Authors: Maxime Taquet, John R Geddes, Masud Husain, Sierra Luciano, Paul J Harrison
Summary
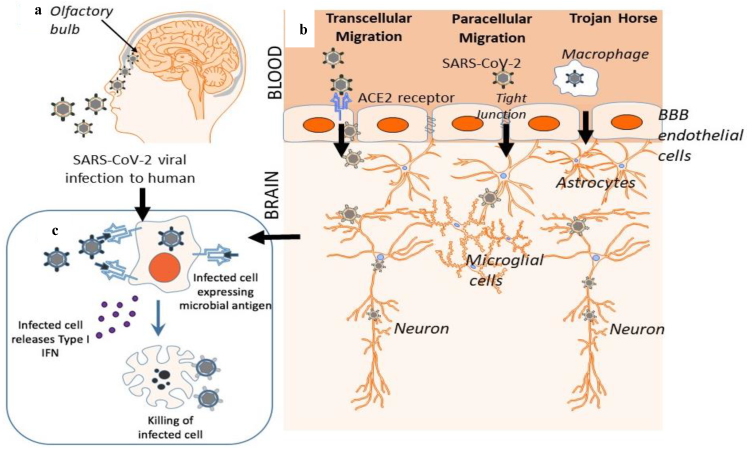
Background Neurological and psychiatric sequelae of COVID-19 have been reported, but more data are needed to adequately assess the effects of COVID-19 on brain health. We aimed to provide robust estimates of incidence rates and relative risks of neurological and psychiatric diagnoses in patients in the 6 months following a COVID-19 diagnosis. Methods For this retrospective cohort study and time-to-event analysis, we used data obtained from the TriNetX electronic health records network (with over 81 million patients). Our primary cohort comprised patients who had a COVID-19 diagnosis; one matched control cohort included patients diagnosed with influenza, and the other matched control cohort included patients diagnosed with any respiratory tract infection including influenza in the same period. Patients with a diagnosis of COVID-19 or a positive test for SARS-CoV-2 were excluded from the control cohorts. All cohorts included patients older than 10 years who had an index event on or after Jan 20, 2020, and who were still alive on Dec 13, 2020. We estimated the incidence of 14 neurological and psychiatric outcomes in the 6 months after a confirmed diagnosis of COVID-19: intracranial haemorrhage; ischaemic stroke; parkinsonism; Guillain-Barré syndrome; nerve, nerve root, and plexus disorders; myoneural junction and muscle disease; encephalitis; dementia; psychotic, mood, and anxiety disorders (grouped and separately); substance use disorder; and insomnia. Using a Cox model, we compared incidences with those in propensity score-matched cohorts of patients with influenza or other respiratory tract infections. We investigated how these estimates were affected by COVID-19 severity, as proxied by hospitalisation, intensive therapy unit (ITU) admission, and encephalopathy (delirium and related disorders). We assessed the robustness of the differences in outcomes between cohorts by repeating the analysis in different scenarios. To provide benchmarking for the incidence and risk of neurological and psychiatric sequelae, we compared our primary cohort with four cohorts of patients diagnosed in the same period with additional index events: skin infection, urolithiasis, fracture of a large bone, and pulmonary embolism. Findings Among 236 379 patients diagnosed with COVID-19, the estimated incidence of a neurological or psychiatric diagnosis in the following 6 months was 33·62% (95% CI 33·17–34·07), with 12·84% (12·36–13·33) receiving their first such diagnosis. For patients who had been admitted to an ITU, the estimated incidence of a diagnosis was 46·42% (44·78–48·09) and for a first diagnosis was 25·79% (23·50–28·25). Regarding individual diagnoses of the study outcomes, the whole COVID-19 cohort had estimated incidences of 0·56% (0·50–0·63) for intracranial haemorrhage, 2·10% (1·97–2·23) for ischaemic stroke, 0·11% (0·08–0·14) for parkinsonism, 0·67% (0·59–0·75) for dementia, 17·39% (17·04–17·74) for anxiety disorder, and 1·40% (1·30–1·51) for psychotic disorder, among others. In the group with ITU admission, estimated incidences were 2·66% (2·24–3·16) for intracranial haemorrhage, 6·92% (6·17–7·76) for ischaemic stroke, 0·26% (0·15–0·45) for parkinsonism, 1·74% (1·31–2·30) for dementia, 19·15% (17·90–20·48) for anxiety disorder, and 2·77% (2·31–3·33) for psychotic disorder. Most diagnostic categories were more common in patients who had COVID-19 than in those who had influenza (hazard ratio [HR] 1·44, 95% CI 1·40–1·47, for any diagnosis; 1·78, 1·68–1·89, for any first diagnosis) and those who had other respiratory tract infections (1·16, 1·14–1·17, for any diagnosis; 1·32, 1·27–1·36, for any first diagnosis). As with incidences, HRs were higher in patients who had more severe COVID-19 (eg, those admitted to ITU compared with those who were not: 1·58, 1·50–1·67, for any diagnosis; 2·87, 2·45–3·35, for any first diagnosis). Results were robust to various sensitivity analyses and benchmarking against the four additional index health events. Interpretation Our study provides evidence for substantial neurological and psychiatric morbidity in the 6 months after COVID-19 infection. Risks were greatest in, but not limited to, patients who had severe COVID-19. This information could help in service planning and identification of research priorities. Complementary study designs, including prospective cohorts, are needed to corroborate and explain these findings. Funding National Institute for Health Research (NIHR) Oxford Health Biomedical Research Centre. Copyright © 2021 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license. Articles www.thelancet.com/psychiatry Vol 8 May 2021 417 Introduction Since the COVID-19 pandemic began on March 11, 2020, there has been concern that survivors might be at an increased risk of neurological disorders. This concern, initially based on findings from other coronaviruses,1 was followed rapidly by case series,2–4 emerging evidence of COVID-19 CNS involvement,5–7 and the identification of mechanisms by which this could occur.8–11 Similar concerns have been raised regarding psychiatric sequelae of COVID-19,12,13 with evidence showing that survivors are indeed at increased risk of mood and anxiety disorders in the 3 months after infection.14 However, we need large scale, robust, and longer term data to properly identify and quantify the consequences of the COVID-19 pandemic on brain health. Such information is required both to plan services and identify research priorities. In this study, we used an electronic health records network to investigate the incidence of neurological and psychiatric diagnoses in survivors in the 6 months after documented clinical COVID-19 infection, and we compared the associated risks with those following other health conditions. We explored whether the severity of COVID-19 infection, as proxied by hospitalization, intensive therapy unit (ITU) admission, and encephalopathy, affects these risks. We also assessed the trajectory of hazard ratios (HRs) across the 6-month period. Methods Study design and data collection For this retrospective cohort study, we used The TriNetX Analytics Network, a federated network recording anonymized data from electronic health records in 62 health-care organizations, primarily in the USA, comprising 81 million patients. Available data include demographics, diagnoses (using codes from ICD-10), medications, procedures, and measurements (eg, blood pressure and body-mass index). The health-care organizations are a mixture of hospitals, primary care, and specialist providers, contributing data from uninsured and insured patients. These organizations warrant that they have