Chronic Venous Insufficiency (CVI)—a condition where leg veins fail to return blood efficiently to the heart—has gained renewed attention in 2025 due to its association with COVID-19, particularly in patients with vascular complications post-infection or post-vaccination. This article synthesizes recent peer-reviewed findings to explore the etiology, spike protein interactions, and therapeutic strategies for managing CVI in the COVID era.
🧬 Etiology: How COVID Contributes to CVI
CVI typically arises from valvular dysfunction in the leg veins, leading to retrograde blood flow, pooling, and increased venous pressure. COVID-19 exacerbates this through:
- Endothelial damage caused by the SARS-CoV-2 spike protein
- Microvascular thrombosis and inflammatory vasculitis
- ACE2 receptor dysregulation, impairing vascular tone and repair
- Sedentary lifestyle changes during illness or lockdowns
A 2025 review from Columbia University noted a surge in CVI cases linked to reduced calf muscle activity and weight gain during the pandemic.
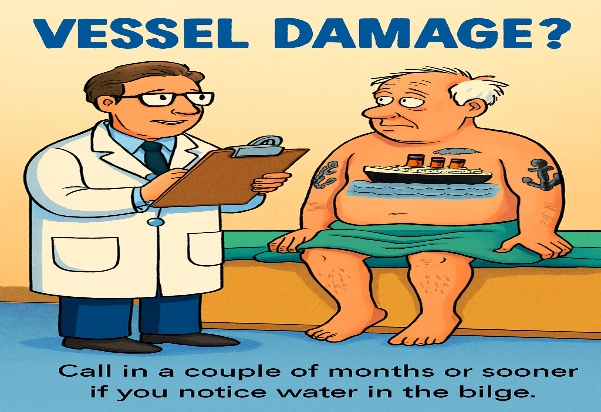
The common condition occurs when leg veins become damaged over time and can’t work as they should, causing blood to pool in the legs.
This increases pressure in the leg veins, leading to symptoms like ankle swelling, leg cramps, ulcers and flaky skin.
Chronic venous insufficiency affects about one in 20 adults, and the risk increases with age, according to Cleveland Clinic.
Chronic venous insufficiency happens due to damage to in the leg veins, slowing down blood flow from the legs back up to the heart.
The condition can cause mild symptoms at first but, over time, it can interfere with your quality of life and lead to serious complications, according to Cleveland Clinic.
Without treatment, it can increase pressure in the legs, causing tiny blood vessels in the leg to burst.
This can give skin in the legs a reddish-brown hue and also make it more vulnerable to injury is bumped or scratched.
Here are 10 telltale symptoms of chronic venous insufficiency to know.
- Achy or tired legs
- Burning, tingling or “pins and needles” sensation in your legs
- Cramping in your legs at night
- Discoloured skin that looks reddish-brown
- Oedema (swelling) in your lower legs and ankles, especially after standing a while or at the end of the day
- Flaking or itching skin on your legs or feet
- Full or heavy feeling legs
- Leathery-looking skin on your legs
- Ulcers (open sores), usually near your ankles
- Varicose veins
Varicose veins are swollen, twisted veins that become visible under the skin, usually in the legs.
They happen when the valves that control the flow of blood in your vein do not work properly.
This causes blood to build up and put pressure on the vein, which makes it swell and twist.
🧪 Spike Protein, ACE2, and Endothelitis
🔹 Mechanistic Cascade
| Component | Role in CVI Pathogenesis |
|---|---|
| Spike Protein | Binds to ACE2 on endothelial cells, triggering inflammation |
| ACE2 Receptor | Downregulated post-infection, impairing vascular repair |
| Endothelitis | Inflammation of vessel lining, leading to clot formation and leakage |
| Microclots | Fibrin-amyloid clots block venous return, worsen tissue perfusion |
| Bleeding Risk | Damaged vessels may rupture, causing petechiae or purpura |
Studies show that spike protein induces IL-6, TNF-α, and CXCL2, promoting endothelial dysfunction and immune complex deposition, which are hallmarks of cutaneous vasculitis and venous insufficiency progression3.
🩺 Therapeutic Regimen in 2025
🔹 Conservative Management
- Compression therapy: Graded stockings to reduce edema and improve venous return
- Leg elevation: Minimizes pooling and pressure
- Exercise: Calf muscle activation improves venous pump function
🔹 Pharmacologic Interventions
| Medication | Purpose |
|---|---|
| Diuretics | Reduce fluid overload and edema |
| Anticoagulants (LMWH, DOACs) | Prevent or treat microvascular clots |
| Anti-inflammatories | Manage endothelitis and cytokine storm |
| Flavonoid supplements | Improve capillary resistance and tone |
🔹 Interventional Therapies
- Endovenous laser ablation (EVLA): Closes damaged veins
- Radiofrequency ablation (RFA): Minimally invasive vein closure
- Sclerotherapy: Chemical injection to collapse dysfunctional veins
- Valve repair or vein bypass: For advanced CEAP stages (C5–C6)
🔹 COVID-Specific Strategies
- ACE2-Fc decoy therapy: Blocks spike protein binding, reduces clot formation
- Anti-fibrin agents: Target spike-fibrin interactions to prevent neurovascular damage
📊 Summary Table
| Aspect | Findings |
|---|---|
| Etiology | COVID-induced endothelial damage, sedentary lifestyle, spike protein toxicity |
| Spike–ACE2 interaction | Triggers endothelitis, clotting, and vascular leakage |
| Symptoms | Leg swelling, pain, skin changes, bleeding spots |
| Treatment | Compression, anticoagulants, ablation, ACE2 decoy therapies |
| Prognosis | Manageable with early intervention; risk of ulcers and long-term disability |
How is chronic venous insufficiency treated?
Being overweight, having a family history of chronic venous insufficiency or suffering blood clots or injuries to your legs can up your risk of the condition.
Having high blood pressure, smoking and not exercising enough can also be risk factors.
Lifestyle tweaks can help with managing chronic venous insufficiency.
This can include taking up walking or other forms of exercise to improve blood flow in your legs.
It’s recommended that you don’t sit or stand for too long, so getting up and moving as often as you can can be helpful.
Foot and ankle flexing exercises may also help.
📚 Peer-Reviewed Sources
- Columbia University: Pandemic impact on vein health
- MedShun: Spike protein and blood clots
- Vejon Health: Endothelial damage and spike persistence
- Journal of Biomedical Science: ACE2-Fc therapy
- Nature: Fibrin-spike interaction and brain/lung damage
- American Heart Association: CVI and cardiovascular risk
- Gurukripa Hospitals: CVI treatment guide 2025
- SCAI Guidelines: Chronic venous disease management