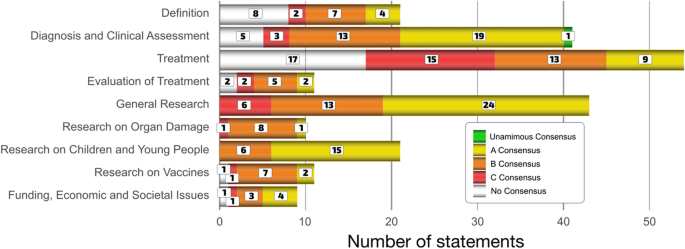
The strongest consensus areas were in diagnosis and clinical assessment (1 statement unanimous, 19 with A-level, 13 with B-level and 3 with C-level statements), general research (24 A-level statements, 13 B-level and 6 C-level), research on children and young people (15 A-level statements and 6 B-level), and funding, economic and societal issues (4 A-level statements, 3 B-level, and 1 C level). Organ or body damage (1 A-level, 8 B-level and 1 C-level statements) and Long COVID and vaccines (2 A-level, 7 B-level, and 1 C-level statements) require more research before we can reach a broad consensus. Not surprisingly, there less congruence on treatment (9 A-level, 13 B-level and 15 C-level statements) and evaluation of treatment (2 A-level, 5 B-level and 2 C-level statements) as clinicians around the world have adopted their own practices in the absence of clear guidelines or a strong evidence-base. This reinforces the need for translational research and trials.
Statements not reaching consensus are listed in Table S2 of the supporting information. Of these 34 statements, 8 deal with definition, 5 with diagnosis, 17 with treatment, 2 with evaluation of treatment, 1 statement on vaccination improving Long COVID and 1 statement nearly reaching consensus calling for routine cognitive impairment testing in critical professions (discussed below). It is not surprising that definition and treatment have the most statements not reaching consensus as they are the areas most in need of clarity in understanding Long COVID.
Discussion
Long COVID definition
The WHO [12], CDC [13], USA NESAM [14] and others have proposed candidate definitions (Table 2), but there is currently no single unified definition of Long COVID, which is a detriment to the research, diagnostics, treatment, and patient rights. The consensus agreement emphasises that functional impairment, reduced effort tolerance, new-onset or worsening of pre-existing conditions, abnormalities in clinical parameters or medical imaging, and other detectable systemic pathology should be included in the definition or as a distinct clinical category, regardless of the presence or absence of associated symptoms. Of the listed definitions, this component is currently present only in the USA NESAM definition, which includes not only symptoms but also diagnosable conditions which may or may not produce recognizable symptoms. These include interstitial lung disease and hypoxemia, cardiovascular disease and arrhythmias, cognitive impairment, stroke, hyperlipidemia, blood clots, chronic kidney disease, and many other diseases which are known to often remain clinically silent until late in their natural history when the physiological reserve is exhausted. The main contributions of the work presented here are recognizing (1) the role of functional impairment in Long COVID; and (2) the diversity of distinct associated conditions and different treatments.
Diagnosis recommendations
There was unanimous consensus for a need to educate all health care workers about the possible complications following SARS-CoV-2 infection. The panel was clear that patients should be listened to, appropriately investigated, and supported.
Long COVID is multi-systemic and may present with different phenotypes that fall under the umbrella of Long COVID. Thus, the process of diagnosis must reflect the complexity of the condition, and the variability of signs and symptoms among individuals may present a special challenge for clinicians. The first step in the diagnostic process is the determination that the individual patient has experienced a prolonged change in health status and a decline in functioning following an acute SARS-CoV-2 infection.
