Authors: the UC Davis Post-COVID-19 clinic CORONAVIRUS February 11, 2022
Known to health experts as post-acute sequelae SARS-CoV-2 infection (PASC), it is more commonly known as long-haul COVID or long COVID. The Centers for Disease Control describes post-COVID conditions as ongoing or new symptoms occurring a month or more after a COVID-19 infection. It is estimated that between 10% to 30% of people who had COVID-19 may experience long COVID.
1. Fatigue is the number one symptom seen at the clinic
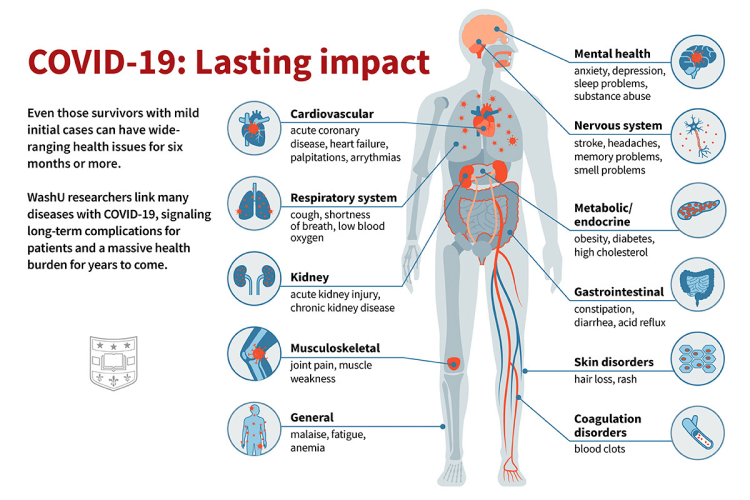
“Fatigue, depression, loss of sense of smell, brain fog and chest pain are the five most common symptoms I see,” said Christian Sandrock, an infectious diseases expert and the director of critical care at UC Davis Medical Center. “Shortness of breath and anxiety round it out.” These correspond with symptoms identified by the CDC, which notes that people with long COVID can experience multi-organ symptoms weeks or sometimes months after infection. An international study released in 2021 identified more than 200 symptoms, including hallucinations, tremors and tinnitus, or ringing and buzzing in the ears. The widespread nature of the symptoms might be explained by an NIH study that found the virus can spread throughout the body, including the brain, and persist for months after the acute infection. “It’s a complex disease,” Sandrock said. “We are still figuring it out more than a year after opening the clinic.”
2. SSRIs may help some patients with long-haul COVID
In addition to treatments like inhaled steroids and bronchodilators for post-viral cough, antidepressants are a common therapy for some long COVID patients. Selective serotonin reuptake inhibitors, known as SSRIs, are the number one type of medication Sandrock uses in the long-haul clinic. These are medicines like Prozac. “The mechanism for why SSRIs are effective isn’t yet clear. We know that patients with COVID-19 experience neurologic symptoms. It may be related to inflammation. Or the infection could have created neurological dysregulation — ‘rewired’ the central nervous system in some way,” Sandrock said. “So, the SSRIs may help.”
3. The symptoms are generally not caused by widespread inflammation
When the clinic first opened, many of the physicians thought an inflammatory process likely drove the syndrome — the body’s immune system staying revved up, even though the illness was over. “Now, a year later, I can say that inflammation is rare,” said Mark Avdalovic, a specialist in pulmonary and critical care medicine and director of the clinic. “We look for evidence of ongoing whole-body inflammation by testing C-reactive protein, and we rarely find it. It’s a little bit opposite of what we thought we were going to see,” Avdalovic said.
4. There is no typical long COVID patient
The condition can affect anyone. Although there’s not a “typical” long COVID patient, there are some trends. They have not yet seen any children with severe long COVID symptoms. The largest group is between the ages of 27 and 54. “We are not seeing many older people,” Sandrock said. He noted that most of the patients are generally not obese or diabetic, which are risk factors during the acute phase of the disease. In the beginning, all the patients were unvaccinated because vaccines were not available. Now, they see some vaccinated patients, but not enough to be sure whether vaccines mostly prevent long-haul COVID.
