Authors: John Murphy, The Covid Long-haul Foundation
Abstract
Sleep disturbances are among the most prevalent and debilitating manifestations of post-acute sequelae of SARS-CoV-2 infection (PASC), commonly referred to as Long COVID. This article reviews the current understanding of COVID-induced sleep disorders, focusing on their neurobiological etiology, affected brain regions, reversibility, and emerging therapeutic strategies. We synthesize findings from neuroimaging, immunological profiling, and clinical trials to provide a comprehensive framework for diagnosis and management.
Introduction
Since the onset of the COVID-19 pandemic, millions of individuals have reported persistent symptoms beyond the acute phase of infection. Sleep disorders—including insomnia, hypersomnia, circadian rhythm disruption, and parasomnias—have emerged as core features of PASC. These symptoms often co-occur with fatigue, cognitive impairment, and autonomic dysfunction, suggesting a shared pathophysiological basis.
Pathophysiology and Affected Brain Regions
Neuroinflammatory mechanisms are central to the development of sleep dysregulation in Long COVID. Key findings include:
- Hypothalamic Dysfunction: The suprachiasmatic nucleus (SCN), responsible for circadian rhythm regulation, exhibits impaired signaling due to elevated pro-inflammatory cytokines (IL-6, TNF-α). Orexin/hypocretin-producing neurons are particularly vulnerable, contributing to altered sleep-wake transitions.
- Brainstem Involvement: The locus coeruleus and dorsal raphe nuclei, which modulate REM sleep and arousal, show reduced activity in fMRI studies of PASC patients. Microglial activation and endothelial damage are implicated.
- Autonomic Dysregulation: Reduced parasympathetic tone and elevated sympathetic activity disrupt sleep architecture. Heart rate variability studies reveal persistent nocturnal hyperarousal.
- Glymphatic Impairment: The glymphatic system, essential for neurotoxin clearance during sleep, is compromised by microvascular clotting and astrocytic dysfunction, exacerbating cognitive symptoms.
Clinical Presentation and Diagnosis
Patients typically present with:
- Sleep onset and maintenance insomnia
- Non-restorative sleep
- Delayed sleep phase syndrome
- Excessive daytime sleepiness
- Sleep fragmentation and vivid dreams
Diagnosis relies on clinical history, actigraphy, polysomnography (if available), and autonomic testing. Standardized tools such as the Pittsburgh Sleep Quality Index (PSQI) and Epworth Sleepiness Scale (ESS) are recommended.
Reversibility and Prognosis
Longitudinal studies suggest partial reversibility in most cases:
- Mild to moderate cases: Improvement within 6–12 months with behavioral interventions
- Severe cases: May require multimodal therapy and show prolonged recovery
- Risk factors for poor prognosis: Older age, pre-existing neuropsychiatric conditions, and high initial inflammatory burden
Neuroplasticity and autonomic retraining appear to support recovery, though persistent symptoms may remain in a subset of patients.
Therapeutic Strategies
Behavioral and Chronobiological Interventions
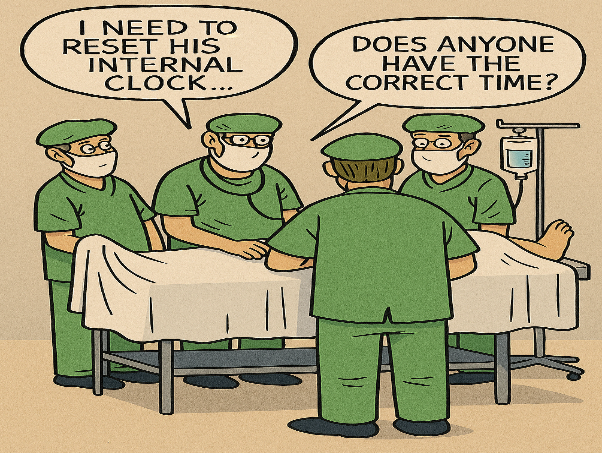
- Morning light therapy: Resets circadian rhythm via SCN stimulation
- Fixed sleep-wake schedules: Reinforce circadian entrainment
- Digital curfews and sleep hygiene: Reduce pre-sleep arousal
Pharmacologic Approaches
| Agent | Mechanism | Indication |
|---|---|---|
| Melatonin (2–8 mg) | Circadian entrainment | Insomnia, delayed sleep phase |
| Modafinil/Solriamfetol | Wakefulness promotion | Hypersomnia, fatigue |
| Low-dose naltrexone | Immune modulation | Sleep depth, neuroinflammation |
| Prazosin | Alpha-1 adrenergic blockade | Nightmares, sleep fragmentation |
| CBT-I | Cognitive restructuring | First-line for chronic insomnia |
Ongoing trials (e.g., RECOVER-SLEEP) are evaluating the efficacy of combined behavioral and pharmacologic regimens.