all necessary rights, consents, approvals, and authority to provide the data to TriNetX, so long as their name remains anonymous as a data source and their data are used for research purposes. By use of the TriNetX user interface, cohorts can be created on the basis of inclusion and exclusion criteria, matched for confounding variables with a built-in propensity score-matching algorithm, and compared for outcomes of interest over specified time periods. Additional details about TriNetX, its data, provenance, and functionalities, are presented in the appendix (pp 1–2). Cohorts The primary cohort was defined as all patients who had a confirmed diagnosis of COVID-19 (ICD-10 code U07.1). We also constructed two matched control cohorts: patients diagnosed with influenza (ICD-10 codes J09–11) and patients diagnosed with any respiratory tract infection including influenza (ICD-10 codes J00–06, J09–18, or J20–22). We excluded patients with a diagnosis of COVID-19 or a positive test for SARS-CoV-2 from the control cohorts. We refer to the diagnosis of COVID-19 (in the primary cohort) and influenza or other respiratory See Online for appendix For the TriNetX Analytics Network see www.trinetx.com Research in context Evidence before this study We searched Web of Science and Medline on Aug 1 and Dec 31, 2020, for studies in English, with the terms “(COVID-19 OR SARS-CoV2 OR SARS-CoV-2) AND (psychiatry* or neurology*) AND (incidence OR epidemiology* OR ‘systematic review’ or ‘meta-analysis’)”. We found case series and reviews of series reporting neurological and neuropsychiatric disorders during acute COVID-19 illness. We found one large electronic health records study of the psychiatric sequelae in the 3 months after a COVID-19 diagnosis. It reported an increased risk for anxiety and mood disorders and dementia after COVID-19 compared with a range of other health events; the study also reported the incidence of each disorder. We are not aware of any large-scale data regarding the incidence or relative risks of neurological diagnoses in patients who had recovered from COVID-19. Added value of this study To our knowledge, we provide the first meaningful estimates of the risks of major neurological and psychiatric conditions in the 6 months after a COVID-19 diagnosis, using the electronic health records of over 236000 patients with COVID-19. We report their incidence and hazard ratios compared with patients who had had influenza or other respiratory tract infections. We show that both incidence and hazard ratios were greater in patients who required hospitalization or admission to the intensive therapy unit (ITU), and in those who had encephalopathy (delirium and other altered mental states) during the illness compared with those who did not. Implications of all the available evidence COVID-19 was robustly associated with an increased risk of neurological and psychiatric disorders in the 6 months after a diagnosis. Given the size of the pandemic and the chronicity of many of the diagnoses and their consequences (eg, dementia, stroke, and intracranial hemorrhage), substantial effects on health and social care systems are likely to occur. Our data provide important evidence indicating the scale and nature of services that might be required. The findings also highlight the need for enhanced neurological follow-up of patients who were admitted to ITU or had encephalopathy during their COVID-19 illness. Articles 418 www.thelancet.com/psychiatry Vol 8 May 2021 tract infections (in the control cohorts) as index events. The cohorts included all patients older than 10 years who had an index event on or after Jan 20, 2020 (the date of the first recorded COVID-19 case in the USA), and who were still alive at the time of the main analysis (Dec 13, 2020). Additional details on cohorts are provided in the appendix (pp 2–3). Covariates We used a set of established and suspected risk factors for COVID-19 and for more severe COVID-19 illness:15,16 age, sex, race, ethnicity, obesity, hypertension, diabetes, chronic kidney disease, asthma, chronic lower respiratory diseases, nicotine dependence, substance use disorder, ischemic heart disease and other forms of heart disease, socioeconomic deprivation, cancer (and hematological cancer in particular), chronic liver disease, stroke, dementia, organ transplant, rheumatoid arthritis, lupus, psoriasis, and disorders involving an immune mechanism. To capture these risk factors in patients’ health records, we used 55 variables. More details, including ICD-10 codes, are provided in the appendix (pp 3–4). Cohorts were matched for all these variables, as described in the following subsections. Outcomes We investigated neurological and psychiatric sequelae of COVID-19 in terms of 14 outcomes occurring 1–180 days after the index event: intracranial hemorrhage (ICD-10 codes I60–62); ischemic stroke (I63); Parkinson’s disease and parkinsonism (G20–21); Guillain-Barré syndrome (G61.0); nerve, nerve root, and plexus disorders (G50–59); myoneural junction and muscle disease (neuromuscular disorders; G70–73); encephalitis (G04, G05, A86, or A85.8); dementia (F01–03, G30, G31.0, or G31.83); psychotic, mood, and anxiety disorders (F20–48), as well as each category separately; substance use disorder (F10–19), and insomnia (F51.0 or G47.0). For outcomes that are chronic illnesses (eg, dementia or Parkinson’s disease), we excluded patients who had the diagnosis before the index event. For outcomes that All patients Patients without hospitalization Patients with hospitalization Patients with ITU admission Patients with encephalopathy Cohort size 236379 (100·0%) 190077 (100·0%) 46302 (100·0%) 8945 (100·0%) 6229 (100·0%) Demographics Age, years 46 (19·7) 43·3 (19·0) 57 (18·7) 59·1 (17·3) 66·7 (17·0) Sex Male 104015 (44·0%) 81 512 (42·9%) 22 503 (48·6%) 5196 (58·1%) 3307 (53·1%) Female 131460 (55·6%) 107 730 (56·7%) 23 730 (51·3%) 3743 (41·8%) 2909 (46·7%) Other 904 (0·4%) 835 (0·4%) 69 (0·1%) 10 (0·1%) 13 (0·2%) Race White 135 143 (57·2%) 109635 (57·7%) 25 508 (55·1%) 4918 (55·0%) 3331 (53·5%) Black or African American 44459 (18·8%) 33868 (17·8%) 10591 (22·9%) 2184 (24·4%) 1552 (24·9%) Unknown 48085 (20·3%) 39841 (21·0%) 8244 (17·8%) 1457 (16·3%) 1071 (17·2%) Ethnicity Hispanic or Latino 37 772 (16·0%) 29155 (15·3%) 8617 (18·6%) 2248 (25·1%) 895 (14·4%) Not Hispanic or Latino 134075 (56·7%) 106844 (56·2%) 27 231 (58·8%) 5041 (56·4%) 3873 (62·2%) Unknown 64532 (27·3%) 54078 (28·5%) 10454 (22·6%) 1656 (18·5%) 1461 (23·5%) Comorbidities Overweight and obesity 42871 (18·1%) 30198 (15·9%) 12673 (27·4%) 3062 (34·2%) 1838 (29·5%) Hypertensive disease 71014 (30·0%) 47 516 (25·0%) 23498 (50·7%) 5569 (62·3%) 4591 (73·7%) Type 2 diabetes 36696 (15·5%) 22 518 (11·8%) 14178 (30·6%) 3787 (42·3%) 