5. Exercise can help some patients
Bradley Sanville is a pulmonary and critical care physician who specializes in exercise physiology and how disease affects exercise tolerance. He prescribes pulmonary or cardiac rehab for patients who don’t have exercise-induced fatigue. “Some are really reluctant in the beginning. They are afraid exercising might cause harm or make their symptoms worse. But most find it helpful. They feel better. And they are often surprised, when we push them, that they can tolerate more exercise than they thought,” Sanville said.
6. Women are slightly more likely to develop long-hauler symptoms
According to a study using data from the University of California COVID Research Data Set (CORDS), the breakdown of long-haul patients is generally about 53% female and 47% male. The UC Davis Health clinic, though, has seen almost twice as many women as men. This contrasts with the demographics of patients admitted for acute COVID infection, where men are the majority. Although it’s not clear why, more women seem to be affected by long COVID. “We know that there are conditions like autoimmune diseases that are more likely to be had by female patients,” Avdalovic said. “There may be a hormonal predisposition for certain symptoms, whether it’s an autoimmune process or something related to a chronic inflammatory state. I think this is an opportunity for research.”
7. Some long-haulers show improvements after getting the vaccine
Early data suggested that vaccines provided relief for many long-haulers, but 10 to 15% said they felt worse after getting them. At UC Davis Health, the results have been more positive. According to Sandrock, many patients said they felt better after getting the COVID-19 vaccine. “Not one I’ve seen said they felt worse after getting the COVID vaccine. There had been a concern that by getting the vaccine, their symptoms might get worse, but we haven’t seen it,” Sandrock said.
8. The reactivation of a previous virus may be causing long COVID symptoms
A study published in the journal Cell found reactivation of the Epstein-Barr Virus (EBV) to be a factor in developing long COVID. EBV is the virus that causes mononucleosis. The virus is also associated with chronic fatigue syndrome, which resembles long COVID symptoms for some people. According to Nam Tran, a professor of clinical pathology, the usual screening test for EBV, known as a heterophile antibody test, is not appropriate for evaluating EBV reactivation. But there are other serology tests — blood tests —that are. One EBV serology test looks at four different markers to determine if the infection is acute, recent, past or a reactivation. Another test looks at the EBV viral load and may be preferred over serology when evaluating reactivation cases. “The EBV serology or EBV viral load test can reveal if reactivation may be contributing to some symptoms experienced by long COVID patients,” Tran said.
9. There’s no test on the market that detects long COVID
There’s currently no single test that can determine if someone has long COVID. And unlike being able to find out if the Epstein-Barr virus has reactivated, there is presently no blood test on the market that can determine if the SARS-CoV-2 is still active in someone with long COVID, according to Tran. “Although some studies have detected tiny amounts of virus in blood, most tests are not able to detect such low amounts unless using very special highly sensitive techniques such as a mass spectrometer,” Tran said. Instead, physicians rely on a battery of tests such as the complete blood count (CBC), electrolytes, metabolites, hepatic function panels, cardiac biomarkers, thyroid panels and D-dimer to determine the overall health of the patient with long COVID.
10. Most patients get better, but it takes a while
Over the past year, Avdalovic has seen improvements with his patients in the long-haul clinic. “In general, these patients get better over time.” The first 15 patients seen at the clinic were all experiencing fatigue and shortness of breath. They saw their symptoms improve after seven weeks of pulmonary training or exercise to strengthen the lungs. Participants improved on the six-minute walk test, which measures how far someone can walk in six minutes and their cardiovascular response. “With about three-fourths of our patients, things eventually come back to either normal or near-normal for them. But it’s just that for some, it takes a long time,” Avdalovic said.