Authors: Eric J. Kremer1,∗
Main Text
Most of us might be surprised by the rudimentary scientific rationale prevalent in the field of vaccine research just 50 years ago. For over a century after Louis Pasteur’s vaccine against rabies, approaches usually consisted of inactivating a virus, injecting it, and seeing if it protected the host. Unlike today, interactions between vaccinologists and immunologists to improve vaccine efficacy were marginal.
With the rise of molecular biology, vaccine designs became more nuanced and the use of viral vectors emerged. An example is the evolution and checkered history of vaccines based on adenoviruses (Ads). Live Ad types 4 (Ad4) and 7 (Ad7) have been used in North American military recruits since the 1950s to prevent severe respiratory illness.1 Similarly, dogs in western countries are vaccinated with an attenuated canine Ad type 2 (CAV-2) to prevent infection of the more virulent CAV-1.
Many of the first replication-defective Ad “vectors” in the early 1980s were vaccines. The original Ad vaccine design was relatively simple: delete a region of the viral genome that the virus needs to propagate, provide these functions via transcomplementing cells (e.g., Frank Graham’s 293 cells) so that one could grow the vaccine, and then insert into the virus genome an expression cassette encoding the targeted epitopes.
Fast forward to 2020. The SARS-CoV-2 pandemic may be headed toward historic proportions—although still far from the 1918 Spanish flu (50 million deaths) and AIDS (35 million deaths)—inflicting havoc on families, communities, and economies and overwhelming health care facilities. Clearly, we need a vaccine. Are Ad-based vaccines targeting the SARS-CoV-2 spike and capsid proteins our best bet? After almost 70 years of working with Ads, their biochemical properties are well characterized: Ads are simple to make (in ∼2 weeks a graduate student could generate enough of a novel Ad vaccine to treat a thousand mice and dozens of monkeys), easy to purify to high titer, genetically stable, easily stockpiled, relatively inexpensive, and can be delivered via aerosol, oral, intradermal, and intramuscular routes. The aerosol route is particularly relevant when targeting a respiratory virus because inducing protective immune responses that home to the tissue where infections will occur is strategically important. It is also worth noting that Ad-based vaccines tend to induce B cell and T cell responses.
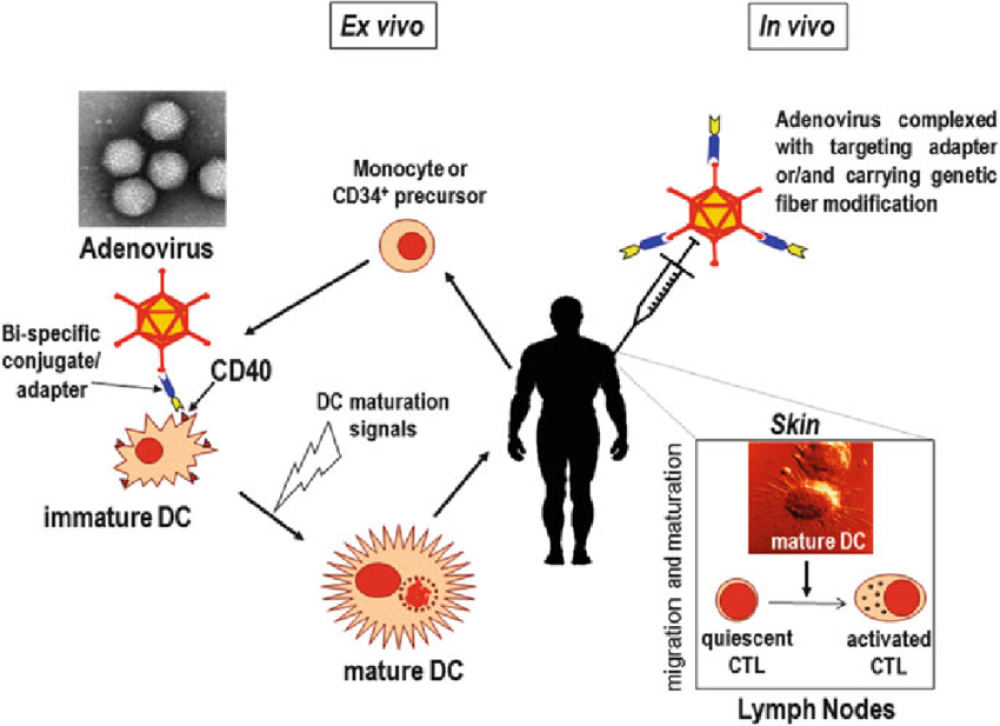
Hundreds of millions of euros, dollars, and yen have been invested in advancing Ad-based vaccines. These advances include production and purification methods, genetic incorporation of epitopes into the capsid so that mononuclear phagocytes present these antigens via major histocompatibility complex (MHC) class I and II pathways, cloaking the capsid with polymers/shields or using Ad types with a lower level of seroprevalence to prevent neutralization by antibodies (NAbs) to common types found in many individuals, retargeting the vector to professional antigen-presenting cells, using helper-dependent vectors (so that the vector-infected cell only expresses the target epitopes and not Ad antigens), and single-cycle replication of vaccines to produce massive amounts of antigens. Each tweak, alone or in combination with others, has improved vaccine efficacy in preclinical trials.
As SARS-CoV-2 became a pandemic, it is astonishing that, in the case of the Ad-based vaccine frontrunners, little has changed from the basic design of 40 years ago. Some used the well-trodden path of an Ad5-based vaccine, while others switched to human (e.g., Ad26) or simian (monkey and gorilla) Ads that have low seroprevalence in Europe and North America (but not necessarily in Africa or Asia).2 Conceptually, Ad type switching to avoid NAbs is at least 30 years old. The advent of simian Ad vaccines was not developed following a rigorous testing of all of the >200 different Ad types but was most likely the result of intellectual property issues and the ability to produce simian Ads in good manufacturing practice (GMP)-compliant cells. One presumes that subsequent rounds of Ad-based coronavirus disease 2019 (COVID-19) vaccine candidates will be more sophisticated.
Should we go “all in” on an Ad-based vaccine against SARS-CoV-2? The first issue is safety. There are few drugs or biologicals that do not have side effects or cause adverse reactions. Weighing the advantages versus disadvantages during the current pandemic can be idiosyncratic, and the strength of the reasoning varies by population, culture, religious beliefs, and bizarrely (for those of us outside the USA) even political affiliation. Current criteria limit the window to identify adverse reactions to 2 months. In addition to swelling and pain at the injection site, common to some vaccines, Ad-based vaccine adverse effects include fever, pneumonia, diarrhea, transient neutropenia and lymphopenia, fatigue, labored breathing, headaches, liver damage, and fasting hyperglycaemia. Rare but grave adverse reactions include neuropathies such as Bell’s palsy, Guillain-Barré syndrome, gait disturbance, and transverse myelitis, an inflammatory condition in the spinal cord.
For More Information: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7546260/