2890 (46·4%) Asthma 25 104 (10·6%) 19834 (10·4%) 5270 (11·4%) 1132 (12·7%) 755 (12·1%) Nicotine dependence 17 105 (7·2%) 12639 (6·6%) 4466 (9·6%) 1042 (11·6%) 803 (12·9%) Substance use disorder 24870 (10·5%) 18173 (9·6%) 6697 (14·5%) 1620 (18·1%) 1316 (21·1%) Ischemic heart diseases 21082 (8·9%) 11815 (6·2%) 9267 (20·0%) 2460 (27·5%) 2200 (35·3%) Other forms of heart disease 42431 (18·0%) 26066 (13·7%) 16365 (35·3%) 4678 (52·3%) 3694 (59·3%) Chronic kidney disease 15908 (6·7%) 8345 (4·4%) 7563 (16·3%) 1941 (21·7%) 1892 (30·4%) Neoplasms 45 255 (19·1%) 34362 (18·1%) 10893 (23·5%) 2339 (26·1%) 1793 (28·8%) Data are n (%) or mean (SD). Only characteristics with a prevalence higher than 5% in the whole population are displayed. Additional baseline characteristics are presented in the appendix (pp 25–27). ITU=intensive therapy unit. Table 1: Baseline characteristics for the whole COVID-19 cohort and for the non-hospitalization, hospitalization, ITU admission, and encephalopathy cohorts during the illness Articles www.thelancet.com/psychiatry Vol 8 May 2021 419 tend to recur or relapse (eg, ischaemic strokes or psychiatric diagnoses), we estimated separately the incidence of first diagnoses (ie, excluding those who had a diagnosis before the index event) and the incidence of any diagnosis (ie, including patients who had a diagnosis at some point before the index event). For other outcomes (eg, Guillain-Barré syndrome), we estimated the incidence of any diagnosis. More details, and a full list of ICD-10 codes, are provided in the appendix (pp 4–5). Finally, to assess the overall risk of neurological and psychiatric outcomes after COVID-19, we estimated the incidence of any of the 14 outcomes, and the incidence of a first diagnosis of any of the outcomes. This is lower than the sum of incidences of each outcome because some patients had more than one diagnosis. Secondary analyses We investigated whether the neurological and psychiatric sequelae of COVID-19 were affected by the severity of the illness. The incidence of outcomes was estimated separately in four subgroups: first, in those who had required hospitalization within a time window from 4 days before their COVID-19 diagnosis (taken to be the time it might take between clinical presentation and confirmation) to 2 weeks afterwards; second, in those who had not required hospitalization during that window; third, in those who had been admitted to an intensive therapy unit (ITU) during that window; and fourth, in those who were diagnosed with delirium or other forms of altered mental status during that window; we use the term encephalopathy to describe this group of patients (appendix p 5).17,18 Differences in outcome incidence between these subgroups might reflect differences in their baseline characteristics. Therefore, for each outcome, we estimated the HR between patients requiring hospitalization (or ITU) and a matched cohort of patients not requiring hospitalization (or ITU), and between patients with encephalopathy and a matched cohort of patients without encephalopathy. Finally, HRs were calculated for patients who had not required hospitalization for COVID-19, influenza, or other respiratory tract infections. To provide benchmarks for the incidence and risk of neurological and psychiatric sequelae, patients after COVID-19 were compared with those in four additional matched cohorts of patients diagnosed with health events selected to represent a range of acute presentations during the same time period. These additional four index events were skin infection, urolithiasis, fracture of a large bone, and pulmonary embolism. More details are presented in the appendix (pp 5–6). We assessed the robustness of the differences in outcomes between cohorts by repeating the analysis in three scenarios: one including patients who had died by All patients Patients without hospitalization Patients with hospitalization Patients with ITU admission Patients with encephalopathy Intracranial hemorrhage (any) 0·56% (0·50–0·63) 0·31% (0·25–0·39) 1·31% (1·14–1·52) 2·66% (2·24–3·16) 3·61% (2·97–4·39) Intracranial hemorrhage (first) 0·28% (0·23–0·33) 0·14% (0·10–0·20) 0·63% (0·50–0·80) 1·05% (0·79–1·40) 1·19% (0·82–1·70) Ischemic stroke (any) 2·10% (1·97–2·23) 1·33% (1·22–1·46) 4·38% (4·05–4·74) 6·92% (6·17–7·76) 9·35% (8·23–10·62) Ischemic stroke (first) 0·76% (0·68–0·85) 0·43% (0·36–0·52) 1·60% (1·37–1·86) 2·82% (2·29–3·47) 3·28% (2·51–4·27) Parkinsonism 0·11% (0·08–0·14) 0·07% (0·05–0·12) 0·20% (0·15–0·28) 0·26% (0·15–0·45) 0·46% (0·28–0·78) Guillain-Barré syndrome 0·08% (0·06–0·11) 0·05% (0·03–0·07) 0·22% (0·15–0·32) 0·33% (0·21–0·54) 0·48% (0·20–1·14) Nerve, nerve root, or plexus disorders 2·85% (2·69–3·03) 2·69% (2·51–2·89) 3·35% (3·02–3·72) 4·24% (3·58–5·03) 4·69% (3·81–5·77) Myoneural junction or muscle disease 0·45% (0·40–0·52) 0·16% (0·12–0·20) 1·24% (1·05–1·46) 3·35% (2·76–4·05) 3·27% (2·54–4·21) Encephalitis 0·10% (0·08–0·13) 0·05% (0·03–0·08) 0·24% (0·17–0·33) 0·35% (0·19–0·64) 0·64% (0·39–1·07) Dementia 0·67% (0·59–0·75) 0·35% (0·29–0·43) 1·46% (1·26–1·71) 1·74% (1·31–2·30) 4·72% (3·80–5·85) Mood, anxiety, or psychotic disorder (any) 23·98% (23·58–24·38) 23·59% (23·12–24·07) 24·50% (23·76–25·26) 27·78% (26·33–29·29) 36·25% (34·16–38·43) Mood, anxiety, or psychotic disorder (first) 8·63% (8·28–8·98) 8·15% (7·75–8·57) 8·85% (8·22–9·52) 12·68% (11·28–14·24) 12·96% (11·13–15·07) Mood disorder (any) 13·66% (13·35–13·99) 13·10% (12·73–13·47) 14·69% (14·09–15·32) 15·43% (14·27–16·68) 22·52% (20·71–24·47) Mood disorder (first) 4·22% (3·99–4·47) 3·86% (3·60–4·14) 4·49% (4·05–4·99) 5·82% (4·86–6·97) 8·07% (6·56–9·90) Anxiety disorder (any) 17·39% (17·04–17·74) 17·51% (17·09–17·93) 16·40% (15·76–17·06) 19·15% (17·90–20·48) 22·43% (20·65–24·34) Anxiety disorder (first) 7·11% (6·82–7·41) 6·81% (6·47–7·16) 6·91% (6·38–7·47) 9·79% (8·65–11·06) 9·24% (7·70–11·07) Psychotic disorder (any) 1·40% (1·30–1·51) 0·93% (0·83–1·04) 2·89% (2·62–3·18) 2·77% (2·31–3·33) 7·00% (6·01–8·14) Psychotic disorder (first) 0·42% (0·36–0·49) 0·25% (0·19–0·33) 0·89% (0·72–1·09) 0·70% (0·46–1·06) 2·12% (1·53–2·94) Substance use disorder (any) 6·58% (6·36–6·80) 5·87% (5·63–6·13) 8·56% (8·10–9·04) 10·14% (9·25–11·10) 11·85% (10·55–13·31) Substance use disorder (first) 1·92% (1·77–2·07) 1·74% (1·58–1·91) 2·09% (1·82–2·40) 3·15% (2·60–3·82) 2·58% (1·91–3·47) Insomnia (any) 5·42% (5·20–5·64) 5·16% (4·91–5·42) 5·95% (5·53–6·39) 7·50% (6·66–8·44) 9·82% (8·57–11·24) Insomnia (first) 2·53% (2·37–2·71) 2·23% (2·05–2·43) 3·14% (2·81–3·51) 4·24% (3·55–5·07) 5·05% (4·10–6·20) Any outcome 33·62% (33·17–34·07) 31·74% (31·22–32·27) 38·73% (37·87–39·60) 46·42% (44·78–48·09) 62·34% (60·14–64·55) Any first outcome 12·84% (12·36–13·33) 11·51% (10·98–12·07) 15·29% (14·32–16·33) 25·79% (23·50–28·25) 