This consensus underlines the need for a nuanced and multi-dimensional diagnostic approach, considering the broad spectrum of Long COVID manifestations. The necessity for individualised diagnostic strategies to effectively capture and manage the disease’s complexity is also emphasized. A summary of significant diagnostic criteria derived from the consensus statements is given in Table 3.Table 3 Recommended diagnostic tests available to clinicians for evaluation of patients with Long COVID based on clinical history and examination
The change in health status may include not only the appearance of symptoms and signs of illness, but decreased ability to perform or greater effort needed to maintain activities of daily living compared to the pre-COVID-19 state. Self-reported impairment of energy level, cognitive function, changes in mood, sleep or social interactions and exercise tolerance are all important indicators. The second diagnostic step is typically an assessment of possible alterations in cardiovascular, respiratory, metabolic, endocrine, renal or neurological health, as each of these systems alone or in combination may be affected in patients with Long COVID.
Currently, there are no evidence-based guidelines on the diagnosis of Long COVID and no specific validated diagnostic tests that are clinically available to diagnose Long COVID. Thus, the diagnosis is based primarily on clinical assessment consisting of detailed history and physical exam, in conjunction with the currently available diagnostic tests that help identify objective evidence of possible underlying pathophysiology and possible post-COVID-19 conditions. Several consensus guidance statements on the assessment of Long COVID and post-COVID-19 conditions have been developed to help guide healthcare practitioners in the diagnostic approach to Long COVID [15,16,17].
Clearly, there is a great need to develop a spectrum of validated, clinically useful and easily accessible diagnostic tests for patients with Long COVID. These may assess endothelial, microclotting, as well as mitochondrial functions, oral and gut microbiome, and inflammatory, immunologic, autoimmune and hypercoagulable state biomarkers. For example, a number of reports have discussed gut microbiome dysbiosis resulting from COVID infection, and affecting other organs [18,19,20]. Biomarkers may include serum cytokines and antibodies that underlie the pathophysiology of Long COVID. Several markers have been suggested as potential diagnostic biomarkers for Long COVID, including Interleukin 6 [21], C-reactive protein, tumor necrosis factor alpha, neurofilament light chain, glial fibrillary acidic protein and transforming growth factor beta [22,23,24]. Aside from C-reactive protein and other inflammatory and autoimmune markers available as part of the standard diagnostic serum panels, most of these biomarkers are not readily available or easily accessible in clinical practice around the world. Bridging the gap between testing available to researchers and those available to clinicians is paramount to improving diagnostic capabilities and investigations available to patients and their treating physicians.
Treatment and evaluation of treatment
To-date, like diagnostic approaches, there are no evidence-based guidelines on the treatment of Long COVID and no specific validated procedures that are clinically available to treat this complex disorder. Consensus shows it requires an individual and tailored approach to each patient accounting for patient history and physical examination and that multidisciplinary team management is beneficial.
Treatment has focused predominantly on the demonstrable pathologies and manifestations of their many varied presentations and identified processes. Midodrine, ivabradine beta-blockers, and fludrocortisone can be used for POTS [25,26,27], whereas a combination of 5-HT1 inhibitors and two antihistamines can be helpful for management of symptoms of MCAS [28]. Statins can be used for hyperlipidaemia and melatonin for sleep dysrhythmia and endothelial protection. There have been several randomised controlled studies but no single unifying therapy. Considerable gaps remain in treatment protocols including the use of anticoagulants, probiotics [29], and mitochondrial supplements. Larger trials of antivirals for both prevention and treatment of Long COVID are needed. A small RCT showed no benefit of 15 days of nirmatrelvir-ritonavir [30]. Whilst there is a vast array of therapies for specific issues, there are few well-performed RCTs for treatment efficacy in Long COVID.
A summary of significant treatment criteria from consensus is given in the Supporting Information (Table S3). Clearly there is agreement that multidisciplinary team tailored therapies are essential [31]. The management of POTS, sleep disturbance and MCAS were highly conserved across both Delphi rounds 2 and 3. Attention to clotting abnormalities, whilst considered important, the consensus suggests that this is best undertaken when biomarkers are available, and expertise is required for treatment oversight.
