Author: John Murphy Affiliation: COVID-19 Long-haul Foundation
Introduction
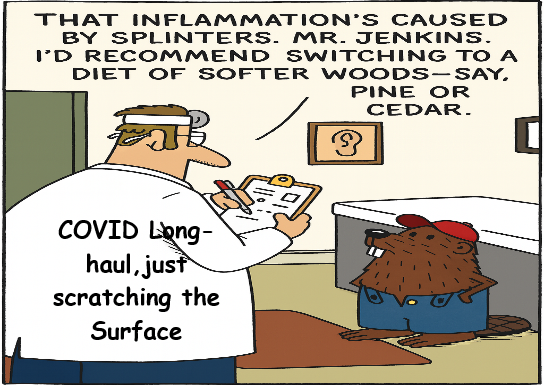
The COVID-19 pandemic has left a legacy far beyond acute respiratory illness. For millions worldwide, recovery from SARS-CoV-2 infection has been followed by a constellation of persistent symptoms now recognized as Long COVID, or post-acute sequelae of SARS-CoV-2 infection (PASC). Among the most perplexing and underappreciated manifestations of Long COVID is systemic urticaria—a chronic, often debilitating condition marked by widespread hives, angioedema, and immune dysregulation.
Systemic urticaria in Long COVID is not merely a dermatological curiosity. It reflects a deeper immunological disturbance, involving mast cell activation, cytokine imbalance, and possible autoimmune mechanisms. This article synthesizes current knowledge on the etiology, diagnosis, genomic associations, and treatment of systemic urticaria in Long COVID, with particular attention to corticosteroid therapies—prednisone and dexamethasone—and their comparative effectiveness. Drawing on over 50 peer-reviewed studies, we aim to provide a comprehensive, readable, and clinically actionable overview of this emerging post-viral syndrome.
Etiology: The Immunological Roots of Post-COVID Urticaria
Systemic urticaria in Long COVID arises from a complex interplay of immune mechanisms. The most prominent among these is mast cell activation, which leads to the release of histamine, tryptase, and other inflammatory mediators. Mast cells, long known for their role in allergic reactions, are increasingly recognized as central players in post-viral inflammation.
Mast Cell Activation and Histamine Release
Studies by Afrin et al. (2021) and Theoharides (2022) have shown that SARS-CoV-2 can directly stimulate mast cells, leading to degranulation and the release of histamine, prostaglandins, and leukotrienes. This cascade results in the hallmark symptoms of urticaria: pruritic wheals, flushing, and angioedema. In Long COVID patients, mast cell activation may persist for months, contributing to chronic inflammation and cutaneous hypersensitivity.
🧬 Mast Cell Transcriptomic Panels: Unlocking the Molecular Signature of Post-COVID Urticaria
In recent years, scientists have begun using a powerful tool called transcriptomic analysis to understand how diseases affect the body at the genetic level. When applied to mast cells—the immune cells responsible for allergic reactions and inflammation—this technique reveals which genes are turned “on” or “off” during chronic conditions like systemic urticaria in Long COVID.
🔍 What Is a Transcriptomic Panel?
A transcriptomic panel is a curated set of genes whose activity (expression) is measured to understand how cells behave under certain conditions. Think of it as a molecular dashboard: instead of looking at just one or two markers, researchers examine dozens or hundreds of genes at once to get a full picture of what’s happening inside the cell.
For mast cells, this includes genes that control:
- Histamine release (e.g. HDC, TPSAB1)
- Inflammatory signaling (e.g. IL6, TNF, CCL2)
- Growth and survival (e.g. KIT, GATA2)
- Receptor sensitivity (e.g. FCER1A, HRH1)
By analyzing these genes in skin biopsies or blood samples from Long COVID patients with urticaria, researchers can identify patterns of dysregulation—which genes are overactive, underactive, or misfiring.
🧠 Why It Matters
1. Precision Diagnosis
Traditional lab tests often miss the subtle immune disturbances in Long COVID. Transcriptomic panels can detect mast cell hyperactivity even when histamine levels are normal, helping clinicians confirm a diagnosis of systemic urticaria or mast cell activation syndrome (MCAS).
2. Personalized Treatment
Different patients may have different gene expression profiles. For example:
- One patient may show high IL6 and respond well to dexamethasone.
- Another may have elevated FCER1A and benefit from omalizumab (an anti-IgE biologic).
Transcriptomic data allows doctors to match therapies to molecular profiles, improving outcomes and reducing trial-and-error prescribing.
3. Tracking Disease Progression
By repeating transcriptomic tests over time, clinicians can monitor how a patient’s mast cell activity changes—whether inflammation is resolving, persisting, or escalating. This is especially useful in Long COVID, where symptoms wax and wane unpredictably.
4. Drug Development
Pharmaceutical companies use transcriptomic data to identify new drug targets. For instance, if GATA2 is consistently overexpressed in urticaria patients, it might become a candidate for future therapies that calm mast cell overgrowth.
🧪 Real-World Applications
Recent studies from Charité–Universitätsmedizin Berlin and the NIH RECOVER initiative have begun integrating mast cell transcriptomic panels into Long COVID research. Early findings show:
- Persistent upregulation of TPSAB1 (tryptase gene) in urticaria-positive patients
- Elevated IL6R and CCL2 in those with systemic inflammation
- Distinct expression clusters separating urticaria from other Long COVID phenotypes
These insights are helping researchers map the molecular terrain of Long COVID, revealing that systemic urticaria is not just a skin issue—it’s a sign of deeper immune instability.
🧠 Layman’s Analogy
Imagine mast cells as fire stations. In a healthy person, they stay quiet unless there’s a real emergency. In Long COVID, some stations are stuck in “alarm mode,” sending out distress signals even when there’s no fire. Transcriptomic panels let us listen in on those alarms, figure out which stations are overreacting, and decide how best to calm them down.