31·13% (27·29–35·36) Data are percentage at 6 months (95% CI). Additional outcomes are presented in the appendix (pp 27–28). ITU=intensive therapy unit. Table 2: Major outcomes for the whole COVID-19 cohort, and for the non-hospitalization, hospitalization, ITU admission, and encephalopathy cohorts during the illness Articles 420 www.thelancet.com/psychiatry Vol 8 May 2021 the time of the analysis, another restricting the COVID-19 diagnoses to patients who had a positive RNA or antigen test (and using antigen test as an index event), and another comparing the rates of sequelae of patients with COVID-19 with those observed in patients with influenza before the pandemic (ie, in 2019 or 2018). Details of these analyses are provided in the appendix (p 6). Finally, to test whether differences in sequelae between cohorts could be accounted for by differences in extent of follow-up, we counted the average number of health visits that each cohort had during the follow-up period. Statistical analysis We used propensity score matching19 to create cohorts with matched baseline characteristics, done within the TriNetX network. Propensity score with 1:1 matching used a greedy nearest neighbor matching approach with a caliper distance of 0·1 pooled SDs of the logit of the propensity score. Any characteristic with a standardized mean difference between cohorts lower than 0·1 was considered well matched.20 The incidence of each outcome was estimated by use of the KaplanMeier estimator. Comparisons between cohorts were made with a log-rank test. We calculated HRs with 95% CIs using a proportional hazard model wherein the cohort to which the patient belonged was used as the independent variable. The proportional hazard assumption was tested with the generalized Schoenfeld approach. When the assumption was violated, the time varying HR was assessed with natural cubic splines fitted to the log cumulative hazard.21 Additional details are presented in the appendix (p 6). Statistical analyses were done in R, version 3.4.3, except for the log-rank tests, which were done within TriNetX. Statistical significance was set at two-sided p-value <0⋅05. Our study was reported according to the Reporting of studies Conducted using Observational Routinely collected health Data (RECORD, appendix pp 55–60). Role of the funding source The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. Results Our primary cohort comprised 236 379 patients diagnosed with COVID-19, and our two propensity-score matched control cohorts comprised 105579 patients diagnosed with influenza and 236 038 patients diagnosed with any respiratory tract infection including influenza. The COVID-19 cohort was divided into subgroups of patients who were not hospitalized (190077 patients), those who were hospitalized (46 302 patients), those who required ITU admission (8945 patients), and those who received a diagnosis of encephalopathy (6229 patients). The main demographic features and comorbidities of the COVID-19 cohort are summarized in table 1, with additional demographic details presented in the appendix (pp 25–27). Matched baseline characteristics of the two control cohorts are also presented in the appendix (pp 29–30 for patients with influenza, and pp 31–32 for patients with other respiratory tract infections). Adequate propensity-score matching (standardized mean difference <0·1) was achieved for all comparisons and baseline characteristics. We estimated the diagnostic incidence of the neurological and psychiatric outcomes of the primary cohort in the 6 months after a COVID-19 diagnosis. In the whole cohort, 33·62% (95% CI 33·17–34·07) of patients received a diagnosis (table 2). For the cohort subgroups, these estimates were 38·73% (37·87–39·60) for patients who were hospitalized, 46·42% (44·78–48·09) for those admitted to ITU, and 62·34% (60·14–64·55) for those diagnosed with COVID-19 vs influenza (N=105 579)* COVID-19 vs other RTI (N=236038)* HR (95% CI) p value HR (95% CI) p value Intracranial hemorrhage (any) 2·44 (1·89–3·16) <0·0001 1·26 (1·11–1·43) 0·0003 Intracranial hemorrhage (first) 2·53 (1·68–3·79) <0·0001 1·56 (1·27–1·92) <0·0001 Ischemic stroke (any) 1·62 (1·43–1·83) <0·0001 1·45 (1·36–1·55) <0·0001 Ischemic stroke (first) 1·97 (1·57–2·47) <0·0001 1·63 (1·44–1·85) <0·0001 Parkinsonism 1·42 (0·75–2·67) 0·19 1·45 (1·05–2·00) 0·020 Guillain-Barré syndrome 1·21 (0·72–2·04) 0·41 2·06 (1·43–2·96) <0·0001 Nerve, nerve root, or plexus disorders 1·64 (1·50–1·81) <0·0001 1·27 (1·19–1·35) <0·0001 Myoneural junction or muscle disease 5·28 (3·71–7·53) <0·0001 4·52 (3·65–5·59) <0·0001 Encephalitis 1·70 (1·04–2·78) 0·028 1·41 (1·03–1·92) 0·028 Dementia 2·33 (1·77–3·07) <0·0001 1·71 (1·50–1·95) <0·0001 Mood, anxiety, or psychotic disorder (any) 1·46 (1·43–1·50) <0·0001 1·20 (1·18–1·23) <0·0001 Mood, anxiety, or psychotic disorder (first) 1·81 (1·69–1·94) <0·0001 1·48 (1·42–1·55) <0·0001 Mood disorder (any) 1·47 (1·42–1·53) <0·0001 1·23 (1·20–1·26) <0·0001 Mood disorder (first) 1·79 (1·64–1·95) <0·0001 1·41 (1·33–1·50) <0·0001 Anxiety disorder (any) 1·45 (1·40–1·49) <0·0001 1·17 (1·15–1·20) <0·0001 Anxiety disorder (first) 1·78 (1·66–1·91) <0·0001 1·48 (1·42–1·55) <0·0001 Psychotic disorder (any) 2·03 (1·78–2·31) <0·0001 1·66 (1·53–1·81) <0·0001 Psychotic disorder (first) 2·16 (1·62–2·88) <0·0001 1·82 (1·53–2·16) <0·0001 Substance use disorder (any) 1·27 (1·22–1·33) <0·0001 1·09 (1·05–1·12) <0·0001 Substance use disorder (first) 1·22 (1·09–1·37) 0·0006 0·92 (0·86–0·99) 0·033 Insomnia (any) 1·48 (1·38–1·57) <0·0001 1·15 (1·10–1·20) <0·0001 Insomnia (first) 1·92 (1·72–2·15) <0·0001 1·43 (1·34–1·54) <0·0001 Any outcome 1·44 (1·40–1·47) <0·0001 1·16 (1·14–1·17) <0·0001 Any first outcome 1·78 (1·68–1·89) <0·0001 1·32 (1·27–1·36) <0·0001 Additional details on cohort characteristics and diagnostic subcategories are presented in the appendix (pp 29–33). HR=hazard ratio. RTI=respiratory tract infection. *Matched cohorts. Table 3: HRs for the major outcomes in patients after COVID-19 compared with those after influenza and other RTIs Articles www.thelancet.com/psychiatry Vol 8 May 2021 421 encephalopathy. A similar, but more marked, increasing trend was observed for patients receiving their first recorded neurological or psychiatric diagnosis (table 2). Results according to sex, race, and age are shown in the appendix (p 28). The baseline characteristics of the COVID-19 cohort divided into those who did versus those who did not have a neurological or psychiatric outcome are also shown in the appendix (p 7). We assessed the probability of the major neurological and psychiatric outcomes in patients diagnosed with COVID-19 compared with the matched cohorts diagnosed with other respiratory tract infections and with influenza (table 