There was excellent consensus for the appropriate treatment of mood disorders and the conjunctive value of psychological therapies and support [32]. Formal neurocognitive evaluation both at presentation and at follow-up is strongly supported. The usual standard evaluation tools were considered inadequate and more comprehensive testing was strongly recommended. This is critical as COVID-19 can lead to long-term cognitive impairment [33].
There was considerable caution around exercise and pulmonary rehabilitation, particularly in the absence of an adequate clinical evaluation and exclusion of POTS and PEMS [34]. The value of non-invasive vagus nerve stimulation therapies (including stimulators, cold exposure breathwork, mindfulness, and trauma release) was supported, but not strongly. This may reflect local practices and experience as well as the lack of RCT’s for external stimulators and the efficacy of non-conventional treatments. Tracking devices for assessment of heart rate, sleep quality and pacing for patients, whilst Level B, may have value for both clinicians and patients. Group data for prospective evaluation of therapeutics may be where this lies in the future.
Future research focus
The overarching consensus from this Delphi, with regards to research, is the need for a designed framework. This will allow for a structured approach to addressing Long COVID, outlining key focus areas of interest, concern, and need.
The consensus statements on research and particularly on organ damage, align closely with the existing literature, which increasingly supports a multi-system involvement in Long COVID [6, 35]. Research to date indicates a complex interplay of factors that may contribute to the persistence of symptoms, suggesting the need for a holistic approach in future studies. Ongoing research has shown that Long COVID impacts the immune system [36] and there is an increased risk of cardiovascular complications such as heart attacks, coronary heart disease, heart failure, and deep vein thrombosis among those infected [37,38,39]. These cardiovascular issues are often precipitated by disruptions in endothelial cell function, which regulate the flow of substances into and out of tissues and are a focal point of the virus’s deleterious effects [40]. The virus also poses significant neurological risks [41].
Consistent with the consensus agreement, persistent symptoms have been associated with metabolic and endocrine systems, potentially leading to diabetes through mechanisms involving pancreatic dysfunction and altered insulin responses [42]. Reproductive health issues in both males and females have been noted [43,44,45]; with the virus affecting hormonal balances, potentially disrupting menstrual cycles, impairing fertility, and complicating pregnancies. Kidney damage from the virus can escalate to chronic kidney disease, and gastrointestinal symptoms, may persist or lead to chronic conditions, reflecting the virus’s ability to infect intestinal cells and possibly alter the gut microbiome [46, 47]. This extensive involvement of diverse bodily systems illustrates the critical need for a multi-disciplinary approach in research and treatment strategies for COVID-19 and Long COVID, highlighting the virus’s ability to cause systemic damage beyond the respiratory system.
The research directions highlighted in the consensus emphasize the importance of investigating the relationship between Long COVID and other health conditions, such as sleep disorders, dysbiosis, and PEM. This suggests a complex interplay between Long COVID and pre-existing vulnerabilities or concurrent health issues. As most of the COVID-19-induced pathophysiology is immune-mediated or even immunologically driven, interactions with any existing or future inflammatory conditions are likely to be important at an individual level. The emphasis on endothelial dysfunction, coagulopathy, and mitochondrial dysfunction points to a nuanced understanding of the disease’s pathophysiology, indicating potential pathways for targeted treatments.
Global SARS-CoV2 vaccination programs have saved lives, and research shows on a population basis that COVID vaccines reduce the risk of long COVID [48, 49]. However less is known about the individual effects of vaccination on patients who have pre-existing immune mediated inflammation from Long Covid. A common question our long COVID clinicians are asked by patients is whether the vaccine will make their long covid symptoms better or worse. To our knowledge this has not been studied and our experts showed consensus agreement that this was an important area for further research so clinicians can give patients scientifically informed answers. There was not agreement with the statement, ‘Long COVID can improve with vaccination.’ The consensus and nonconsensus show that vaccination and Long COVID is an issue that is still not clear.