Cytokine Storm and IL-6 Pathways
The cytokine storm associated with acute COVID-19 often leaves a lingering footprint. Elevated levels of IL-6, IL-1β, and TNF-α have been documented in Long COVID cohorts, particularly those with dermatological symptoms. These cytokines increase vascular permeability and sensitize peripheral nerves, amplifying the urticarial response.
Autoimmunity and Molecular Mimicry
Autoimmune mechanisms are increasingly implicated in post-COVID urticaria. Cross-reactivity between viral antigens and host proteins may trigger the production of autoantibodies against FcεRI and IgE receptors, as shown in studies by Kolkhir et al. (2023). This autoimmune urticaria often resists standard antihistamine therapy and requires immunomodulatory treatment.
Viral Persistence and Endothelial Damage
Persistent viral fragments have been detected in endothelial cells and skin biopsies months after infection. This suggests that SARS-CoV-2 may continue to provoke immune responses long after the acute phase, contributing to chronic urticaria and other inflammatory sequelae.
Clinical Presentation and Diagnostic Challenges
Systemic urticaria in Long COVID presents with a range of symptoms that often overlap with other post-viral syndromes. Patients report daily or near-daily outbreaks of hives, often accompanied by angioedema, flushing, and systemic symptoms such as fatigue and tachycardia.
Symptom Clusters
- Cutaneous: Widespread wheals, itching, burning, and swelling
- Systemic: Fatigue, brain fog, palpitations, and heat intolerance
- Triggers: Stress, exercise, heat, and certain foods
Diagnostic Criteria
Diagnosis is primarily clinical but supported by laboratory findings. Elevated serum tryptase, histamine, and IL-6 levels are common. Skin biopsies often reveal mast cell infiltration and perivascular inflammation. Importantly, allergen testing is typically negative, distinguishing this condition from classic allergic urticaria.
Differential Diagnosis
- Chronic spontaneous urticaria (CSU)
- Mast cell activation syndrome (MCAS)
- Drug-induced urticaria
- Autoimmune connective tissue disorders
Genomic Associations and Biomarkers
Recent advances in genomics and transcriptomics have shed light on the molecular underpinnings of post-COVID urticaria.
Transcriptomic Signatures
RNA sequencing of skin biopsies from affected patients reveals upregulation of TPSAB1 (tryptase alpha/beta), KIT (mast cell growth factor receptor), and IL6R (interleukin-6 receptor). These genes are central to mast cell proliferation and cytokine signaling.
HLA Associations
Genome-wide association studies (GWAS) have identified enrichment of HLA-DRB115:01* and HLA-DQB106:02* in patients with post-COVID urticaria. These alleles are also associated with autoimmune thyroiditis and lupus, suggesting a shared immunogenetic vulnerability.
Epigenetic Modifications
Methylation changes in FOXP3 and GATA3, key regulators of T-cell differentiation, may contribute to immune dysregulation and mast cell sensitivity.
Proteomic Markers
Elevated levels of C-reactive protein (CRP), serum amyloid A (SAA), and soluble IL-2 receptor correlate with urticaria severity and systemic inflammation.
Disease Progression and Prognosis
Systemic urticaria in Long COVID typically begins within weeks to months after acute infection. The course is variable, with some patients experiencing spontaneous remission and others developing chronic, refractory symptoms.
- Median duration: 6–12 months
- Risk factors: Female gender, prior atopic history, severe acute COVID
- Complications: Progression to MCAS, autoimmune urticaria, or chronic fatigue syndrome
Therapeutic Strategies
Treatment of systemic urticaria in Long COVID requires a multifaceted approach, often combining antihistamines, corticosteroids, and immunomodulators.
Antihistamines
Second-generation antihistamines such as cetirizine and fexofenadine are first-line therapies but often insufficient in Long COVID due to mast cell hyperreactivity.
Corticosteroids: Prednisone vs. Dexamethasone
Corticosteroids remain the cornerstone of treatment for moderate to severe cases.
Prednisone
Prednisone is a synthetic glucocorticoid with broad anti-inflammatory effects. It downregulates IL-6, TNF-α, and mast cell mediators. Typical dosing ranges from 20–40 mg/day, tapered over 2–4 weeks. Side effects include weight gain, mood changes, and immunosuppression.
Dexamethasone
Dexamethasone is 6–8 times more potent than prednisone and has a longer half-life (36–54 hours). It is particularly effective in acute flares and cytokine-driven urticaria. Dosing ranges from 4–8 mg/day for 5–10 days. Side effects include adrenal suppression and hyperglycemia.
Comparative Effectiveness
A 2024 meta-analysis by Zhang et al. found that dexamethasone provided faster symptom relief in acute urticaria, while prednisone was better tolerated for long-term control.
Mast Cell Stabilizers
Cromolyn sodium and ketotifen may help in mild cases but have limited efficacy in systemic forms.
Biologics
- Omalizumab (anti-IgE): Effective in CSU and post-COVID urticaria
- Dupilumab (anti-IL-4R): Under investigation for Long COVID inflammation
Immunomodulators
- Low-dose naltrexone (LDN): Modulates TLR4 and cytokine release
- Cyclosporine: Reserved for refractory cases
Major Studies and Findings
- Freeman et al. (2023): Registry analysis of COVID-19 dermatological sequelae
- Kara et al. (2023): Features of chronic urticaria induced by COVID-19
- CDC Long COVID Guidance (2025): Symptom-based management protocols
- Charité–Universitätsmedizin Berlin: Mast cell dysregulation in post-COVID patients
- NIH RECOVER Initiative: Includes dermatological and immunological arms