3; figure 1, appendix pp 8–10). Most diagnostic categories were more common in patients who had COVID-19 than in those who had influenza (HR 1·44, 95% CI 1·40–1·47 for any diagnosis; 1·78, 1·68–1·89 for any first diagnosis) and those who had other respiratory tract infections (1·16, 1·14–1·17 for any diagnosis; 1·32, 1·27–1·36 for any first diagnosis). Hazard rates were also higher in patients who were admitted to ITU than in those who were not (1·58, 1·50–1·67 for any diagnosis; 2·87, 2·45–3·35 for any first diagnosis). HRs were significantly greater than 1 for all diagnoses for patients who had COVID-19 compared with those who had influenza, except for parkinsonism and Guillain-Barré syndrome, and significantly greater than 1 for all diagnoses compared with patients who had respiratory tract infections (table 3). Similar results were observed when patients who had COVID-19 were compared with those who had Figure 1: Kaplan-Meier estimates for the incidence of major outcomes after COVID-19 compared with other RTIs Shaded areas are 95% CIs. For incidences of first diagnoses, the number in brackets corresponds to all patients who did not have the outcome before the follow-up period. For diagnostic subcategories, see appendix (pp 8–10). RTI=respiratory tract infection. Number at risk COVID-19 Other RTI 0 50 100 150 200 92579 131885 67102 116315 Intracranial haemorrhage (any) 50172 103261 32705 90066 20679 77005 12775 65909 0 0·2 0·6 0·4 0·8 Outcome probability (%) 30 60 90 120 150 180 0 50 100 150 200 91998 131352 66499 115264 48528 102599 32265 89412 20361 76367 11415 63334 0 0·5 2·0 1·5 2·5 30 60 90 120 150 180 0 50 100 150 200 92193 131363 66587 115073 48488 102233 32186 88929 19962 75806 11585 62702 0 1·0 3·0 2·0 4·0 30 60 90 120 150 180 COVID-19 (n=236038) Other RTI (n=236038) COVID-19 (n=236038) Other RTI (n=236038) COVID-19 (n=236038) Other RTI (n=236038) Ischaemic stroke (any) Nerve, nerve root, or plexus disorder Number at risk COVID-19 Other RTI 0 50 100 Time since index event (days) Time since index event (days) Time since index event (days) 150 200 91646 133203 66346 115207 Myoneural junction or muscle disease 50653 102653 34259 90454 21522 76919 11895 63909 0 0·2 0·1 0·5 0·4 0·3 0·6 Outcome probability (%) 30 60 90 120 150 180 0 50 100 150 200 89958 128680 65186 113623 47578 101313 32182 88082 19593 75359 12242 62553 0 0·2 0·6 0·4 0·8 30 60 90 120 150 180 0 50 100 150 200 84435 122790 58504 103824 41026 89662 26310 75998 15885 63173 8741 51033 0 10 5 20 15 25 30 60 90 120 150 180 Dementia Mood, anxiety, or psychotic disorder COVID-19 (n=234527) Other RTI (n=234810) COVID-19 (n=230151) Other RTI (n=230495) COVID-19 (n=236038) Other RTI (n=236038) Articles 422 www.thelancet.com/psychiatry Vol 8 May 2021 one of the four other index events (appendix pp 11–14, 34), except when an outcome had a predicted relationship with the comparator condition (eg, intracranial hemorrhage was more common in association with fracture of a large bone). HRs for diagnostic subcategories are presented in the appendix (p 33). There were no violations of the proportional hazards assumption for most of the neurological outcomes over the 6 months of follow-up (appendix pp 15, 35). The only exception was for intracranial hemorrhage and ischemic stroke in patients who had COVID-19 when compared with patients who had other respiratory tract infections (p=0·012 for intracranial hemorrhage and p=0·032 for ischemic stroke). For the overall psychiatric disorder category (ICD-10 F20–48), the HR did vary with time, declining but remaining significantly higher than 1, indicating that the risk was attenuated but maintained 6 months after COVID-19 diagnosis (appendix p 9). HRs for COVID-19 diagnosis compared with the additional four index events showed more variation with time, partly reflecting the natural history of the comparator condition (appendix, pp 16–19, 36). We explored the effect of COVID-19 severity in four ways. First, we restricted analyses to matched cohorts of patients who had not required hospitalization (matched baseline characteristics in the appendix, pp 37–40). HRs remained significantly greater than 1 in this subgroup, with an overall HR for any diagnosis of 1·47 (95% CI 1·44–1·51) for patients who had COVID-19 compared with patients who had influenza, and 1·16 (1·14–1·17) compared with those who had other respiratory tract infections (table 4, appendix pp 20–21). For a first diagnosis, the HRs were 1·83 (1·71–1·96) versus patients who had influenza and 1·28 (1·23–1·33) versus those who had other respiratory tract infections. Second, we calculated HRs for the matched cohorts of patients with COVID-19 requiring hospitalization versus those who did not require hospitalization (44 927 matched patients; matched baseline characteristics are presented in the appendix, pp 41–42). This comparison showed greater hazard rates for all outcomes in the hospitalized group than in the non-hospitalized group, except for nerve, nerve root, or plexus disorders (table 5, figure 2), with an overall HR of 1·33 (1·29–1·37) for any diagnosis and 1·70 (1·56–1·86) for any first diagnosis. Third, we calculated HRs for the matched cohorts of patients with COVID-19 requiring ITU admission versus those not COVID-19 vs influenza in patients without hospitalization (N=96803)* COVID-19 vs other RTI in patients without hospitalization (N=183 731)* HR (95% CI) p value HR (95% CI) p value Intracranial hemorrhage (any) 1·87 (1·25–2·78) 0·0013 1·38 (1·11–1·73) 0·0034 Intracranial hemorrhage (first) 1·66 (0·88–3·14) 0·082 1·63 (1·11–2·40) 0·010 Ischemic stroke (any) 1·80 (1·54–2·10) <0·0001 1·61 (1·45–1·78) <0·0001 Ischemic stroke (first) 1·71 (1·26–2·33) 0·0003 1·69 (1·38–2·08) <0·0001 Parkinsonism 2·22 (0·98–5·06) 0·028 1·20 (0·73–1·96) 0·42 Guillain-Barré syndrome 0·90 (0·44–1·84) 0·99 1·44 (0·85–2·45) 0·10 Nerve, nerve root, or plexus disorders 1·69 (1·53–1·88) <0·0001 1·23 (1·15–1·33) <0·0001 Myoneural junction or muscle disease 3·46 (2·11–5·67) <0·0001 2·69 (1·91–3·79) <0·0001 Encephalitis 1·77 (0·86–3·66) 0·095 2·29 (1·28–4·10) 0·0046 Dementia 1·88 (1·27–2·77) 0·0008 1·95 (1·55–2·45) <0·0001 Mood, anxiety, or psychotic disorder (any) 1·49 (1·45–1·54) <0·0001 1·18 (1·15–1·21) <0·0001 Mood, anxiety, or psychotic disorder (first) 1·85 (1·72–1·99) <0·0001 1·40 (1·32–1·48) <0·0001 Mood disorder (any) 1·49 (1·43–1·55) <0·0001 1·22 (1·19–1·26) <0·0001 Mood disorder (first) 1·78 (1·61–1·96) <0·0001 1·37 (1·27–1·47) <0·0001 Anxiety disorder (any) 1·48 (1·43–1·54) <0·0001 1·16 (1·13–1·19) <0·0001 Anxiety disorder (first) 1·80 (1·67–1·94) <0·0001 1·37 (1·30–1·45) <0·0001 Psychotic disorder (any) 1·93 (1·63–2·28) <0·0001 1·44 (1·27–1·62) <0·0001 Psychotic disorder (first) 2·27 (1·56–3·30) <0·0001 1·49 (1·15–1·93) 0·0016 Substance