In parallel, the consensus points to the need to address factors that may lower the incidence of Long COVID, such as reducing SARS-CoV-2 transmission and improving indoor air quality, highlighting the intersection between public health measures and individual health outcomes. This underscores the complexity of Long COVID and the necessity for longitudinal studies to fully comprehend its long-term implications.
The growing number of reports and studies on Long COVID in children show that dedicated research into how the condition affects this vulnerable population is imperative. Consensus points from recent rounds highlight the importance of studying the effects on educational performance, mental health, and physiological development. These priorities resonate with recent findings which underscore the unique challenges faced by children with Long COVID [50], including the potential for significant developmental disruptions and the need for tailored clinical approaches.
Existing evidence on Long COVID in children is scarce, partly due to a lack of a standardized case definition, short follow up duration, and heterogenous study designs, resulting in wide variation of reported outcomes [51]. Stigmatization of children, due to a lack of an understanding or ignorance about the disease in children has also been reported [45]. There has, however, been evidence for widespread endothelial damage in children with Long COVID [52, 53].
A pivotal area of concern is the interaction between Long COVID and the education system, highlighting the need to explore how the condition affects school attendance and performance. This extends to the potential cognitive repercussions, including impacts on the developing brain and resultant challenges in learning and development. Of note, meta-analysis identified five pediatric studies documenting abnormal brain imaging findings in children and young people with Long COVID [54]. Moreover, the physical health consequences of Long COVID in children, such as new onset diabetes and alterations in the immune system, underscore the critical need for studies tailored to the pediatric population. The investigation into the long-term physiological effects, including those as specific as thrombotic endotheliosis, presents a clear directive for future research endeavors. This is particularly relevant considering recent pilot studies documenting objective physiological abnormalities in young patients with Long COVID, including dysautonomia [55, 56], pathological cardiopulmonary exercise testing [57], immune dysregulation [58], and platelet activation [53].
It is important to note that the burden of post-acute sequelae of COVID-19 may go beyond what is currently referred to as Long COVID. For example, there may be sub-clinical impacts following a SARS-CoV-2 infection as well as symptoms that may not be considered related to Long COVID. Unrecognized sequelae include new onset health conditions [3, 59] or worsening of pre-existing health conditions [60] in adults and children. Diverse medical presentations may not be considered Long COVID due to a lack of awareness. An area of research agreed on by consensus is to develop biomarkers for Long COVID, and this can be extended to unrecognized conditions including the heart, brain, vasculature, and more.
Long COVID funding, economic impact and societal issues
The consensus reached through the modified Delphi process offers a nuanced view of the global response required to address the socioeconomic challenges of Long COVID. More effective strategies and interventions are needed, especially for more impacted groups, since disparities appear exacerbated by Long COVID. A mixed-methods study across five countries explored the economic and social impacts of COVID-19 revealing significant disparities based on age, education, household size, and income [61]. Also, the well-known COVIDENCE UK study highlights the economic vulnerability caused by COVID-19, showing increased short-term household income inadequacy and long-term sickness absence from work, indicating a cycle of impaired health and poor economic outcomes [62]. Additionally, Long COVID requires a reinforced epidemiological surveillance program or periodic reviews for the health personnel who fall ill with it, having been the ones who provided direct care to patients who suffered from COVID-19.
Studies have also quantified impacts of Long COVID on workforce participation, sick leave, disability, and economic activity. A UK cohort study quantified the health and economic burden of Long COVID, finding substantial impacts on health-related quality-of-life and emphasizing the need for continued support and research for those affected [63]. Another population-based cohort study in Hong Kong evaluated the long-term spill-over effects of COVID-19 on people with non-communicable diseases, showing significant disruptions in health outcomes and healthcare costs, stressing the need for optimized care [64].
