John Murphy, M.D., M.P.H., DPH, President The Covid Long-haul Foundation
Abstract
Persistent transient loss of consciousness and pre-syncope (“blackout phenomena”) are increasingly recognized sequelae in patients with post-acute sequelae of SARS-CoV-2 infection (PASC or long COVID). These episodes are typically non-epileptic and arise from complex interactions between autonomic dysfunction, cardiovascular dysregulation, neuroinflammation, impaired cerebrovascular control, and contributing systemic factors. This review synthesizes current evidence on etiology, underlying physiological mechanisms, pathology, and precipitating clinical factors associated with blackout syndromes in long COVID, highlighting the need for systematic evaluation and multidisciplinary management.
1. Introduction
Long COVID is defined by persistent symptoms extending beyond three months after acute infection with SARS-CoV-2 without alternative explanation. Among diverse manifestations including fatigue, dyspnea, cognitive dysfunction, and exercise intolerance, many patients report orthostatic intolerance and transient loss of consciousness consistent with syncope or presyncope. These events represent significant morbidity and may substantially impair quality of life. Autonomic nervous system dysregulation is emerging as a key contributor to this clinical picture.
2. Etiology of Blackout Phenomena in Long-COVID
2.1 Autonomic Nervous System Dysfunction
A defining etiologic substrate in long COVID blackouts is cardiovascular autonomic dysfunction (CAD). In multiple cohorts, patients with PASC exhibit symptoms consistent with dysautonomia, including orthostatic intolerance and abnormalities on autonomic testing. In a prospective study, 79% of PASC patients met criteria for postural orthostatic tachycardia syndrome (POTS), and autonomic symptom burdens were significantly higher than in healthy controls. Autonomic disturbances include:
- POTS, characterized by excessive heart rate increase on standing without hypotension.
- Neurocardiogenic syncope, an aberrant reflex leading to hypotension and bradycardia.
- Orthostatic hypotension and delayed orthostatic hypotension.
- Orthostatic intolerance without overt hemodynamic changes, indicating subtler autonomic impairment.
Mechanistically, dysautonomia may reflect immune-mediated injury to small autonomic nerve fibers, persistent viral or post-viral effects on brainstem autonomic centers, or autoimmune targeting of receptors regulating cardiovascular control.
2.2 Cerebrovascular and Endothelial Dysfunction
SARS-CoV-2 infection has been linked to endothelial activation, microvascular injury, and impaired cerebral autoregulation. Although direct evidence in PASC blackout syndromes remains limited, endothelial dysfunction likely contributes to inappropriate cerebral perfusion on orthostatic stress, lowering the threshold for syncope. Furthermore, microthrombotic and inflammatory vascular changes may impair oxygen delivery to the brain.
2.3 Immune-Mediated and Autoimmune Mechanisms
Autoantibodies against autonomic receptors (e.g., adrenergic and muscarinic receptors) have been implicated in post-infectious dysautonomia, potentially disrupting autonomic tone and vascular control. These antibodies may arise as part of the post-COVID immune response, although exact prevalence and pathogenic roles require further study.
2.4 Cardiopulmonary and Deconditioning Contributions
Subclinical myocarditis, reduced stroke volume, and pulmonary vascular abnormalities have been reported in long COVID and may exacerbate orthostatic intolerance by limiting cardiac output upon positional change. Deconditioning following prolonged illness further diminishes cardiovascular reserve, compounding susceptibility to blackout episodes.
3. Physiology: Mechanisms Precipitating Blackouts
Blackouts are defined clinically as transient loss of consciousness lasting seconds to minutes due to insufficient cerebral perfusion. Normal postural changes elicit adaptive autonomic responses: baroreceptor-mediated vasoconstriction and heart rate modulation maintain blood pressure and cerebral blood flow. In PASC, disruptions in these compensatory mechanisms underpin blackout phenomena.
3.1 Baroreflex and Heart Rate Dysregulation
Baroreflex failure impairs the normal increase in sympathetic vascular tone upon standing. In POTS variants, exaggerated heart rate rise attempts to compensate for venous pooling but may inadequately sustain blood pressure and cerebral perfusion. Reduced heart rate variability and impaired parasympathetic modulation have been documented in long COVID patients with orthostatic intolerance.