use disorder (any) 1·26 (1·19–1·33) <0·0001 1·11 (1·07–1·17) <0·0001 Substance use disorder (first) 1·21 (1·05–1·38) 0·0054 0·89 (0·81–0·97) 0·013 Insomnia (any) 1·52 (1·42–1·63) <0·0001 1·18 (1·12–1·24) <0·0001 Insomnia (first) 2·06 (1·82–2·33) <0·0001 1·51 (1·38–1·66) <0·0001 Any outcome 1·47 (1·44–1·51) <0·0001 1·16 (1·14–1·17) <0·0001 Any first outcome 1·83 (1·71–1·96) <0·0001 1·28 (1·23–1·33) <0·0001 Details on cohort characteristics are presented in the appendix (pp 37–40). HR=hazard ratio. RTI=respiratory tract infection. *Matched cohorts. Table 4: HRs for the major outcomes in patients without hospitalization after COVID-19 compared with those after influenza or other RTIs Articles www.thelancet.com/psychiatry Vol 8 May 2021 423 requiring ITU admission (8942 patients; matched baseline characteristics presented in the appendix, pp 43–44), with a HR of 1·58 (1·50–1·67) for any diagnosis and 2·87 (2·45–3·35) for any first diagnosis (table 5, appendix p 22). Fourth, we calculated HRs for the matched cohorts of patients with COVID-19 who had encephalopathy diagnosed during acute illness versus those who did not (6221 patients; matched baseline characteristics presented in the appendix, pp 45–46). HRs for all diagnoses were greater for the group who had encephalopathy than for the matched cohort who did not, with an overall HR of 1·85 (1·73–1·98) for any diagnosis and 3·19 (2·54–4·00) for any first diagnosis (table 5, figure 2). We inspected other factors that might influence the findings. The results regarding hospitalization, ITU admission, or encephalopathy (which we had defined as occurring up to 14 days after diagnosis) could be confounded by admissions due to an early complication of COVID-19 rather than to COVID-19 itself. This was explored by excluding outcomes during this period, with the findings remaining similar, albeit with many HRs being reduced (appendix pp 47–49). Additionally, COVID-19 survivors had fewer health-care visits during the 6-month period compared with the other cohorts (appendix p 50). Hence the higher incidence of many diagnoses was not simply due to having had more diagnostic opportunities. The increased rates of neurological and psychiatric sequelae were robust in all three sensitivity analyses: when patients who had died by the time of the analysis were included (appendix p 51), when the COVID-19 diagnosis was confirmed by use of an RNA or antigen test (appendix p 52), and when the sequelae were compared with those observed in patients who had influenza in 2019 or 2018 (appendix pp 53). Discussion Various adverse neurological and psychiatric outcomes occurring after COVID-19 have been predicted and COVID-19 with vs without hospitalization (N=45167) COVID-19 with vs without ITU admission (N=8942) COVID-19 with vs without encephalopathy (N=6221) HR (95% CI) p value HR (95% CI) p value HR (95% CI) p value Intracranial hemorrhage (any) 3·09 (2·43–3·94) <0·0001 5·06 (3·43–7·47) <0·0001 4·73 (3·15–7·11) <0·0001 Intracranial hemorrhage (first) 3·75 (2·49–5·64) <0·0001 5·12 (2·68–9·77) <0·0001 5·00 (2·33–10·70) <0·0001 Ischemic stroke (any) 1·65 (1·48–1·85) <0·0001 1·93 (1·62–2·31) <0·0001 1·65 (1·38–1·97) <0·0001 Ischemic stroke (first) 2·82 (2·22–3·57) <0·0001 3·51 (2·39–5·15) <0·0001 3·39 (2·17–5·29) <0·0001 Parkinsonism 2·63 (1·45–4·77) 0·0016 3·90 (1·29–11·79) 0·024 1·64 (0·75–3·58) 0·24 Guillain-Barré syndrome 2·94 (1·60–5·42) 0·00094 11·01 (2·55–47·61) 0·0007 2·27 (0·76–6·73) 0·24 Nerve, nerve root, or plexus disorders 0·94 (0·83–1·06) 0·29 1·16 (0·92–1·45) 0·21 1·41 (1·07–1·87) 0·018 Myoneural junction or muscle disease 7·76 (5·15–11·69) <0·0001 11·53 (6·38–20·83) <0·0001 5·40 (3·21–9·07) <0·0001 Encephalitis 3·26 (1·75–6·06) 0·0002 1·78 (0·75–4·20) 0·22 9·98 (2·98–33·43) <0·0001 Dementia 2·28 (1·80–2·88) <0·0001 1·66 (1·12–2·46) 0·018 4·25 (2·79–6·47) <0·0001 Mood, anxiety, or psychotic disorder (any) 1·23 (1·18–1·28) <0·0001 1·34 (1·24–1·46) <0·0001 1·73 (1·58–1·90) <0·0001 Mood, anxiety, or psychotic disorder (first) 1·55 (1·40–1·71) <0·0001 2·27 (1·87–2·74) <0·0001 2·28 (1·80–2·89) <0·0001 Mood disorder (any) 1·21 (1·15–1·28) <0·0001 1·15 (1·03–1·27) 0·010 1·51 (1·35–1·70) <0·0001 Mood disorder (first) 1·53 (1·33–1·75) <0·0001 2·06 (1·57–2·71) <0·0001 2·09 (1·55–2·80) <0·0001 Anxiety disorder (any) 1·16 (1·10–1·22) <0·0001 1·39 (1·26–1·53) <0·0001 1·64 (1·45–1·84) <0·0001 Anxiety disorder (first) 1·49 (1·34–1·65) <0·0001 2·22 (1·82–2·71) <0·0001 1·91 (1·48–2·45) <0·0001 Psychotic disorder (any) 2·22 (1·92–2·57) <0·0001 1·48 (1·14–1·92) 0·0028 3·84 (2·90–5·10) <0·0001 Psychotic disorder (first) 2·77 (1·99–3·85) <0·0001 1·77 (0·98–3·20) 0·072 5·62 (2·93–10·77) <0·0001 Substance use disorder (any) 1·53 (1·42–1·64) <0·0001 1·62 (1·41–1·85) <0·0001 1·45 (1·24–1·70) <0·0001 Substance use disorder (first) 1·68 (1·40–2·01) <0·0001 2·53 (1·83–3·50) <0·0001 2·03 (1·32–3·11) 0·0015 Insomnia (any) 1·08 (0·99–1·18) 0·088 1·40 (1·19–1·66) <0·0001 1·73 (1·42–2·11) <0·0001 Insomnia (first) 1·49 (1·28–1·74) <0·0001 1·93 (1·46–2·55) <0·0001 3·44 (2·35–5·04) <0·0001 Any outcome 1·33 (1·29–1·37) <0·0001 1·58 (1·50–1·67) <0·0001 1·85 (1·73–1·98) <0·0001 Any first outcome 1·70 (1·56–1·86) <0·0001 2·87 (2·45–3·35) <0·0001 3·19 (2·54–4·00) <0·0001 Details on cohort characteristics are presented in the appendix (pp 41–46). HR=hazard ratio. ITU=intensive therapy unit. *Matched cohorts. Table 5: HRs for the major outcomes after COVID-19 for patients with vs those without hospitalization, patients with vs without ITU admission, and patients with vs without encephalopathy Articles 424 www.thelancet.com/psychiatry Vol 8 May 2021 Encephalopathy Matched cohort without encephalopathy Number at risk Encephalopathy Matched cohort without encephalopathy Hospitalization Matched cohort without hospitalization 0 50 100 150 200 Intracranial hemorrhage (any) 0 1 4 3 2 Outcome probability (%) 30 60 90 120 150 180 Ischemic stroke (any) Total 6221 6221 45167 45167 3214 3424 20486 20010 2296 2372 14717 14696 1746 2372 11818 11185 1269 1244 7766 7344 1032 1244 5232 4799 733 642 4030 3598 0 50 100 150 200 0 2·5 10·0 7·5 5·0 Total 30 60 90 120 150 180 6221 6221 45167 45167 3133 2989 20218 19587 2201 2187 14429 14515 1639 1641 10786 10792 1177 1221 7566 7464 821 758 5083 4714 634 758 3551 3133 Number at risk Encephalopathy Matched cohort without encephalopathy Hospitalization Matched cohort without hospitalization 0 50 100 150 200 Nerve, nerve root, or plexus disorder 0 1 5 4 3 2 Outcome probability (%) 30 60 90 120 150 180 Myoneural junction or muscle disease Total 0 50 100 150 200 0 1 4 3 2 Total 30 60 90 120 150 180 6221 6221 45167 45167 3277 3125 20453 19636 2317 2225 14614 14537 1701 1701 10902 10775 1231 1314 7737 7447 881 825 5062 4549 602 596 3378 2606 5906 6109 44481 