In synthesizing the consensus points, it becomes evident that tackling Long COVID requires a concerted effort from all sectors of society. For example, Uwishema et al. (2022) highlight how COVID-19 disrupts healthcare access for neurological patients in Africa, a challenge likely magnified by Long COVID’s chronic burden [65] and Uwishema and Boon emphasize addressing neurological care inequities, a priority echoed in Long COVID’s global burden on underserved populations [66]. The insights gained from this modified Delphi study not only inform immediate policy and research priorities but also illustrate the broader societal shifts necessary to deal with the pandemic’s long-term effects effectively. The consensus conclusions can be aggregated into the following overarching considerations: (1) an interdisciplinary approach is needed to address the issue of Long COVID; (2) educational adjustments and policy implications need to be discussed and implemented; and (3) corporate responsibility and public health funding are needed. Additionally, the near consensus calling for routine cognitive impairment testing in critical professions underscores the practical implications of Long COVID on workforce safety and productivity.
Strengths and limitations
One of the strengths of this study is the broad scope covering the entire issue of Long COVID. Another strength is we minimized potential bias by generating a large, geographically and diverse panel from multiple sources where nominees from the working group were combined with a comprehensive literature search to identify Long COVID authors. These made up most of the panelists. Additionally, we implemented a modified Delphi methodology where we used experts identified by literature search to answer questions about the most important topics in Long COVID. This allowed the most unbiased approach possible to an understanding of this complex topic and development of subsequent statements. The large sampling of physicians working with LC patients, and researchers, gives this consensus credibility, especially in the areas of understanding what Long COVID looks like, how it is diagnosed and treated, as well as what should be researched. Finally, statements from the second round of Delphi process were made clearer for round three with the help of open-ended comments after each section of the survey.
The Delphi method has many advantages, but limitations also exist. One limitation is that the survey was voluntary and, hence, this self-selection might have omitted some experts. However, everyone who wanted to participate was able to do so. It is important to note that a small number of the panel experts (16%) were also on the extended committee. This number is small making it unlikely to be significant. Another limitation is that Long COVID is an evolving syndrome, and the science reviewed in this paper covers a time period from mid-2023 to mid-2024; the scientific evidence will have to be revisited later. A follow up survey might be useful when diagnosis and treatment are more refined. One consideration that is difficult to address is that there might be insufficient data due to lack of good healthcare protocols especially in lower-middle income countries and issues related to stigmatization with people not going to the hospital, missed data, lack of funding and people not able to afford medical visits and therefore not being assessed for Long COVID. Furthermore, differences in how long covid cases are managed in high-income vs low-middle income countries might lead to differences across panelists. This limitation should be addressed by the broad range of countries used in this survey.
An important concern can be raised that there is a lack of randomized controlled trials in the areas of diagnosis and treatment of Long COVID. These still need to be developed, but our consensus establishes the groundwork for implementation of clinical care for people with Long COVID.
Conclusions
This modified Delphi study is the first to provide international consensus regarding the clinical evaluation and medical investigation of Long COVID with expert consensus recommendations to physicians. Gaining consensus agreement from 179 experts around the globe we establish conditions for diagnosis of different subgroups within the Long COVID umbrella. Strong consensus was gained for assessment and treatment of Long COVID-associated conditions, including POTS, MCAS, insomnia, new onset dyslipidemia, diabetes, and hypertension. Consensus was also achieved that cardio-metabolic disturbance should be ruled out before prescribing graded exercise therapy as treatment. Biomarkers, where available, may be useful when monitoring treatment response to Long COVID.
Our expert panel agreed that further research was urgently needed for Long COVID. It was recommended that an international task force should be developed to oversee research priorities and facilitate/encourage global collaborative efforts and data sharing. Instead of abandoning public health related to infectious diseases, governments need to reaffirm priorities. There are over 400 million people worldwide affected by Long COVID and it is not just for covid, but for all post viral syndromes, that this work needs to be done. Clear consensus was reached that the impacts of COVID-19 infection on children should be a research priority (e.g. prevention of transmission in schools, long-term impacts of infections, impacts on learning/development, etc.). Consensus was also reached on the need to determine the effects of Long COVID on societies and economies, and that governments need to prioritize investment in public health protections to prevent reinfections.
