Author: John Murphy Affiliation: AshMate™ Research Division Keywords: Long COVID, brain fog, disc herniation, L3–S1, neuromechanical stability, post-viral syndrome, rehabilitation
Abstract
Long COVID, or Post-Acute Sequelae of SARS-CoV-2 Infection (PASC), presents a constellation of persistent symptoms including fatigue, cognitive dysfunction (“brain fog”), and neuromuscular instability. While its systemic effects are well-documented, its impact on patients with pre-existing spinal pathologies—particularly L3–S1 disc herniations—remains underexplored. This article synthesizes emerging neurocognitive data with biomechanical considerations, proposing a framework for understanding how long COVID may exacerbate spinal instability, impair proprioception, and complicate rehabilitation in this vulnerable cohort.
1. Introduction
The L3–S1 spinal segment plays a critical role in load-bearing, gait coordination, and pelvic-lumbar stability. Herniations in this region often result in radiculopathy, motor deficits, and altered postural mechanics. Concurrently, long COVID has emerged as a chronic neuroinflammatory condition affecting executive function, attention regulation, and neuromuscular coordination2. The intersection of these conditions raises urgent questions about compounded disability, rehabilitation efficacy, and long-term functional outcomes.
2. Neurocognitive Sequelae of Long COVID
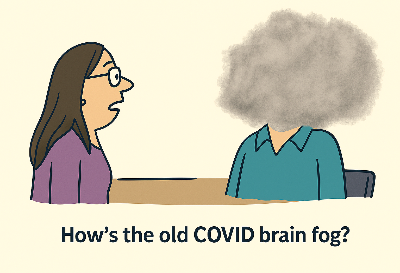
Recent studies reveal that up to 60% of long COVID patients experience persistent brain fog, characterized by:
- Impaired working memory and attention regulation2
- Slowed processing speed and executive dysfunction
- Post-exertional malaise and mental fatigue
These deficits are linked to neuroinflammation, endothelial dysfunction, and blood-brain barrier disruption. Importantly, such cognitive impairments can reduce motor planning accuracy and proprioceptive feedback—critical for patients managing spinal instability.
3. Biomechanical Vulnerability in L3–S1 Herniation
Patients with L3–S1 disc herniations often exhibit:
- Compromised lumbar lordosis and segmental instability
- Altered gait mechanics and compensatory muscle recruitment
- Reduced core activation and pelvic tilt control
These biomechanical deficits demand precise neuromuscular coordination—something long COVID may impair via central fatigue and disrupted sensorimotor integration.
4. Synergistic Impact: Cognitive Fog Meets Spinal Instability
The convergence of long COVID and L3–S1 herniation may result in:
| Symptom Domain | Long COVID Effect | L3–S1 Herniation Effect | Synergistic Impact |
|---|---|---|---|
| Proprioception | Impaired sensory integration | Nerve root compression | Increased fall risk, poor postural control |
| Motor Planning | Executive dysfunction | Muscle inhibition | Delayed response, unstable gait |
| Fatigue | Central and peripheral fatigue | Pain-induced disuse | Reduced rehab tolerance |
| Cognitive Load | Brain fog, multitasking difficulty | Pain distraction | Poor adherence to exercise protocols |
5. Rehabilitation Considerations
Rehabilitation protocols must adapt to this dual burden. Recommendations include:
- 🧘♂️ Cognitive-aware PT: Use simplified, repetitive motor tasks with minimal cognitive load.
- 🧠 Neurofeedback & pacing: Incorporate fatigue monitoring and cognitive pacing strategies.
- 🧍 Stability-first approach: Prioritize core activation and proprioceptive retraining before dynamic loading.
- 💊 Pharmacological adjuncts: Consider off-label use of guanfacine and NAC for brain fog mitigation.
6. Conclusion
Long COVID introduces a novel layer of complexity to spinal rehabilitation, particularly in patients with L3–S1 disc herniations. The interplay between cognitive dysfunction and biomechanical instability demands a multidisciplinary approach—one that integrates neurocognitive assessment, fatigue management, and precision physical therapy. As the pandemic’s chronic tail continues to unfold, targeted research and adaptive care models will be essential to restoring function and quality of life in this vulnerable population.