44788 2996 3067 20044 20069 2127 2236 14345 16550 1836 1916 10853 13067 1292 1916 8206 10185 790 1139 5270 10185 604 635 3320 4092 Number at risk Encephalopathy Matched cohort without encephalopathy Hospitalization Matched cohort without hospitalization 0 50 100 Time since index event (days) Time since index event (days) 150 200 Dementia 0 1 5 4 3 2 Outcome probability (%) 30 60 90 120 150 180 Mood, anxiety, or psychotic disorder Total 0 50 100 150 200 0 10 40 30 20 Total 30 60 90 120 150 180 4704 5094 42434 42877 2627 2562 19428 18719 1929 2010 13970 13904 1425 1419 10567 10329 1036 986 7611 7017 717 986 5427 5174 583 986 3616 2697 6221 6221 45167 45167 2640 2729 18072 18092 1734 1910 12352 12874 1217 1417 8933 9170 888 955 6068 5925 575 633 3976 3653 351 437 2501 2001 Hospitalization Matched cohort without hospitalization Articles www.thelancet.com/psychiatry Vol 8 May 2021 425 reported.1–5,14 The data presented in this study, from a large electronic health records network, support these predictions and provide estimates of the incidence and risk of these outcomes in patients who had COVID-19 compared with matched cohorts of patients with other health conditions occurring contemporaneously with the COVID-19 pandemic (tables 2, 3, figure 1). The severity of COVID-19 had a clear effect on subsequent neurological diagnoses (tables 4, 5, figure 2). Overall, COVID-19 was associated with increased risk of neurological and psychiatric outcomes, but the incidences and HRs of these were greater in patients who had required hospitalization, and markedly so in those who had required ITU admission or had developed encephalopathy, even after extensive propensity score matching for other factors (eg, age or previous cerebrovascular disease). Potential mechanisms for this association include viral invasion of the CNS,10,11 hypercoagulable states,22 and neural effects of the immune response.9 However, the incidence and relative risk of neurological and psychiatric diagnoses were also increased even in patients with COVID-19 who did not require hospitalization. Some specific neurological diagnoses merit individual mention. Consistent with several other reports,23,24 the risk of cerebrovascular events (ischemic stroke and intracranial hemorrhage) was elevated after COVID-19, with the incidence of ischemic stroke rising to almost one in ten (or three in 100 for a first stroke) in patients with encephalopathy. A similarly increased risk of stroke in patients who had COVID-19 compared with those who had influenza has been reported.25 Our previous study reported preliminary evidence for an association between COVID-19 and dementia.14 The data in this study support this association. Although the estimated incidence was modest in the whole COVID-19 cohort (table 2), 2·66% of patients older than 65 years (appendix p 28) and 4·72% who had encephalopathy (table 2), received a first diagnosis of dementia within 6 months of having COVID-19. The associations between COVID-19 and cerebrovascular and neurodegenerative diagnoses are concerning, and information about the severity and subsequent course of these diseases is required. Whether COVID-19 is associated with Guillain-Barré syndrome remains unclear;26 our data were also equivocal, with HRs increased with COVID-19 compared with other respiratory tract infections but not with influenza (table 3), and increased compared with three of the four other index health events (appendix p 34). Concerns have also been raised about post-COVID-19 parkinsonian syndromes, driven by the encephalitis lethargica epidemic that followed the 1918 influenza pandemic.27 Our data provide some support for this possibility, although the incidence was low and not all HRs were significant. Parkinsonism might be a delayed outcome, in which case a clearer signal might emerge with a longer follow-up. The findings regarding anxiety and mood disorders were broadly consistent with 3-month outcome data from a study done in a smaller number of cases than our cohort, using the same network,14 and showed that the HR remained elevated, although decreasing, at the 6-month period. Unlike the earlier study, and in line with previous suggestions,28 we also observed a significantly increased risk of psychotic disorders, probably reflecting the larger sample size and longer duration of follow-up reported here. Substance use disorders and insomnia were also more common in COVID-19 survivors than in those who had influenza or other respiratory tract infections (except for the incidence of a first diagnosis of substance use disorder after COVID-19 compared with other respiratory tract infections). Therefore, as with the neurological outcomes, the psychiatric sequelae of COVID-19 appear widespread and to persist up to, and probably beyond, 6 months. Compared with neurological disorders, common psychiatric disorders (mood and anxiety disorders) showed a weaker relationship with the markers of COVID-19 severity in terms of incidence (table 2) or HRs (table 5). This might indicate that their occurrence reflects, at least partly, the psychological and other implications of a COVID-19 diagnosis rather than being a direct manifestation of the illness. HRs for most neurological outcomes were constant, and hence the risks associated with COVID-19 persisted up to the 6-month timepoint. Longer-term studies are needed to ascertain the duration of risk and the trajectory for individual diagnoses. Our findings are robust given the sample size, the propensity score matching, and the results of the sensitivity and secondary analyses. Nevertheless, they have weaknesses inherent to an electronic health records study,29 such as the unknown completeness of records, no validation of diagnoses, and sparse information on socioeconomic and lifestyle factors. These issues primarily affect the incidence estimates, but the choice of cohorts against which to compare COVID-19 outcomes influenced the magnitude of the HRs (table 3, appendix p 34). The analyses regarding encephalopathy (delirium and related conditions) deserve a note of caution. Even among patients who were hospitalized, only about 11% received this Figure 2: Kaplan-Meier estimates for the incidence of major outcomes after COVID-19 comparing patients requiring hospitalization with matched patients not requiring hospitalization, and comparing those who had encephalopathy with matched patients who did not have encephalopathy 95% CIs are omitted for clarity but are shown in the appendix (p 23). For incidences of first diagnoses, the total number corresponds to all patients who did not have the outcome before the follow-up period. The equivalent figure showing the comparison between patients with intensive therapy unit admission versus those without is presented in