Authors: Goethe University Frankfurt am Main Nature Medicine September 3,2022
After recovering from a SARS-CoV-2 infection, many people complain of persistent heart complaints, such as poor exercise tolerance, palpitations or chest pain, even if the infection was mild and there were no known heart problems in the past. Earlier studies, predominantly among young, physically fit individuals, were already able to show that mild cardiac inflammation can occur after COVID-19. However, the underlying cause of persistent symptoms, and whether this changes over time, was unknown.
A team of medical scientists led by Dr. Valentina Puntmann and Professor Eike Nagel from the Institute for Experimental and Translational Cardiovascular Imaging at University Hospital Frankfurt followed up with 346 people—half of them women—between the age of 18 and 77 years, in each case around 4–11 months after the documented SARS-CoV-2 infection. For this purpose, the team analyzed the study participants’ blood, conducted heart MRIs, and recorded and graded their symptoms using standardized questionnaires.
At the beginning of the study, 73% reported heart problems; for 57% these symptoms persisted 11 months after the SARS-CoV-2 infection. The research team measured mild but persistent heart inflammation that was not accompanied by structural changes in the heart. Blood levels of troponin—a protein that enters the blood when the heart muscle is damaged—were also unremarkable.
Dr. Puntmann, who led the Impression COVID&Heart Study, explains, “The patients’ symptoms match our medical findings. It is important to note that although triggered by the SARS-CoV-2 virus, the post-COVID cardiac inflammatory involvement differs considerably from classic viral myocarditis. Extensive damage of the heart muscle leading to structural heart changes or impaired function are not characteristic at this stage of disease evolution.”
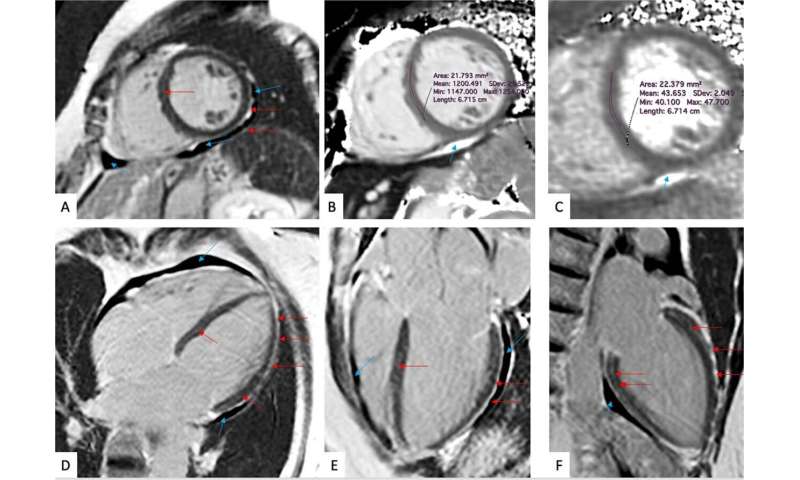
The clinical picture is more reminiscent, she says, of the findings in chronic diffuse inflammatory syndromes such as autoimmune conditions. “Although most likely driven by a virus-triggered autoimmune process, a lot more research is needed in order to understand the underlying pathophysiology. Similarly, the long-term effects of cardiac inflammation following a mild COVID infection need to be clarified in future studies.”
Because the study is restricted to a selected group of individuals who took part because they had symptoms, the prevalence of findings cannot be extrapolated to the population as a whole. The study appears in Nature Medicine.