Authors: Narayanappa Amruta,a Wesley H. Chastain,a Meshi Paz,a Rebecca J. Solch,b Isabel C. Murray-Brown,a Jaime B. Befeler,a Timothy E. Gressett,a Michele T. Longo,b,c Elizabeth B. Engler-Chiurazzi,a,c and Gregory Bixa,b,c,*
Abstract
SARS-CoV-2 is a novel coronavirus that severely affects the respiratory system, is the cause of the COVID-19 pandemic, and is projected to result in the deaths of 2 million people worldwide. Recent reports suggest that SARS-CoV-2 also affects the central nervous system along with other organs. COVID-19-associated complications are observed in older people with underlying neurological conditions like stroke, Alzheimer’s disease, and Parkinson’s disease. Hence, we discuss SARS-CoV-2 viral replication and its inflammation-mediated infection. This review also focuses on COVID-19 associated neurological complications in individuals with those complications as well as other groups of people. Finally, we also briefly discuss the current therapies available to treat patients, as well as ongoing available treatments and vaccines for effective cures with a special focus on the therapeutic potential of a small 5 amino acid peptide (PHSCN), ATN-161, that inhibits SARS-CoV-2 spike protein binding to both integrin α5β1 and α5β1/hACE2.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the agent causative of coronavirus disease 2019 (COVID-19), is a respiratory pathogen that emerged in late 2019 [1]. As of late January 2021, it has infected 97 million people worldwide, and in the United States alone it has infected 25 million people with 421,000 deaths have been reported (https://www.cdc.gov/). Symptoms of COVID-19 include fever followed by cough in most patients [2]. Additional symptoms include myalgia, diarrhea, and constipation at the onset of illness. Though a mortality rate of greater than 20 % is seen in older people with underlying medical conditions such as hypertension, diabetes, lung, and cardiac disease [3], the majority of cases do not require intensive intervention and most infected patients are expected to make a full recovery from effects of the acute lung infection. In most cases, viral replication occurs in the upper respiratory epithelia and is transmitted effectively via mediating angiotensin-converting enzyme 2 (ACE2), which increases immune responses by cytokine storm [4].
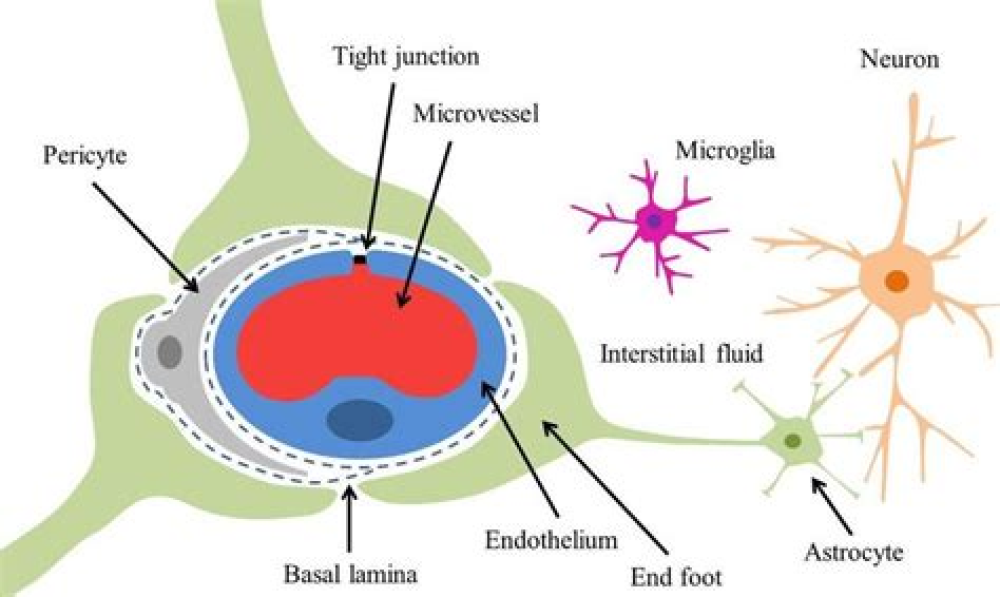
Interestingly, coronaviruses are associated with central nervous system (CNS) diseases such as disseminated encephalomyelitis, multiple sclerosis, febrile seizures, and encephalitis epilepsy [3,[5], [6], [7]]. Studies have shown that human coronavirus OC43 (HCoV−OC43) can access the CNS through axonal transport and viral migration through neurons in the brain [8] and others have reported that SARS-CoV may enter the CNS through both blood circulation (blood-brain barrier, BBB) and olfactory bulb [[9], [10], [11]]. The inflammatory and immune responses to SARS-CoV-2 results in immune system changes, enhancing lung injury and CNS complications. Importantly, patients hospitalized with COVID-19 and concurrent neurological problems, mainly stroke and confusion, have a higher risk of dying than other patients. Thus, in addition to developing interventions that prevent infection and limit mortality from SARS-CoV-2, additional work is needed to characterize and ultimately treat these CNS manifestations of COVID-19 complications.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7894219/