the appendix (p 22). Articles 426 www.thelancet.com/psychiatry Vol 8 May 2021 diagnosis, whereas much higher rates would be expected.18,30 Under-recording of delirium during acute illness is well known and probably means that the diagnosed cases had prominent or sustained features; as such, results for this group should not be generalized to all patients with COVID-19 who experience delirium. We also note that encephalopathy is not just a severity marker but a diagnosis in itself, which might predispose to, or be an early sign of, other neuropsychiatric or neurodegenerative outcomes observed during follow-up. The timing of index events was such that most infections with influenza and many of the other respiratory tract infections occurred earlier on during the pandemic, whereas the incidence of COVID-19 diagnoses increased over time (appendix p 24). The effect of these timing differences on observed rates of sequelae is unclear but, if anything, they are likely to make the HRs an underestimate because COVID-19 cases were diagnosed at a time when all other diagnoses were made at a lower rate in the population (appendix p 24). Some patients in the comparison cohorts are likely to have had undiagnosed COVID-19; this would also tend to make our HRs an underestimate. Finally, a study of this kind can only show associations; efforts to identify mechanisms and assess causality will require prospective cohort studies and additional study designs. In summary, the present data show that COVID-19 is followed by significant rates of neurological and psychiatric diagnoses over the subsequent 6 months. Services need to be configured, and resourced, to deal with this anticipated need. Contributors PJH and MT were granted unrestricted access to the TriNetX Analytics network for the purposes of research, and with no constraints on the analyses done or the decision to publish; they designed the study and directly accessed the TriNetX Analytics web interface to do it. MT, JRG, MH, and PJH defined cohort inclusion and exclusion criteria, and the outcome criteria and analytical approaches. MT did the data analyses, assisted by SL and PJH. All authors contributed to data interpretation. MT and PJH wrote the paper with input from JRG, MH, and SL. MT and PJH verified the data. PJH is the guarantor. PJH and MT had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. Declaration of interests SL is an employee of TriNetX. All other authors declare no competing interests. Data sharing The TriNetX system returned the results of these analyses as .csv files, which were downloaded and archived. Data presented in this paper can be freely accessed online. Additionally, TriNetX will grant access to researchers if they have a specific concern (through a third-party agreement option).
Acknowledgments
This work was supported by the NIHR Oxford Health Biomedical Research Centre (grant BRC-1215–20005). MT is an NIHR Academic Clinical Fellow. MH is supported by a Wellcome Trust Principal Research Fellowship and the NIHR Oxford Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the UK National Health Service, NIHR, or the UK Department of Health.
References
1 Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020; 7: 611–27.
2 Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol 2020; 19: 767–83.
3 Varatharaj A, Thomas N, Ellul MA, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 2020; 7: 875–82.
4 Paterson RW, Brown RL, Benjamin L, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain 2020; 143: 3104–20.
5 Kremer S, Lersy F, Anheim M, et al. Neurologic and neuroimaging findings in patients with COVID-19: a retrospective multicenter study. Neurology 2020; 95: e1868–82.
6 Pezzini A, Padovani A. Lifting the mask on neurological manifestations of COVID-19. Nat Rev Neurol 2020; 16: 636–44.
7 Raman B, Cassar MP, Tunnicliffe EM, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine 2021; 31: 100683.
8 Iadecola C, Anrather J, Kamel H. Effects of COVID-19 on the nervous system. Cell 2020; 183: 16–27.
9 Kreye J, Reincke SM, Prüss H. Do cross-reactive antibodies cause neuropathology in COVID-19? Nat Rev Immunol 2020; 20: 645–46.
10 Meinhardt J, Radke J, Dittmayer C, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci 2021; 24: 168–75.
11 Rhea EM, Logsdon AF, Hansen KM, et al. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat Neurosci 2021; 24: 368–78.
12 Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020; 7: 547–60.
13 Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020; 89: 531–42.
14 Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021; 8: 130–40.
15 de Lusignan S, Dorward J, Correa A, et al. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis 2020; 20: 1034–42.
16 Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–36.
17 Slooter AJC, Otte WM, Devlin JW, et al. Updated nomenclature of delirium and acute encephalopathy: statement of ten Societies. Intensive Care Med 2020; 46: 1020–22.
18 Oldham MA, Slooter AJC, Cunningham C, et al. Characterising neuropsychiatric disorders in patients with COVID-19. Lancet Psychiatry 2020; 7: 932–33.
19 Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011; 46: 399–424.
20 Haukoos JS, Lewis RJ. The propensity score. JAMA 2015; 314: 1637–38. 21 Royston P, Parmar MKB. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med 2002;
21: 2175–97.
22 Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost 2020; 18: 1738–42.
23 Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A, Young B. Stroke as a neurological complication of COVID-19: a systematic review and meta-analysis of incidence, outcomes and predictors. J Stroke Cerebrovasc Dis 2021; 30: 105549. For the study data see https:// osf.io/7tzvy Articles www.thelancet.com/psychiatry Vol 8 May 2021 427
24 Hernandez-Fernandez F, Valencia HS, Barbella-Aponte R, et al. Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain 2020; 143: 3089–103.
25 Xie Y, Bowe B, Maddukuri G, Al-Aly Z. Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with COVID-19 and seasonal influenza: cohort study. BMJ 2020; 371: m4677.
26 Keddie S, Pakpoor J, Mousele C, et al. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain 2020; published online Dec 14. https://doi. org/10.1093/brain/awaa433.
27 Hoffman LA, Vilensky JA. Encephalitis lethargica: 100 years after the epidemic. Brain 2017; 140: 2246–51.
28 Watson CJ, Thomas RH, Solomon T, Michael BD, Nicholson TR, Pollak TA. COVID-19 and psychosis risk: real or delusional concern? Neurosci Lett 2021; 741: 135491.
29 Casey JA, Schwartz BS, Stewart WF, Adler NE. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health 2016; 37: 61–81.
30 Docherty AB, Harrison EM, Green CA, et al. Features of 20133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 2020; 369: m1985.