3.2 Venous Pooling and Reduced Preload
Impaired vasoconstriction leads to pooling of blood in the lower extremities and splanchnic bed on upright posture, reducing venous return and preload. In the absence of adequate compensatory mechanisms, cardiac output may fall precipitously, provoking presyncope or syncope.
3.3 Cerebral Autoregulation Impairment
Cerebral blood flow is normally maintained across a range of systemic blood pressures. Dysregulated autoregulation, possibly related to endothelial dysfunction or microvascular injury, may increase vulnerability to even modest hypotensive episodes, leading to blackouts.
4. Pathology Underlying Dysautonomia and Blackouts
Post-COVID autonomic pathology encompasses both central and peripheral elements:
- Small-fiber autonomic neuropathy affecting efferent and afferent autonomic fibers.
- Brainstem neuroinflammation, potentially disrupting integrated autonomic centers.
- Persistent endothelial activation and microvascular compromise reducing vascular responsiveness.
- Autoimmune phenomena, including receptor-directed antibodies interfering with neurotransmission.
These processes reflect a multisystem pathophysiology, not confined to a single organ or pathway, and likely vary among individuals.
5. Clinical Factors Predisposing to Blackouts
5.1 Triggers of Orthostatic Stress
- Rapid transition to upright posture.
- Heat exposure and dehydration.
- Post-prandial states and prolonged standing.
- Exercise or physical exertion.
5.2 Comorbid and Demographic Risk Modifiers
Women appear disproportionately affected by PASC autonomic symptoms, mirroring patterns seen in primary POTS. Severe acute COVID, preexisting autonomic dysfunction, and connective tissue disorders may also elevate risk. Behavioral factors including deconditioning and sleep deprivation further impair autonomic resilience.
6. Clinical Phenotypes of Blackout Syndromes in Long COVID
Multiple overlapping clinical presentations are observed:
- POTS-related presyncope and syncope, marked by excessive heart rate response.
- Neurocardiogenic syncope, with reflex hypotension and bradycardia.
- Orthostatic intolerance without classic hemodynamic changes, necessitating careful assessment including continuous blood pressure and cerebral blood flow measures.
- Delayed orthostatic hypotension, with symptoms developing minutes after standing.
These phenotypes often coexist or evolve over time, complicating diagnosis and management.
7. Discussion
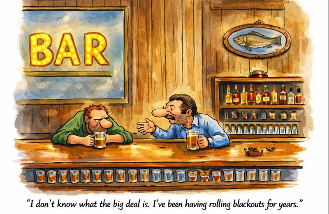
Blackout phenomena in long COVID represent a real and physiologically grounded form of autonomic and cardiovascular dysregulation, distinct from anxiety or psychogenic explanations. The existing literature demonstrates a high prevalence of orthostatic intolerance and autonomic dysfunction in long COVID cohorts, often captured by tilt table testing and active orthostatic challenges.
Limitations in current research include small sample sizes, heterogeneity of study designs, and variable use of quantitative autonomic measures. Further investigation with advanced autonomic testing, cerebral perfusion monitoring, and immunologic profiling is essential to elucidate mechanisms and guide therapeutic strategies.
8. Conclusion
Blackouts in long COVID arise from intertwined autonomic, vascular, immune, and cardiac pathophysiology. Recognizing these episodes as physiologic consequences of post-COVID dysautonomia is critical for accurate diagnosis and appropriate multidisciplinary care. Future research should focus on delineating specific mechanistic pathways, refining diagnostic criteria, and testing targeted interventions.
References
- Long COVID with high incidence of autonomic dysfunction and POTS features; prevalence and symptom burden in PASC cohorts.
- Dysautonomia patterns, heart rate variability, and orthostatic intolerance physiology in long COVID.
- Role of tilt table testing and head-up orthostatic challenges in identifying CAD in PASC.
- Pathophysiology and clinical spectrum of post-COVID autonomic dysfunction and orthostatic intolerance.
- Proposed mechanisms including indirect autoimmunity, neuroinflammation, and central autonomic disruption.