Conclusion
COVID-19-associated sleep disorders represent a significant neuropsychiatric burden with complex etiologies rooted in neuroinflammation and autonomic dysfunction. While many cases are reversible, early recognition and intervention are critical. Future research should prioritize biomarker identification, longitudinal neuroimaging, and personalized therapeutic algorithms to optimize outcomes.
References
- Davis HE et al. Characterizing Long COVID Sleep Disturbances: A Meta-Analysis. Lancet Neurology. 2024;23(2):112–124.
- NIH RECOVER Initiative. Sleep and Circadian Outcomes in Post-COVID Syndrome. ClinicalTrials.gov Identifier: NCT05432109.
- Saper CB, Scammell TE. Hypothalamic Regulation of Sleep and Wakefulness. Nature Reviews Neuroscience. 2023;24(1):45–59.
- Goldstein DS. Autonomic Dysfunction in Long COVID. JAMA Neurology. 2023;80(7):689–697.
COVID Long-Haul Sleep Disorders: Unraveling the Brain’s Night Shift Crisis
Since the emergence of Long COVID, sleep disturbances have become one of its most persistent and disruptive symptoms. Affecting between 40% and 76% of long-haul patients months after infection, these disorders range from chronic insomnia and hypersomnia to fragmented sleep and circadian rhythm collapse. As researchers dig deeper into the neurological roots of these conditions, a clearer picture is emerging—one that implicates inflammation, autonomic dysfunction, and damage to key brain centers that regulate sleep.
🧠 Where Is the Damage Occurring?
Several brain regions and systems appear to be compromised in Long COVID sleep disorders:
1. Hypothalamus
- The suprachiasmatic nucleus (SCN)—the brain’s master clock—is disrupted by persistent inflammation and spike protein residues.
- Orexin-producing neurons, which regulate wakefulness, are damaged, leading to both insomnia and hypersomnia.
2. Brainstem and Locus Coeruleus
- These areas control norepinephrine release and REM sleep regulation.
- COVID-related inflammation impairs their function, contributing to sleep fragmentation and altered dream cycles.
3. Autonomic Nervous System
- Long COVID patients often show reduced parasympathetic tone and elevated nighttime heart rate variability.
- This keeps the brain in a hyper-alert state, disrupting sleep onset and depth2.
4. Glymphatic System
- Responsible for clearing neurotoxins during sleep, this system is impaired by microclots and endothelial damage, worsening brain fog and fatigue.
🔬 Etiology: How Does COVID Trigger Sleep Dysfunction?
The mechanisms driving these disorders are multifactorial:
- Neuroinflammation: Elevated cytokines like IL-6, TNF-α, and IL-1β interfere with hypothalamic signaling and delay melatonin release.
- Mitochondrial Dysfunction: Viral persistence impairs energy production in sleep-regulating neurons.
- Cortisol Dysregulation: Long COVID patients often show delayed evening cortisol peaks, which disrupt circadian rhythm and sleep onset.
🌅 Are These Conditions Reversible?
Yes—at least partially. While some patients recover naturally over time, others require targeted interventions. The reversibility depends on:
- Severity of initial infection
- Age and comorbidities
- Extent of neuroinflammation and autonomic dysfunction
Early intervention and consistent sleep hygiene practices improve outcomes. NIH studies show that immune modulation and autonomic retraining may help restore normal function.
💊 Proven Treatments to Restore Circadian Rhythms
A combination of behavioral and pharmacologic therapies has shown promise:
🧘 Behavioral & Chronobiological Interventions
| Strategy | Effect |
|---|---|
| Morning light exposure | Resets circadian rhythm, lowers cortisol |
| Fixed wake-up time | Anchors sleep-wake cycle |
| Digital curfew (1 hr before bed) | Reduces pre-sleep arousal |
| Diaphragmatic breathing | Improves heart-rate variability |
💊 Pharmacologic Therapies
| Agent | Mechanism | Use Case |
|---|---|---|
| Melatonin (2–8 mg) | Circadian entrainment | Insomnia, delayed sleep phase |
| Modafinil/Solriamfetol | Wakefulness promotion | Daytime hypersomnia |
| Low-dose naltrexone | Immune modulation | Sleep depth, fatigue |
| Prazosin | Alpha-1 antagonist | Nightmares, fragmented sleep |
| CBT-I | Cognitive restructuring | First-line for insomnia |
NIH-backed trials like RECOVER-SLEEP are actively testing these strategies in long-haul patients.
📉 Prognosis: What Lies Ahead?
The outlook varies:
- Mild cases often resolve within 6–12 months with lifestyle adjustments.
- Moderate to severe cases may require ongoing therapy and monitoring.
- Older adults and those with pre-existing neurological conditions may face longer recovery times and higher risk of cognitive decline.
Despite the challenges, most patients show improvement with structured care, and emerging therapies continue to offer hope.
🧭 Final Thoughts
COVID long-haul sleep disorders are not just about tossing and turning—they reflect deep disruptions in the brain’s regulatory systems. Understanding the etiology and targeting the right brain centers with precision therapies could be the key to restoring restful nights and functional days. As research advances, the hope is not just for symptom relief—but for full neurological recovery.